Histopathological Spectrum of Eyelid Tumors in Northeast India: A 6-Year Retrospective Study
Download
Abstract
Background: Eyelid tumors present with a diverse histopathological spectrum, varying across geographic and ethnic groups. In Asia, sebaceous gland carcinoma (SGC) often rivals basal cell carcinoma (BCC) in incidence. This study evaluates the clinicopathological profile of eyelid tumors from Northeast India.
Objective: To analyse the histopathological distribution, demographic profile, and malignant versus benign ratio of surgically excised eyelid tumours over six years at a tertiary care centre.
Methods: A retrospective review was conducted on histopathologically diagnosed eyelid tumors excised between March 2008 and February 2014. Clinical and demographic data were retrieved. Routine H&E staining was performed, with immunohistochemistry as needed. Tumours were classified according to the WHO 5th edition classification.
Results: Of 132 excised eyelid lesions, 124 were neoplastic (81.5% benign, 18.5% malignant), and 8 were inflammatory chalazia. Benign tumors included epidermal cyst (23.8%), dermoid cyst (21.8%), haemangioma (14.9%), and squamous papilloma (11.9%). Among malignancies, basal cell carcinoma (BCC) predominated (39.1%), followed by squamous cell Carcinoma (SCC) (30.4%), Sebaceous gland carcinoma (SGC) (21.7%), and malignant melanoma (8.6%). Malignant tumors showed a female preponderance. Comparative analysis with regional and global studies demonstrated higher proportions of SGC and SCC in this cohort.
Conclusion: Benign lesions remain predominant in eyelid tumors. However, sebaceous carcinoma and squamous cell carcinoma constitute a significant malignant burden in this Northeast Indian population. Early biopsy and histopathological diagnosis are essential for timely intervention.
Introduction
The eyelids are the most visible and accessible part of the eye; therefore, any mass lesion occurring in the eyelids can be detected and treated at an early stage. However, ignorance, poverty and inaccessibility to proper health care result in late diagnosis, which has adverse aesthetic side effects and may result in loss of vision [1, 2].
The eyelids contain numerous histological elements that can give rise to a host of benign and malignant lesions. Most eyelid tumours are benign, and cutaneous neoplasms are the most common. Among the malignant tumours, geographic and ethnic diversity is noted. BCC is the most common malignant eyelid tumour among Caucasians and sebaceous gland carcinoma in Asians [3].
Materials and Methods
This is a retrospective study carried out in the pathology department at the Regional Institute of Ophthalmology, Guwahati, Assam, Northeast India. The study included all cases with a histological diagnosis of eyelid tumours that were surgically removed in the Department of Ophthalmology from March 2008 to February 2014. The medical records of these patients were thoroughly studied regarding age, gender, lesion location, clinical diagnosis, and type of surgery.
Only patients who underwent surgical excision at our centre were included. Cases requiring extensive surgery, such as orbital exenteration or advanced reconstructive procedures, were referred to higher centres and excluded from the present analysis. Inflammatory lesions such as chalazia were excluded from the neoplastic analysis.
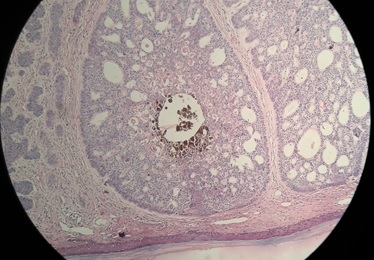
Tissue specimens were submitted to the pathology department in 10% formalin, processed and embedded in paraffin. Hematoxylin and eosin (H&E) staining was performed for all specimens. In selected cases, immunohistochemistry (IHC) was performed to aid in histopathological diagnosis. HMB-45 and S100 were used to differentiate malignant melanoma from pigmented Basal cell carcinoma (BCC), while epithelial membrane antigen (EMA) was employed to distinguish Sebaceous carcinoma from BCC with Sebaceous differentiation. All tumours were classified according to the World Health Organisation (WHO) 5th edition classification of eye tumours (Figure 1 and 2).
Figure 1. Clinical Picture Showing BCC in the Lower Lid of the Eye.

Figure 2. Low Power View of H and E Staining of Eyelid Mass Showing Adenoid Basal Cell Carcinoma .
Results
A total of 132 eyelid lesions were excised during the study period. Of these, 124 were neoplastic and 8 were inflammatory chalazia. The analysis included only the neoplastic lesions. The cohort consisted of 67 males (54%) and 57 females (46%), with ages ranging from 3 to 80 years (median: 34 years).
