Digital Nutrition in Cancer Care: A Co-Design Approach to Transform Chemotherapy Patient Outcomes
Download
Abstract
-
Introduction
Cancer treatment, especially chemotherapy, poses unprecedented challenges to patients’ nutritional health and dietary management. The prevalence of malnutrition among cancer patients ranges from 20% to over 70%, with malnutrition responsible for 10-20% of cancer-related deaths rather than the malignancy itself [1]. Recent research indicates that 39% of hospitalised cancer patients are malnourished, with 51.1% experiencing nutritional impairment, including risk of malnutrition and overt malnutrition [2, 3]. This high prevalence greatly affects treatment tolerance, quality of life, and clinical outcomes.
Traditional approaches to nutritional assessment and intervention, while fundamental, often lack the personalised, real-time support that modern cancer patients need. The rise of digital health technologies offers unprecedented opportunities to revolutionise cancer nutrition care, but only when these solutions are developed through genuine collaboration with patients and caregivers using co-design methodologies.
Current Challenges in Cancer Nutrition
Cancer patients face a constellation of nutritional challenges extending beyond simple appetite loss. Malnutrition affects up to 75% of cancer patients, with prevalence varying according to tumour type, stage, treatment type, patient age, and care setting. Approximately 15-50% of cancer patients present with nutritional deficiencies at diagnosis, while 43% and 9% have overt malnutrition or are at risk of malnutrition, respectively, at their first oncologic visit [4].
The prevalence varies greatly according to cancer type, with gastroesophageal, pancreatic, head and neck, and lung tumours exhibiting the highest rates of malnutrition. Unintentional weight loss impacts 65% of cancer patients at their initial medical oncology appointment, with 28.4% losing over 10% of their body weight [2, 5].
The development of tools like the Chemotherapy Dietary Adherence Scale (CDAS) has provided crucial insights into the dietary adherence challenges faced by patients undergoing chemotherapy [6]. However, traditional nutritional assessment approaches often rely on periodic consultations and static measurements that fail to capture the dynamic, day-to-day fluctuations characterising the chemotherapy experience.
Healthcare systems across the Asia-Pacific region face additional challenges, including limited dietitian- to-patient ratios, geographical barriers to specialist care, and cultural diversity requiring tailored nutritional interventions.
Digital Technologies Transforming Nutritional Care
Mobile health (mHealth) applications represent the most accessible entry point for digital nutrition interventions in cancer care. However, a comprehensive analysis of 123 cancer-related smartphone apps revealed significant quality concerns, highlighting the critical need for evidence-based, co-designed solutions [7].
The analysis found that only 3% of cancer apps had content developed or evaluated by health providers, despite 90% being developed by commercial entities. Most concerning, 15% of apps claimed to offer advice about “cancer-fighting foods” and nutrition, yet none provided scientific evidence supporting these claims. Only 10% of apps identified content sources, and very few supported critical interactive features such as connecting with health providers (4%) or sharing medical records (3%) [7].
Artificial intelligence (AI) technologies offer remarkable potential for personalising nutritional recommendations based on individual patient characteristics and real-time symptom reporting. The national implementation of an AI- based virtual dietitian, “Ina,” demonstrated the feasibility and effectiveness of evidence-based, AI-powered nutrition support [8].
Among 3,310 cancer patients across all 50 US states who used Ina, engagement levels were high: 68% texted questions, 79% completed surveys, with a median user retention of 8.8 months. Importantly, 94% of participants were satisfied with the platform, 84% utilised AI guidance to modify their diet, 82% reported an improved quality of life, and 88% experienced better symptom management [8].
The success of Ina can be attributed to its development based on more than 100,000 expert-curated interventions, peer-reviewed literature, and clinical guidelines, demonstrating how AI can be effectively implemented when grounded in evidence-based practice.
Telehealth integration provides opportunities for virtual consultations, real-time cooking demonstrations, and ongoing support that accommodates patients’ varying energy levels and treatment schedules. When integrated with digital nutrition tools, telehealth platforms enable more targeted, efficient consultations informed by real-time patient-generated data.
