Fibre Proportion in Oral Nutritional Supplements on Diarrhea Management in Cancer Patients: A Case Study
Download
Abstract
Background and purpose: Diarrhea is a common side effect in cancer patients, especially during chemotherapy or antibiotic treatment. Managing this symptom is important for patient comfort, hydration, and nutritional status. Fibre, an important component of many oral nutritional supplements (ONS) formulations, has been shown to influence bowel function, including diarrhea. This case study examines the role of fibre proportion in ONS for managing diarrhea in two cancer patients undergoing treatment.
Case presentation: Both patients initially experienced persistent diarrhea despite switching to fibre-based ONS. Upon transitioning to an ONS with an equal ratio of soluble to insoluble fibre, both patients showed improved stool consistency and bowel open frequencies with optimal energy and protein intake.
Discussion: The proportion of soluble to insoluble fibre in ONS may play a crucial role in managing diarrhea among cancer patients. While achieving adequate total fibre intake is important, healthcare providers may need to consider not just the quantity but also the quality and proportion of fibre in nutritional interventions. Soluble fibre-enriched ONS may offer benefits for reducing diarrhea, while high insoluble fibre content could aggravate the condition.
Conclusion: A careful consideration of the types and proportions of fibre may be necessary for optimal symptom management. A tailored approach that accounts for the patient’s specific needs is essential in optimizing nutritional care and improving quality of life.
Introduction
Diarrhea during enteral nutrition is a common complication. Diarrhea is a condition characterized by loose, watery stools, usually occurring three or more times a day. It has been reported that the incidence of diarrhea was 2% - 95% in enteral feeding cases [1, 2]. Ongoing chemotherapy treatment, particularly chemotherapy like FOLFIRI (irinotecan) and 5-fluorouracil (5-FU®), is associated with high rates of chemotherapy-induced diarrhea (CID), reaching up to 80% [2]. The use of antibiotics may worsen a compromised intestinal lining and increase the risk of diarrhea [2]. Unresolved diarrhea can cause treatment disruption, substantial psychosocial distress and impact quality of life (QoL) [3]. It can lead to dehydration, malnutrition, and a significant decrease in QoL for patients [3]. Pharmacological and non-pharmacological treatments currently used, including loperamide, probiotics, or octreotide, are often ineffective and have little impact on outcomes [2]. Managing diarrhea effectively is crucial for maintaining nutritional status and ensuring the continuity of cancer treatment.
Fibre supplementation has been shown to offer potential benefits in managing diarrhea, especially in patients receiving enteral nutrition [4]. Therefore, dietary fibre supplementation is recommended to normalise bowel function, enhance feeding tolerance, and reduce diarrhea in patients on enteral nutrition [1]. According to a meta- analysis by Kaewdech et al. [4], fibre-supplemented enteral nutrition particularly partially hydrolysed guar gum (PHGG) and mixed soluble or insoluble fibre can help alleviate diarrhea [5]. However, the optimal type and proportion of fibre for managing diarrhea in cancer patients remain unclear. This case study aims to explore the role of fibre proportion in oral nutritional supplements on diarrhea management in two cancer patients with different primary diagnoses and treatment regimens.
Case Presentations
Case 1: Mr. A was a 69-year-old male diagnosed with rectal cancer, weighed 39kg and had a height of 1.6m, with a BMI of 15.2kg/m²(underweight). His adjusted weight was 44kg. Laboratory tests revealed a low Absolute Neutrophil Count (ANC) of 0.27 x 109/L and a low albumin level of 20g/L. Based on Subjective Global Assessment (SGA) C, Mr. A is severely malnourished. Mr. A’s daily energy requirements were calculated to be 1320- 1540 kcal (30-35 kcal/kg/day), while his protein needs were estimated at 52.8-66 g per day (1.2-1.5 g/kg/day). He was undergoing chemotherapy with irinotecan when he developed watery stoma output, indicative of diarrhea, on Day 7 post cycle 1 of chemotherapy. He also developed febrile neutropenia, leading to the initiation of antibiotic therapy (cefepime) on Day 2 of diarrhea onset. Two types of anti-diarrhea medication (Lomotil and Loperamide) were initiated to manage his symptoms before ONS change. The diarrhea episode remained unchanges even anti-diarrhea medication prescribed. Mr. His diet changed to low residue mixed porridge, supplemented with a standard oral nutrition supplement (ONS), and the estimated intake was 56.7% of his energy and protein requirements. But he still presented with Type 7 diarrhea according to the Bristol Stool Chart, occurring 4-5 times per day. After that the standard ONS was changed to the 50:50 proportion of fibre-enriched ONS. The diarrhea was improved.