Benign tumours accounted for 101 of the 124 neoplastic cases (81.5%). The upper eyelid was affected in 59 (58%) of benign cases. The most common benign entities were epidermal inclusion cysts (24 cases; 23.8%), dermoid cysts (22; 21.8%), hemangiomas (15; 14.9%),
and squamous papillomas (12; 11.9%) (Table 1, 2 and 3).
| Parameter | Value |
| Total lesions excised | 132 |
| Inflammatory/reactive lesions (chalazion) | 8 (reported separately) |
| Tumours analysed | 124 |
| Gender (all tumours) | Males 67 (54%); Females 57 (46%) |
| Tumour type | Benign 101 (81.5%); Malignant 23 (18.5%) |
| Most common benign lesions | Epidermal cyst 24; Dermoid cyst 22; Haemangioma 15; Squamous papilloma 12 |
| Most common malignant lesions | BCC 9; SCC 7; SGC 5; MM 2 |
| WHO category | Benign (n) | Malignant (n) |
| Cystic lesions | 52 | |
| Vascular tumours | 15 | |
| Keratinocyte tumours | 17 | 16 |
| Sebaceous gland tumours | 3 | 5 |
| Follicular adnexal tumours | 2 | |
| Melanocytic tumours | 8 | 2 |
| Peripheral nerve sheath tumours | 3 | |
| Sweat gland tumours | 1 |
| Study | Study Period | Most Common Lesion | 2nd Most Common | 3rd Most Common |
| Present Study – India | 2008–2014 | Epidermal cyst | Dermoid cyst | Haemangioma |
| Krishnamurthy H et al., India [4] | 2002–2011 | Epidermal cyst | Nevus | Dermoid cyst |
| Çakici O et al., Türkiye [5] | 2016–2020 | Xanthelasma | Squamous papilloma | Chalazion |
| Huang Y et al., China [6] | 1995–2015 | Intradermal nevus | Seborrhoeic keratosis | Xanthelasma |
| Chang CH et al., Taiwan [7] | 1994–1998 | Nevus | Squamous papilloma | Inclusion cyst |
Malignant lesions comprised 23 cases (18.5%). Basal cell carcinoma (BCC) was the most common malignancy, accounting for 9 cases (39.1%), followed by squamous cell carcinoma (SCC) with 7 cases (30.4%), sebaceous gland carcinoma (SGC) with 5 cases (21.7%), and malignant melanoma with 2 cases (8.6%).
A chi-square test of independence was conducted to evaluate the association between patient gender and type of malignant eyelid tumor (Table 4).
| Sex | BCC | SCC | SGC | MM | TOTAL |
| Male | 3 | 3 | 1 | - | 7 |
| Female | 6 | 4 | 4 | 2 | 16 |
| Total | 9 | 7 | 5 | 2 | 23 |
The result was not statistically significant (χ² = 1.68, df = 3, p = 0.642), indicating that the distribution of tumor types did not significantly differ between male and female patients.
Similarly, a chi-square test was applied to assess the relationship between tumor type and eyelid location (upper vs lower lid) (Table 5).
| Lid location | BCC | SCC | SGC | MM | TOTAL |
| Upper | 2 | 4 | 4 | 2 | 12 |
| Lower | 7 | 3 | 1 | 0 | 11 |
| Total | 9 | 7 | 5 | 2 | 23 |
While the test yielded a higher chi-square value (χ² = 6.69, df = 3), the result was not statistically significant at the conventional 0.05 level (p = 0.082).
Among 23 malignant eyelid tumors, all cases had negative surgical margins with cut margin distances ranging from 0.4 to 0.8 cm. Perineural invasion (PNI) was observed in 1 case of squamous cell carcinoma (SCC), while lymphovascular invasion (LVI) was seen in 1 SCC and one malignant melanoma (MM). No PNI or LVI was identified in basal cell carcinoma (BCC) or sebaceous gland carcinoma (SGC). Overall, high-risk histopathological features were infrequent and limited to SCC and MM (Table 6 and 7).
