A Rare Case of a 30-Gram Giant Parathyroid Adenoma Detected by 99mTc-Sestamibi Scintigraphy and Presenting with Pathological Fracture
Download
Abstract
Background: A giant parathyroid adenoma (GPA) is a very rare, benign (non-cancerous) tumor of the parathyroid gland that is significantly larger than a typical parathyroid adenoma, typically weighing more than 3.5 gram. These primarily present not only hyperparathyroidism but also have severe clinical presentations like high serum calcium, alkaline phosphatase and cause significantly severe osteoporosis. These topographies are totally unlike from malignant parathyroid cancer.
Case Presentation: We present here an interesting case and clinical course of a 55 years female patient with GPA. Patient initially came with pain in left leg along with trouble in walking and was afterward diagnosed to have fracture of neck of left femur and reported with high serum calcium and alkaline phosphatase level. On assessment, the patient was found to have hyper parathyroidism with severe hypercalcemia and osteoporosis. Parathyroid Scintigraphy which procedure includes 99mTcO4- Thyroid Scan followed with 99mTc-sestamibi Parathyroid Scan showed tracer localization to inferior aspect of lower lobe of right thyroid gland suggestive of Parathyroid Adenoma. USG neck revealed large multilobulated hypoechoic mass with retro-tracheal extension displacing trachea anterolaterally and esophagus laterally to left side suggestive as parathyroid adenoma. She underwent right inferior parathyroidectomy and a giant parathyroid adenoma (GPA) weighing 30 gram measuring 6.4x3.8x2.2 cm was excised. Histology confirmed parathyroid adenoma with mostly chief cell type. The tumor excision resulted not only substantial decline in PTH levels but also decrease serum calcium and alkaline phosphatase level. She developed severe hungry bone syndrome (HBS) in post operative period. She was treated aggressively for HBS with intravenous calcium gluconate, oral calcium supplements along with calcitriol.
Conclusion: GPA present as distinct clinical entity with features different from both parathyroid adenoma and parathyroid carcinoma. We strongly recommend the use of 99mTc-Sestamibi parathyroid scintigraphy as a useful and safe examination technique for the diagnosis of parathyroid adenomas.
Introduction
The parathyroid glands are two pairs, which are situated behind the thyroid gland and it’s weighing about 60 milligrams (mg). Each gland is a yellowish- brown flat ovoid that resembles a lentil seed, usually about 6 mm long and 3 to 4 mm wide, and 1 to 2 mm antero-posteriorly [1]. The parathyroid hormone (PTH), which is secreted by these glands, is a crucial modulator of calcium metabolism. The most frequent cause of hyperparathyroidism and hypercalcemia is parathyroid adenomas and the majority of parathyroid adenomas weigh less than 1 gram [2]. Parathyroid adenoma which is more than 3.5 gram is presented as a giant parathyroid adenoma (GPA) [3]. GPA differs from normal pituitary adenomas in both clinical and biochemical characteristics, making it a clinically unique entity. GPAs typically exhibit clinical symptoms and share many characteristics with parathyroid carcinomas.
The characteristics that set GPA and parathyroid carcinomas apart are crucial since both illnesses require separate surgical and medicinal approaches to treatment. Understanding these characteristics is crucial since patients with GPA have a unique clinical trajectory and are more susceptible to problems following surgery. 99mTc-Sestamibi scintigraphy is the gold standard imaging technique of choice for the diagnosis of parathyroid adenomas because of high sensitivity.
We present a clinical case of 55 years old female patient with giant parathyroid adenoma (GPA), emphasizing the patients’ diagnosis (99mTc-Sestamibi Scan) post-operative care, test results, and clinical outcome.
Case Report
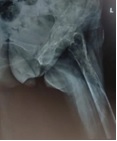
A 55 years old woman came with pain in left leg along with difficulty in walking. After then patient was admitted to orthopedic ward for further evaluation. The patient was found to have pathological fracture of neck of left femur (Figure 1) and severe hypercalcemia with high alkaline phosphatase.
Figure 1. Left Femur X-ray Showing the Left Femoral Neck Fracture with Osteoporosis.