The Critical Importance of Co-Design
Co-design represents a fundamental shift from traditional technology development approaches, involving patients, caregivers, and healthcare providers as active partners throughout the entire design and development process. An umbrella review of digital health intervention co-design found that participatory design processes resulted in significantly higher user satisfaction scores, improved usability metrics, and better clinical outcomes compared to conventionally developed applications [9].
Co-designed cancer care applications demonstrated sustained engagement rates 40-60% higher than traditionally developed solutions and significantly improved patient-reported outcome measures [10]. The poor quality and low engagement rates of existing cancer apps underscore the importance of co-design approaches.
Evidence Supporting Co-Design Approaches
Recent research demonstrates the critical importance of patient engagement in digital health development. A scoping review found that despite the benefits of including cancer survivors on research teams, few studies have meaningfully involved them in the design process [11]. This represents a significant missed opportunity, as patient partners bring unique perspectives about managing treatment-related side effects and navigating dietary restrictions.
A study developing an mHealth app for cancer survivors with disabilities through co-design found that working directly with cancer survivors ensured the design team maintained focus on creating something patients would actually want to use and benefit from [12-14]. The co-design process yielded both a functional prototype and guidelines for other researchers.
Successful co-design in digital cancer nutrition requires several fundamental principles: genuine partnership, treating patients and caregivers as equal partners; intentionally cultivating diversity and inclusion throughout the process; and iterative design processes that allow for continuous refinement based on user feedback.
Figure 1 illustrates the comprehensive co-design process framework that should guide the development of digital cancer nutrition solutions, emphasising the iterative nature of patient engagement and multiple stakeholder perspectives required for successful implementation.
Figure 1. Co-Design Process Framework for Digital Cancer Nutrition Solutions.
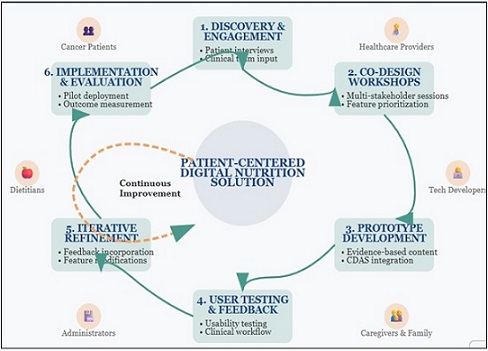
This framework illustrates the iterative co-design process for developing digital cancer nutrition solutions, highlighting the continuous collaboration between patients, caregivers, healthcare providers, and technology developers. The diagram illustrates how stakeholder input influences each development phase, from initial needs assessment through prototype development, testing, refinement, and implementation. Key components include user-centred research, participatory design workshops, iterative prototype testing, and ongoing feedback loops that ensure the final solution meets the real-world needs of cancer patients and their care teams.
Implementation and Future Directions
The analysis of existing cancer apps reveals the critical importance of establishing quality standards for digital nutrition tools. Successful implementation requires addressing several key challenges: ensuring clinical validation of content, establishing transparency regarding developer affiliations and content sources, and implementing peer-review processes for app content.
The integration of digital nutrition tools into existing healthcare workflows requires comprehensive training and support for healthcare providers. Co-design processes that include healthcare providers as active participants can help identify training needs and develop implementation strategies aligning with clinical workflows.
The future of digital cancer nutrition lies in integration with precision medicine approaches that account for individual patient characteristics while maintaining grounding in validated assessment tools. The Chemotherapy Dietary Adherence Scale (CDAS) represents a crucial bridge between traditional psychometric assessment approaches and modern digital health solutions [6].
As the first validated tool specifically designed to assess dietary adherence in chemotherapy patients, the CDAS provides a robust foundation for developing digital nutrition interventions that are both scientifically sound and clinically relevant. Digital platforms incorporating validated assessment tools benefit from established psychometric properties while gaining advantages of real- time data collection and personalised feedback.
Continued research is needed to establish the clinical effectiveness and cost-effectiveness of digital nutrition interventions in cancer care. Patient-reported outcome measures, such as the CDAS, will be essential for capturing the full impact of digital nutrition interventions on patient experience and quality of life.
In conclusion, the transformation of cancer nutrition care through digital technologies represents one of the most promising opportunities to improve outcomes and quality of life for chemotherapy patients globally. However, realising this potential depends critically on our commitment to human-centred design approaches that place patients, caregivers, and healthcare providers at the centre of the development process.