| Histopathological Diagnosis | Total Number of cases | Nearest cut margin distance from tumour | Perineural Invasion (PNI) | Lymphovascular Invasion (LVI) |
| Basal Cell Carcinoma (BCC) | 9 | 0.5 cm | Not seen | Not seen |
| 0.5 cm | Not seen | Not seen | ||
| 0.5 cm | Not seen | Not seen | ||
| 0.4 cm | Not seen | Not seen | ||
| 0.6 cm | Not seen | Not seen | ||
| 0.5 cm | Not seen | Not seen | ||
| 0.5 cm | Not seen | Not seen | ||
| 0.6 cm | Not seen | Not seen | ||
| 0.5 cm | Not seen | Not seen | ||
| Squamous Cell Carcinoma (SCC) | 7 | 0.6 cm | Not seen | Not seen |
| 0.5 cm | Seen | Not seen | ||
| 0.4 cm | Not seen | Not seen | ||
| 0.5 cm | Not seen | Not seen | ||
| 0.7 cm | Not seen | Not seen | ||
| 0.5 cm | Not seen | Seen | ||
| 0.6 cm | Not seen | Not seen | ||
| Sebaceous Gland Carcinoma (SGC) | 5 | 0.6 cm | Not seen | Not seen |
| 0.5 cm | Not seen | Not seen | ||
| 0.4 cm | Not seen | Not seen | ||
| 0.5 cm | Not seen | Not seen | ||
| 0.6 cm | Not seen | Not seen | ||
| Malignant Melanoma (MM) | 2 | 0.8 cm | Not seen | Not seen |
| 0.5 cm | Not seen | Seen |
| Study | BCC (%) | SCC (%) | SGC (%) | MM (%) |
| Present Study | 39.1 | 30.4 | 21.7 | 8.6 |
| Wang L et al., China (2021) [8] | 48.7 | 12.4 | 34.2 | 2.9 |
| Nguyen NH, Vietnam (2025) [9] | 46 | 31 | 15 | 8 |
| Kiran Kumar BR, India (2024) [10] | 50 | 30 | 10 | 10 |
| Wu Y et al., China (2025) [11] | 74.3 | 7.1 | 11.4 | 2.1 |
| Kaliki S et al., India (2015) [12] | 24 | 18 | 53 | – |
Discussion
In our study, benign tumours accounted for the majority of eyelid lesions, 101 out of 124 (81.4%). This is consistent with most authors, both in India and other Southeast Asian countries [7, 8]. Recent studies provide valuable insights into the evolving epidemiology of eyelid tumours worldwide. Our study showed 18.5% malignant cases, which aligns with several recent Asian studies. The Turkish study (2018–2023) reported a slightly higher malignancy rate (24.2%) [5], whereas Wang et al. (China, 2000–2018) reported a rate of 14.9% [8]. The Vietnamese study reported a 12.5% rate of malignant cases [9]. In contrast, a study by Gundogan et al. Al, the percentage of malignant cases was only 1.5% [13].
Histologic distribution varies internationally. In our series, BCC accounted for 39.1% of malignancies, while SCC and SGC represented 30.4% and 21.7%, respectively. Comparative data reveal interesting trends: in Turkey (2025), BCC comprised 82% of eyelid cancers [5], and Wu et al. (China, 2025) reported 74.3% BCC [11]. Wang et al. (China, 2021) found BCC at 48.7% [8], Belaid A et al. in a study from Tunisia found a significantly higher proportion of BCC in 81.5% cases [14]. In comparison, our cohort displays a notably higher proportion of SCC and SGC, emphasising regional diversity.
Crucially, several Indian studies published after 2005 also reflect dominant SGC prevalence:
Kaliki et al. (2015) reported that among 191 Indian SGC cases, SGC was the most frequent malignant subtype in eyelid lesions [12]. Their 2019 study of 536 malignant eyelid tumours found SGC in 53%, versus BCC (24%) and SCC (18%) [15]. A multicenter Indian study conducted around 2019 reported 42.6% SGC and 36.4% BCC [16]. In a study by Kiran BR et al., the proportion of involvement of the lower eyelid was significantly higher than that of the upper eyelid in basal cell carcinoma (P = 0.045) [10]. In our study, there is a trend toward statistical significance, suggesting an association between BCC and lid location (p = 0.060), with BCC more commonly observed in the lower eyelid . However, the result does not reach conventional significance (p < 0.05).
A larger sample size may help clarify this relationship.
These figures align with our findings; SGC constitutes a significant proportion of eyelid malignancies in Indian cohorts (21.7%), although it often does not exceed half, as seen in larger tertiary studies. Conversely, BCC and SCC remain substantial but less prominent relative to SGC.