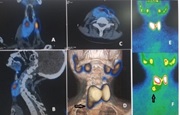
Detailed history revealed that patient had symptom associated with hypercalcemia like constipation, nausea, vomiting, musculoskeletal pains and sometimes pain abdomen. Biochemical 4 parameters showed parathyroid hormone (PTH) dependent hypercalcemia with serum calcium of 15.8 mg/dl, serum alkaline phosphatase of 1201 units/l and serum PTH level of 1750.7 Pg/ml. Her thyroid function tests FT3, FT4 and TSH was respectively 2.8 Pg/mL, 1.3 ng/dl and 5.47 µIU/mL which was normal in range. Her other routine blood tests were within normal limits except Vitamin D which was 20.1 ng/mL (slightly insufficient). Parathyroid Scintigraphy procedure was performed as subtraction technique protocol in which 99mTcO - Thyroid Scan followed with 99mTc-Sestamibi Parathyroid Scan revealed tracer localization to inferior aspect of lower lobe of right thyroid gland suggestive of Parathyroid Adenoma (Figure 2).
Figure 2. 99mTc-Thyroid Scan (5 mCi) Followed by (20 minute later) 99mTc-Sestamibi (20mCi) Parathyroid Scan Showing Normal Radiotracer Uptake in the Thyroid Bed During Thyroid Scan (E) and Radiotracer Uptake in Parathyroid Adenoma just Lower Pole of the Right Thyroid Lobe (F). The coronal (A), Sagittal (B), Axial (C) and 3D image (D) of SPECT/CT Images of parathyroid adenoma were shown in above figure.
Ultrasonography (USG) abdomen revealed that increased right renal parenchymal echogenicity with maintained corticomedullary differentiation (CMD) whereas increased left renal parenchymal echogenicity with loss of CMD with moderate hydronephrosis with cortical thinning and bilateral nephrolithiasis. On examination she feels palpable neck mass. USG neck revealed large multilobulated hypoechoic mass with retro-tracheal extension displacing trachea anterolaterally and esophagus laterally to left side suggestive as parathyroid adenoma. After then which patient underwent for right inferior parathyroidectomy (surgery). A giant parathyroid adenoma was excised weighing 30 gram measuring 6.4x3.8x2.2 cm (Figure 3).
Figure 3. Macroscopical View of Resected Right Inferior Parathyroid Adenoma Measuring 6.4x3.8x2.2 cm.

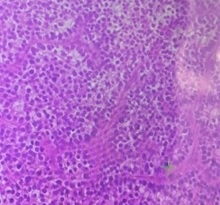
Intra operative period was monotonous. Histology confirmed parathyroid adenoma with mainly chief type cells (Figure 4).
Figure 4. Histopathology Found Mainly Chief Cells Type Suggestive of Parathyroid Adenoma.
Postoperatively, the patient developed hungry bone syndrome (HBS) which was managed by intravenous calcium gluconate infusions, along with oral calcium and calcitriol supplementation. After the surgery, there was sudden drop in PTH levels to 9.8 Pg/ml as well as serum calcium and phosphate became 8.6 mg/dl and 1.5 mg/dl respectively. Subsequently, the patient was shifted to oral calcium supplements and was discharged on oral vitamin D and calcium supplements. All detailed regarding case presentation (our patient) are summarized in Table 1.
| Characteristics of GPA and Index case | ||
| Age | 55 | |
| Sex | Female | |
| Location | ||
| Thyroidal | Thyroidal (right) | |
| Mediastinal extension | Displaced trachea and esophagus | |
| Presentation | ||
| Fracture | Present | |
| Renal stones | Present | |
| Neck swelling | Present | |
| GPA Weight | 30 grams | |
| Investigations | ||
| Laboratory Tests | Pre-operative | Post-operative |
| Serum calcium | 15.8mg/dl | 8.6 mg/dl |
| Serum PTH | 1750.7pg/ml | 9.8 Pg/ml |
| Complications | Hungry bone syndrome |
Giant parathyroid adenoma is very erratic and very difficult to differentiate as benign tumors of parathyroid gland. Preoperative differentiation between giant parathyroid adenoma (GPA) and parathyroid carcinoma may be thought-provoking, as they both may present as a large parathyroid tumor with hyperparathyroidism. Differentiating GPA from parathyroid carcinoma is significant as it determines the subsequent surgical intervention.