The stark contrast between poorly designed commercial cancer apps and evidence-based platforms like Ina demonstrates that technology alone is insufficient; success requires clinical validation, patient engagement, and evidence-based development processes. Co-design methodologies offer a proven pathway for developing digital health solutions that are not only technologically sophisticated but also clinically effective, culturally appropriate, and sustainable in real-world healthcare settings.
The integration of validated assessment tools, such as the CDAS, with co-designed digital platforms provides a foundation for evidence-based, patient-centred innovation that can truly transform cancer nutrition care. As we advance into this digital future, our success will be measured not by the sophistication of our technologies but by their impact on the daily lives and treatment experiences of cancer patients and their families.
The path forward requires sustained collaboration between patients, caregivers, healthcare providers, technology developers, and researchers, with a fundamental commitment to evidence-based practice and placing human needs at the centre of everything we do.
Conflict of Interest
The authors declare no conflicts of interest.
References
- Malnutrition in cancer patients: Causes, consequences and treatment options Arends J. European Journal of Surgical Oncology: The Journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology.2024;50(5). CrossRef
- Prevalence of malnutrition in patients at first medical oncology visit: the PreMiO study Muscaritoli M, Lucia S, Farcomeni A, Lorusso V, Saracino V, Barone C, Plastino F, et al . Oncotarget.2017;8(45). CrossRef
- Use of the scored Patient-Generated Subjective Global Assessment (PG-SGA) as a nutrition assessment tool in patients with cancer Bauer J., Capra S., Ferguson M.. European Journal of Clinical Nutrition.2002;56(8). CrossRef
- Malnutrition management in oncology: An expert view on controversial issues and future perspectives Bossi P, De Luca R, Ciani O, D'Angelo E, Caccialanza R. Frontiers in Oncology.2022;12. CrossRef
- Exploring Malnutrition Risk in Cancer Chemotherapy Patients: An Assessment of Associated Factors in a Tertiary Care Cancer Center Prakash GH , D SK , Pk K, Arun V, Yadav D, Gopi A. Asian Pacific Journal of Cancer Care.2024;9(1). CrossRef
- Enhancing Nutritional Care in Cancer: Development and Face Validation of the Chemotherapy Dietary Adherence Scale Prakash GH , D SK , Pk K, Arun V, Yadav DMS . Asian Pacific Journal of Cancer Care.2024;9(3):501-504. CrossRef
- Smartphone apps for cancer: A content analysis of the digital health marketplace Charbonneau DH , Hightower S, Katz A, Zhang K, Abrams J, Senft N, Beebe-Dimmer JL, et al . Digital Health.2020;6. CrossRef
- National Implementation of an Artificial Intelligence-Based Virtual Dietitian for Patients With Cancer Buchan ML , Goel K, Schneider CK , Steullet V, Bratton S, Basch E. JCO clinical cancer informatics.2024;8. CrossRef
- An umbrella review on how digital health intervention co-design is conducted and described Kilfoy A, Hsu TC , Stockton-Powdrell C, Whelan P, Chu CH , Jibb L. NPJ digital medicine.2024;7(1). CrossRef
- The importance of patient-reported outcomes in clinical trials and strategies for future optimization Mercieca-Bebber R, King MT , Calvert MJ , Stockler MR , Friedlander M. Patient Related Outcome Measures.2018;9. CrossRef
- Patient engagement strategies in digital health interventions for cancer survivors: A scoping review Ren M, Orsso CE , Ghomashchi H, Silva BR , Aubrey C, Nielssen I, Pin S, et al . PLOS digital health.2025;4(5). CrossRef
- Developing an mHealth App for Empowering Cancer Survivors With Disabilities: Co-design Study Adler RF , Morales P, Sotelo J, Magasi S. JMIR formative research.2022;6(7). CrossRef
- Designing a Framework for Remote Cancer Care Through Community Co-design: Participatory Development Study Aronoff-Spencer E, McComsey M, Chih M, Hubenko A, Baker C, Kim J, Ahern DK , et al . Journal of Medical Internet Research.2022;24(4). CrossRef
- The Effect of Nutritional Mobile Apps on Populations With Cancer: Systematic Ng KLS , Munisamy M, Lim JBY , Alshagga M. .
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2025
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times