This study has several limitations. The number of malignant cases was relatively small (n = 23), reflecting the nature of our institution as a regional ophthalmology referral centre rather than a dedicated oncology facility. Consequently, patients requiring extensive surgical interventions, neoadjuvant chemotherapy, or adjuvant treatment were referred to tertiary oncology centres, contributing to the underrepresentation of advanced malignancies. Being a single-institutional study, the findings may not be generalizable to broader populations. The study was cross-sectional and focused on clinicopathological correlation; hence, longitudinal data regarding recurrence, survival, and treatment outcomes were not available.
Thus, our findings contribute important regional data while broadly aligning with emerging global trends. The persistent burden of SGC in our series underscores the need for clinician awareness and early histopathologic evaluation, particularly in Asian populations.
Acknowledgements
We thank Dr. Deepli Deka, Ex-Director, Department of Ophthalmology, Regional Institute of Ophthalmology, Guwahati, for their support in the completion of the study. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for- profit sectors. The authors declare that they have no conflict of interest.
References
- Eyelid, conjunctival, and orbital tumours: an atlas and textbook Shields JA , Shields CL. . Philadelphia: Wolters Kluwer..
- Tumours of the eyelids in Indians Aurora AL . Indian J Ophthalmol.1965;13(3):91-8.
- Sebaceous cell carcinoma of the ocular adnexa Ni C, NSearl SS , Kuo PK , Chu FR . Surv Ophthalmol.1982;26(1):27-36.
- Pattern of benign eyelid lesions in a South Indian population: A histopathological study Krishnamurthy H, et al . Indian J Pathol Microbiol. 2011;54(3):482–485..2011;54(3).
- Malignant eyelid tumours: a tertiary centre experience from Turkey Çakici O, et al . International Journal of Ophthalmology.2020;13(8):1287-1293. CrossRef
- A retrospective review of benign eyelid tumours in a Chinese population Huang Y, et al . Chin Med J.2016;129(24):2933-2937.
- Eyelid Lesions in Taiwan: A Clinicopathological Study Chang CH , et al . Taiwan J Ophthalmol.1998;2(2):35-39.
- Clinicopathological analysis of 5146 eyelid tumours and tumour-like lesions in an eye centre in South China, 2000-2018: a retrospective cohort study Wang L, Shan Y, Dai X, You N, Shao J, Pan X, Gao T, Ye J. BMJ open.2021;11(1). CrossRef
- The correlation of clinical and histopathological features of eyelid malignancies: a 5-year retrospective study in Vietnam Nguyen N, Nguyen M, Mai HK , Do ST , Pham VH , Vuong DTP , Maturi JR , et al . International Ophthalmology.2025;45(1). CrossRef
- Eyelid Tumours: An Institutional Experience on Clinicopathological Profile and Management Br KK , S A, Narayanan GS . Asian Pacific Journal of Cancer Biology.2024;9(2). CrossRef
- Clinicopathologic features and new factors affecting constitution of eyelid neoplasms: a 10-year multicentre experience in southern coastal China Wu Y, Zhong H, Xiang Z, Zhou P, Wang H, Song X, Li Y. Canadian Journal of Ophthalmology.2025;60(2). CrossRef
- Sebaceous gland carcinoma of the eyelid: clinicopathological features and outcome in Asian Indians Kaliki S, Ayyar A, Dave T V, Ali M J, Mishra D K, Naik M N. Eye.2015;29(7). CrossRef
- Eyelid tumors: clinical data from an eye center in Ankara, Turkey Gundogan FC , Yolcu U, Tas A, Sahin OF , Uzun S, Cermik H, Ozaydin S, et al . Asian Pacific journal of cancer prevention: APJCP.2015;16(10). CrossRef
- Radiation Therapy for Primary Eyelid Cancers in Tunisia Belaid A., Nasr C., Benna M., Cherif A., Jmour O., Bouguila H., Benna F.. Asian Pacific journal of cancer prevention: APJCP.2016;17(7).
- Malignant eyelid tumours: Experience from a tertiary eye care centre in India Kaliki S, et al . Ocul Oncol Pathol.2019;5(3):210-219.
- Epidemiological pattern of eyelid malignancies: A multicenter Indian analysis Sudhir RR , et al . Indian J Ophthalmol.2019;67(5):580-685.
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2025
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times