Discussion
Hyperparathyroidism is a predominant endocrine disease demarcated by insistent hypercalcemia and high PHT levels [4]. Research studies concluded that a yearly prevalence of about 21 cases per 100,000 people, and 85% of these cases are caused by a parathyroid adenoma [5]. There are limited occurrences of GPA have previously been pragmatic since it is a rare cause of PTH [6]. In some cases, there is only elevation of parathyroid hormone with normalized serum calcium and alkaline phosphates level. In these cases, there is less chance of osteoporosis with chances of bone fractures. This disorder is classified as normocalcemic hyperparathyroidism to differentiate it from secondary hyperparathyroidism [7]. Those patients whose serum calcium and alkaline phosphatase levels are high, should be closely monitored before and after surgery because the non-pathological parathyroid glands stopover working generally due to a feedback rejoinder. There is a normal phenomenon of transient hypocalcemia after surgery of parathyroid adenoma due to a severe reduction in calcium levels [8]. In this case study, patient was diagnosed with giant parathyroid adenoma with elevated parathyroid hormone, serum calcium and serum phosphate level. The measurement of PTH level was totally normal range after 24 hours of surgery and calcium and phosphate levels was also normal. This study revealed that elevation of PTH level, serum calcium, serum phosphatase and osteoporosis with neck of femur was caused by abnormal function of the three nonpathological parathyroid glands before surgery.
There are number of imaging modalities which can primarily use for preoperative management of giant parathyroid adenoma and localization of the pathologic glands, even though the diagnosis of GPA is established by clinical and laboratory criteria. Research studies concluded that preoperative neck ultrasonography scan can locate the parathyroid gland with a sensitivity and specificity of around 85% and 75%, respectively. The sensitivity, specificity, positive predictive, and negative predictive values of 99mTc-Sestamibi Parathyroid scintigraphy for locating primary lesions were 91%, 99%, 96%, and 97% respectively; and for secondary lesions corresponding figures were 74%, 84%, 93%, and 54%. The corresponding overall results for all lesions were 79%, 95%, 94%, and 82% [9]. There is a comparative study done by Reza Nafisi Moghadam et al concluded that there were no significant differences between the two methods in terms of sensitivity and specificity [10]. There were overlaps in 99% confidence intervals. Also features of the two methods are similar. Accuracy SPECT/CT is even better than what presented in literature because above literature was based on SPECT only. Giant parathyroid adenomas are seen in smaller cases of primary parathyroidism, and there is a challenge with the definition of GPA regarding their weight. There is a report of patient with GPA weight more than 220 g [11], whereas it is described large parathyroid adenomas as having a weight greater than 3.5 g [3]. There are lots of factors which may help to differentiate GPA and parathyroid carcinoma. The differential diagnosis and rationale for diagnosis (adenoma vs carcinoma) are adequately explained by Satrudhan Pd Gupta et al and concluded that the biomarker urine (human chorionic gonadotropin (HCG) in urine has the capability to differentiate between parathyroid adenomas and carcinomas and this has probable to become a marker of disease progression in malignant parathyroid tumor [12].
In our case report, parathyroid adenoma measuring a 6.4x3.8x2.2 cm which weight was 30 gram was excised. Primary hyperparathyroidism is accomplished surgically by removing the pathologic parathyroid tissue, whether it is through locally invasive parathyroidectomy [13].
In our case report, there is not only elevation of parathyroid hormone but also hypercalcemia, osteoporosis, renal calcifications so parathyroidectomy is suggested as a last option for treating parathyroid adenoma. This procedure purposes to find four parathyroid glands by accessing the thyroid gland and, according to its size, cutting and removing the abnormal ones. A solitary overactive parathyroid gland is removed using a minimally invasive procedure in a minimal-invasive parathyroidectomy [14]. This case report is very rare and even first reported case in Nepal showed that a hyper functional large parathyroid adenoma in an old patient might have a very high PTH level and a history of pathologic fracture, which might be difficult to diagnose and manage.