Case 2: Mr. B was a 46-year-old male diagnosed with nasopharyngeal cancer and underlying diabetes, weighed 63.6 kg and had a height of 1.6 m, resulting in a BMI of 24.8 kg/m², which falls within the normal weight range. His ANC was normal at 5.14 x 109/L, and his albumin level was also within the normal range at 41 g/L. Mr. B was assessed as SGA B, indicating moderate malnutrition.
Mr. B’s daily energy requirements were calculated to be 2094-2443 kcal (30-35 kcal/kg/day), while his protein needs were estimated at 84-105 g per day (1.2-1.5 g/kg/ day). He developed fever while undergoing concurrent chemo-radiotherapy (23rd out of 35 fractions, Cisplatin regimen). Diarrhea onset occurred after Day 1 of antibiotic therapy (cefepime) initiation. He was initially on a diabetic ONS and diabetic low residue diet. He experienced dysphagia and taste alterations, affecting his dietary intake. Mr. B presented with Bristol Stool Chart Type 7 diarrhea, occurring 3-4 times per day. One type of anti-diarrhea medication (Loperamide) was initiated to manage his symptoms before ONS change. However, the diarrhea episode remain unchanged. Hence, he was prescribed with the 50:50 proportion of fibre-enriched ONS and diabetic low residue diet. The diarrhea episode was improved and blood glucose remained well controlled throughout the ONS adjustment.
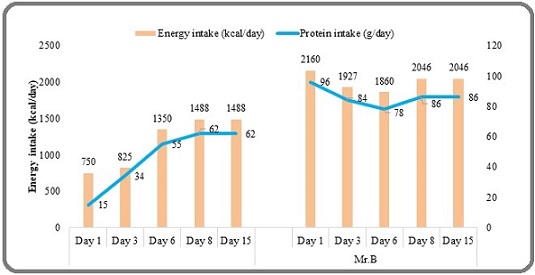
Primarily, both patients were initially switched from their standard or diabetic ONS to a fibre-based ONS when diarrhea occurred. However, both continued to experience watery stools for several days despite this intervention. Following persistent diarrhea, both patients were transitioned to an ONS with an equal ratio of soluble to insoluble fibre. The difference between the ONS was the proportion of fibre. Fibre-based ONS had 33% soluble fibre, while equal fibre ratio ONS had 50% soluble fibre. Both ONS contained a mixture of various types of soluble fibre (FOS, inulin, and gum fibre) and insoluble fibre (wheat, citrus, and oat fibre). Both patients achieved the Recommended Nutrient Intake (RNI) of over 20g of total fibre per day with both types of ONS. Both patients initially experienced persistent diarrhea despite switching to a fibre-based (33% soluble and 67% insoluble fibre) ONS. However, upon transitioning to an ONS with an equal ratio of soluble to insoluble fibre (50% soluble and 50% insoluble fibre), both patients showed marked improvement in stool consistency, frequency and total bowel output amount (Figure 1), fibre intake (Figure 2) as well as the total daily energy protein intake (Figure 3).
Figure 1. Bristol Stool Chart and Total Bowel Output.
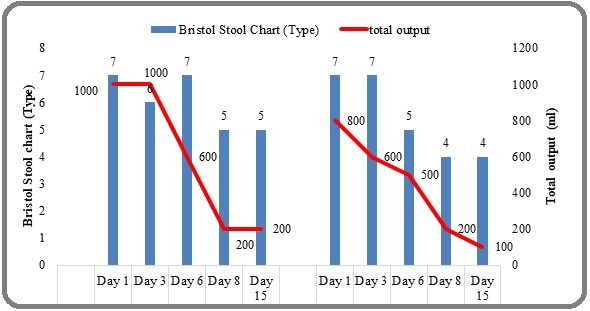
Figure 2. Total Fibre Intake and Fibre Proportion.
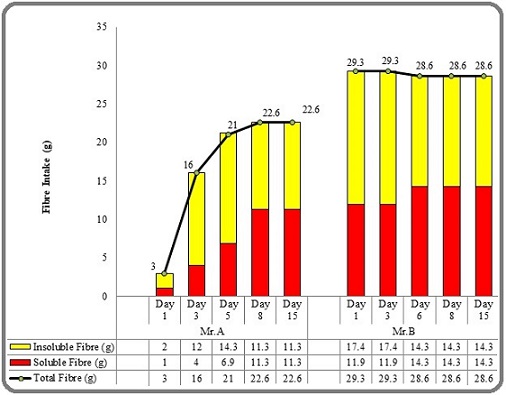
Figure 3. Total Daily Energy and Protein Intake.
Discussion
Chemotherapy is widely known to hurt the host microbiota, altering the microbial community of the gastrointestinal tract in significant and frequently long- lasting ways and resulting in diarrhea [6]. In addition, antibiotics might also induce diarrhea because they disrupt the natural balance of bacteria in the gut. While antibiotics are designed to kill harmful bacteria, they also eliminate beneficial bacteria that help regulate digestion and maintain a healthy intestinal environment. Cancer patients are particularly vulnerable to this effect due to their weakened immune systems and frequent antibiotic use to combat infections during treatment [1, 7]. Persistent diarrhea can lead to malabsorption and dehydration, compromising nutritional intake even when patients meet their caloric and protein goals [8]. The impact includes dehydration, nutrient malabsorption, and increased risk of severe gastrointestinal infections, which can worsen overall health, delay cancer treatments, and further reduce the patient’s QoL [1, 9]. Moreover, cancer treatment may need to be withheld or its dosage lowered, which could have an impact on the overall effectiveness of the treatment [1].
The improvement in diarrhea management also has positive implications for the patients’ overall nutritional status. Moreover, the resolution of diarrhea can significantly impact patients’ QoL during cancer treatment. Frequent bowel movements and associated fatigue can be mentally exhausting for patients, potentially affecting their ability to adhere to treatment regimens [3]. By improving symptom management, the fibre intervention may have indirectly supported the patients’ overall cancer treatment. It’s important to note that while both patients achieved the RNI of over 20g of total fibre per day with both types of ONS, the equal fibre ratio ONS was more effective in diarrhea management. This suggests that the proportion of fibre types may be as crucial as the total fibre content in managing diarrhea among cancer patients. By effectively managing diarrhea, the equal fibre ratio ONS likely improved nutrient absorption and hydration status, as shown in our case study.
The case report showed that the proportion of fibre types, specifically a 50:50 ratio of soluble to insoluble fibre, was the key intervention that improved diarrhea symptoms. While the patients initially received a standard fibre-based ONS and continued to experience watery stools, their condition improved only after the switch to an ONS with an equal ratio of soluble to insoluble fibre [4, 7]. This highlights a crucial distinction, as both ONS types provided adequate total fibre, suggesting that the quality and proportion of fibre are as critical as the total quantity for optimal symptom management [4, 8]. The scientific rationale behind this observation lies in the distinct properties of fibre types: soluble fibre forms a gel, helping to absorb excess water and create firmer stools, while insoluble fibre adds bulk and can accelerate bowel transit, potentially exacerbating diarrhea [4]. Additionally, the fibre supplementation may help by providing prebiotics that support the growth of beneficial gut bacteria. This case study therefore supports the hypothesis that a tailored nutritional approach, focused on the specific ratio of fibre types, is essential for improving clinical outcomes and enhancing the quality of life for cancer patients experiencing treatment-related diarrhea [4, 10]. A study evaluating fibre-enriched ONS in high ileostomy output during chemotherapy found that soluble fibre was better tolerated and more effective in reducing diarrhea compared to formulations with a higher insoluble fibre content [5]. The findings highlight the need for a nuanced approach to fibre supplementation in cancer patients experiencing treatment-related diarrhea. Merely increasing total fibre intake may not be sufficient; instead, careful consideration of the types and proportions of fibre may be necessary for optimal symptom management. These observations have important implications for clinical practice.
While our case study emphasises the importance of fibre percentage, we recognise that the cause of diarrhea in these complex cancer patients is multiple. The ONS alteration affected not only the soluble-to-insoluble fibre ratio, but also other components such as osmolarity, lipid content, and macronutrient type. However, both ONS formulations were intended to be nutritionally balanced, allowing patients to achieve adequate calorie and protein intake after the changeover. Our main finding, that an equivalent 50:50 fibre ratio was successful in alleviating symptoms where a conventional fibre ONS was not, clearly suggests that fibre proportion, rather than other macronutrient alterations, was the significant driver of clinical improvement. We recognise that more study is required to thoroughly investigate the intricate interplay between various nutritional components and fibre types in order to have a better understanding of their overall impact on diarrhoea treatment.
Strengths and Limitations
Although this case study provides valuable insights, further research is needed to establish the optimal fibre proportions for managing diarrhea in cancer patients. A targeted and gradual approach to fibre supplementation is required for patients with poor nutritional status or those who are at risk of gastrointestinal side effects in order to improve tolerance and optimise nutritional treatment. Moreover, while our case study generated excellent results, we acknowledge the significance of this cautious approach in larger clinical practice. We have also emphasised that the type of fibre used might influence tolerance, with a higher proportion of soluble fibre often being better tolerated. The patient’s blood sugar levels were stable throughout the ONS adjustment. This suggests that the switch to the 50:50 fibre ratio ONS had no significant impact on his glycaemic control. This finding is consistent with the known benefits of soluble fibre, which can help manage blood glucose levels by decreasing nutrient absorption. This inclusion enriches our case study by proving that the ONS intervention was safe and tolerable for this patient. However, we highlight the need for larger, randomized controlled trials to validate our observations and establish the optimal fibre proportions for diarrhea management in a more definitive manner especially in various cancer types and treatment regimens. Additionally, studies examining the interaction between fibre supplementation, gut microbiota, and diarrhea in cancer patients could provide deeper insights into the mechanisms underlying the observed effects. However, this case study is limited by its observational nature. The patients had different primary cancer diagnoses and treatment regimens, which could have influenced their responses to the fibre intervention. Additionally, other factors such as medications, overall diet, and individual variations in gut microbiota could have played a role in the observed outcomes.