In conclusion, GPA present as distinct clinical disease with characteristics different from both parathyroid adenoma and parathyroid carcinoma. The severity of symptoms, high serum calcium level, higher PTH level and ultrasonography (USG) of neck characteristics are vital aspects in discriminating GPA prior to surgery. Although, 99mTc-sestamibi Parathyroid scintigraphy with SPECT/CT is the gold standard imaging technique of choice for the diagnosis of giant parathyroid adenomas because of high sensitivity, specificity and accuracy.
Funding source
No funding was obtained during the study.
Patient consent
A written consent was obtained from patient during the study, that the work can be published without exposing the patient details.
Declaration of competing interest
The authors declare there is no conflict of interest among themselves.
References
- Williams, Peter L; Warwick, Roger (eds.). Gray's Anatomy (36th ed.). Churchill Livingstone Gray, Henry . 1980;:p. 1453. ISBN 0-443-01505-8.
- Clinicopathologic and therapeutic aspects of giant parathyroid adenomas - three case reports and short review of the literature Neagoe RM , Sala DT , Borda A, Mogoantă CA , Műhlfay G. Romanian Journal of Morphology and Embryology = Revue Roumaine De Morphologie Et Embryologie.2014;55(2 Suppl).
- Do giant parathyroid adenomas represent a distinct clinical entity? Spanheimer PM , Stoltze AJ , Howe JR , Sugg SL , Lal G, Weigel RJ . Surgery.2013;154(4). CrossRef
- Primary hyperparathyroidism Madkhali T, Alhefdhi A, Chen H, Elfenbein D. Ulusal Cerrahi Dergisi.2016;32(1). CrossRef
- Giant cystic parathyroid adenoma: two case reports and a literature review Weng J, Zhou W, Feng Y. The Journal of International Medical Research.2022;50(6). CrossRef
- Giant Parathyroid Tumor: Parathyroid Adenoma versus Parathyroid Carcinoma Gossili F, Carlé A, Andersen TB , Zacho HD . Case Reports in Endocrinology.2022;2022. CrossRef
- Normocalcemic Parathyroid Adenoma with Brown's Tumor Maxilla: A Rare Case Wadhawan A, Arora N, Goel A, Kumar P, Jangra P, Gupta A. Iranian Journal of Otorhinolaryngology.2023;35(126). CrossRef
- Primary hyperparathyroid-ism. In: das Neves MC, Santos RO, Ohe MN eds. StatPearls[Internet] Pokhrel B, Leslie SW , Levine SN . 2022;Vol 66. StatPearls Publishing:678-688.13.
- Parathyroid Scintigraphy in Primary and Secondary Hyperparathyroidism: Accuracy of Preoperative Localisation Using Combined Imaging Techniques HT Tam , YH Wong , SK Cheung, , WT Ngai , PT Choi . Hong Kong J Radiol.2010;13:59-67.
- Comparative Diagnostic Performance of Ultrasonography and 99mTc-Sestamibi Scintigraphy for Parathyroid Adenoma in Primary Hyperparathyroidism; Systematic Review and Meta- Analysis Nafisi Moghadam R, Amlelshahbaz AP , Namiranian N, Sobhan-Ardekani M, Emami-Meybodi M, Dehghan A, Rahmanian M, Razavi-Ratki SK . Asian Pacific journal of cancer prevention: APJCP.2017;18(12). CrossRef
- A Migratory Mishap: Giant Mediastinal Parathyroid Adenoma Garuna Murthee K, Tay WL , Soo KL , Swee DS . The American Journal of Medicine.2018;131(5). CrossRef
- Significance of HCG to distinguish parathyroid carcinoma from benign disease and in adding prognostic information: a hospital based study from Nepal Gupta SP , Mittal A, Sathian B. Asian Pacific journal of cancer prevention: APJCP.2013;14(1). CrossRef
- Atypical parathyroid adenoma: A case report Besrour C, Rojbi I, Mchirgui N, Ben Nacef I, Khiari K. Clinical Case Reports.2022;10(12). CrossRef
- Surgical treatment of primary hyperparathyroidism: from bilateral neck exploration to minimally invasive surgery Pelizzo M. R., Pagetta C., Piotto A., Sorgato N., Merante Boschin I., Toniato A., Grassetto G., Rubello D.. Minerva Endocrinologica.2008;33(2).
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2025
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times