In conclusion, this case study demonstrates that the ratio of soluble to insoluble fibre in oral nutritional supplements (ONS) can play an important role in treating diarrhoea in cancer patients. While adequate total fibre intake is critical, our findings indicate that healthcare providers should consider not only the quantity but also the quality and percentage of fibre in nutritional interventions. Specifically, soluble fiber-enriched ONS may help to reduce diarrhoea, whereas high insoluble fibre content may aggravate the illness by increasing stool frequency and fluid content. Our favourable findings in two patients after switching to an ONS with an equal ratio of soluble to insoluble fibre emphasise the importance of a personalised, patient-specific approach to nutritional therapy. This personalised strategy, which takes into consideration the exact types and quantities of fibre, is critical for improving symptom management and, ultimately, the patient’s quality of life during cancer treatment. While our findings are hypothesis- generating and merit additional exploration in larger-scale randomised controlled trials, our case study sheds light on a more nuanced approach to fibre supplementation in this vulnerable patient population.
Acknowledgements
The authors would like to thank the Director General of Health Malaysia for permission to publish this paper.
Conflict of interest
The authors declare no potential financial and non-financial conflicts of interest.
Funding source
This work did not receive any funding from public, commercial, or not-for-profit sectors.
Authors’ Contributions
Conceptualisation, methodology, MKN, CYH; formal analysis, investigation, resources, data curation, CYH and NJ; visualisation, MKN & NJ and writing original draft preparation, MKN, NJ, CYH, WHN; validation, NJ & BSMHL; writing – review and editing, MKN, CYH, WHN, BSMHL, AM, AA and NAA; and supervision, NJ and CYH. All authors read and approved the final manuscript.
References
- Formula delivery in patients receiving enteral tube feeding on general hospital wards: the impact of nasogastric extubation and diarrhea Whelan K, Hill L, Preedy VR , Judd PA , Taylor MA . Nutrition (Burbank, Los Angeles County, Calif.).2006;22(10). CrossRef
- Recommended guidelines for the treatment of cancer treatment-induced diarrhea Benson AB , Ajani JA , Catalano RB , Engelking C, Kornblau SM , Martenson JA , McCallum R, et al . Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2004;22(14). CrossRef
- Symptom distress and self-care strategies of colorectal cancer patients with diarrhea up to 3 months after surgery Pan L, Tsai Y, Chen M, Tang R, Chang C. Cancer Nursing.2011;34(1). CrossRef
- The effect of fiber supplementation on the prevention of diarrhea in hospitalized patients receiving enteral nutrition: A meta-analysis of randomized controlled trials with the GRADE assessment Kaewdech A, Sripongpun P, Wetwittayakhlang P, Churuangsuk C. Frontiers in Nutrition.2022;9. CrossRef
- Role of partial hydrolysed guar gum in chemotherapy induced high output stoma in patient with ileostomy Ho CY , Ahmad AF , Sian WS , Selvarajoo T, Jamhuri N, Kahairudin Z. Asian J Diet.2019;:1-4.
- Relationship Between the Gut Microbiome and Systemic Chemotherapy Ervin SM , Ramanan SV , Bhatt AP . Digestive Diseases and Sciences.2020;65(3). CrossRef
- Epidemiology, risk factors and treatments for antibiotic-associated diarrhea McFarland L. V.. Digestive Diseases (Basel, Switzerland).1998;16(5). CrossRef
- Diarrhea Incident in Cervical Cancer Patients Post Chemotherapy Treatment Muhayanah M , Nastiti A . Jurnal Ners.2025;11(1). CrossRef
- Evaluation and management of treatment-related diarrhea in patients with advanced cancer: a review Cherny NI . Journal of Pain and Symptom Management.2008;36(4). CrossRef
- A Randomized Controlled Trial of Novel Treatment for Hemorrhagic Radiation Proctitis Pui WC , Chieng TH , Siow SL , Nik Abdullah NA , Sagap I. Asian Pacific journal of cancer prevention: APJCP.2020;21(10). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2025
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times