Intraosseous Mucoepidermoid Carcinoma of the Mandible: A Case Report with Three-Year Follow-Up
Download
Abstract
Background: Mucoepidermoid carcinoma (MEC) is the most common malignant salivary gland tumor, but its intraosseous (central) presentation in the jaws is extremely rare and often mimics benign odontogenic lesions.
Case: We describe a 37-year-old woman with swelling and dull pain in the left mandible. Clinical and radiographic evaluation, including cone-beam computed tomography (CBCT), revealed a destructive multilocular radiolucent lesion with cortical perforation.
Treatment: An incisional biopsy confirmed the diagnosis of low-grade intraosseous MEC. The lesion was surgically excised, and mandibular reconstruction was performed using an autogenous fibular bone graft.
Outcome: At a three-year follow-up, the patient showed complete recovery with no evidence of recurrence. This case underscores the importance of timely diagnosis, appropriate surgical management, and long-term follow-up in intraosseous salivary gland malignancies.
Introduction
Mucoepidermoid carcinoma (MEC) accounts for 10–15% of all salivary gland tumors and one-third of all malignant salivary gland tumors, and is therefore the most common malignant salivary gland tumor, occurring across a wide age range with a median age of 45-50 years [1-3]. Furthermore, MEC has been shown to be more prevalent in women than in men, possibly due to the differential expression of sexual hormones in women and men [4]. This tumor has a solid mass that is usually asymptomatic and can imitate the behavior of other salivary gland tumors, so it is often considered in the differential diagnosis of salivary gland tumors. Mucoepidermoid carcinoma has also been reported to resemble mucoceles within the oral cavity [5]. Mucoepidermoid carcinomas are composed of mucin-secreting cells, squamous cells, and intermediate cells [6]. In addition to these cells, other cell types, including clear, spindle, goblet, and oncocytic cells, may be found [1]. The histological grading of MEC is usually divided into low, intermediate, and high grade.
As the histopathological grade increases, MEC becomes more infiltrative and less or undifferentiated, making it difficult to diagnose. Oncocytic MEC (OMEC) is defined when MEC is frequently associated with oncocytic cells, and most cases occur in the parotid gland, followed by the submandibular and sublingual glands [1, 2].
Benign or malignant salivary gland tumors do not usually arise from the jawbone or are rarely intraosseous and central, and only 2–3% of all mucoepidermoid carcinomas arise within the jaws as primary intraosseous (central) lesions [7]. Most primary central mucoepidermoid carcinomas arise in the mandible, while maxillary lesions are uncommon. There has been much debate about its etiology, radiological aspects, and histology. This rare lesion may arise from the epithelial lining of an odontogenic cyst or may originate from epithelial remnants of a misplaced salivary gland [3].
As mentioned, the malignancy of this tumor and its rare intraosseous occurrence double the importance of early diagnosis, treatment, and follow-up. Case reports of rare entities such as intraosseous MEC provide valuable clinical insights and contribute to the existing knowledge by highlighting unusual presentations and guiding clinicians in differential diagnosis and management.
The aim of this report is to present a case of intraosseous mucoepidermoid carcinoma of the mandible with uncommon clinical features, including pain and cortical perforation, and to discuss its diagnosis, management, and three-year follow-up outcome.
Case Presentation
A 37-year-old female patient complained of swelling on the left side of the lower jaw and referred to the Department of Oral, Maxillofacial Diseases of Mashhad Dental School on July 11, 2021. The patient stated that the pain in this area started about a year ago and the reason for referral to the Dental School was that the dentist had observed the swelling about a month earlier, and since then its size had not changed significantly. The pain was reported as dull and during yawning and nervous excitement.
Extraoral clinical examination revealed a slight swelling in the area corresponding to the left ramus of the mandible. The left mandibular angle was also not palpable, and the lymph nodes were normal.
In intraoral examination, a sessile exophytic lesion with a smooth surface measuring 2 x 2.5 cm was observed on the posterior ridge of the left mandibular second molar, which was red in most areas with telangiectasia and normal in some areas. On buccal expansion palpation, bony hard was observed in the area of left mandibular second molar with a high probability of extension to the ramus, which also slightly involved the lingual side. However, the consistency of the ridge surface lesion (the mass resulting from bone perforation) was rubbery. Left mandibular second molar had anterior displacement and grade 1 looseness, but there was no tenderness or neurological symptoms. In examining the contact of the lesion with the tooth, the distolingual cusp of left maxillary tooth 7 and the maxillary ridge were in contact with the lesion, but no ulcer was formed (Figure 1).
Figure 1. Intraoral View: Exophytic lesion without base and smooth surface with red color and telangiectasia in the posterior ridge area of left mandibular second molar.

After a complete extraoral and intraoral examination, considering the centrality of the lesion and the unexplained increase in size, as well as the prevalence and location of the lesion, the possibility of an odontogenic tumor with malignant transformation was initially raised. Panoramic radiography showed a multilocular radiolucent lesion extending from the distal region of the left mandibular second molar to the neck of the condyle and below the sigmoid notch. A bony projection resembling a periosteal reaction was seen at the anterior border of the ramus (Figure 2).
Figure 2. Panoramic View: General view of the lesion on the left side of the mandible with extension towards the ramus (in the panoramic radiograph of the patient, a multilocular lesion is seen in the posterior region of the mandible from the distal second molar to below the sigmoid notch)..

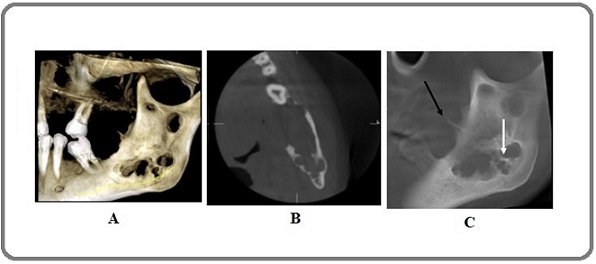
CBCT showed erosion and perforation of the buccal and lingual walls, as well as a downward displacement of the inferior alveolar nerve canal and anterior tilt of the left mandibular second molar. Sagittal planes showed a large lacuna that perforated the anterior ramus wall, and the remaining walls appeared similar to the periosteal reaction (Figure 3).
Figure 3. A, CBCT (3D view): multilocular lesion and bony projections in the anterior wall of the ramus; B, CBCT ( Axial view): multilocular lesion (multilocular with coarse septa); C, CBCT (sagittal view): The lesion is multilocular with coarse septa (white arrow). Note the bony projection (black arrow) that closely resembles a periosteal reaction.
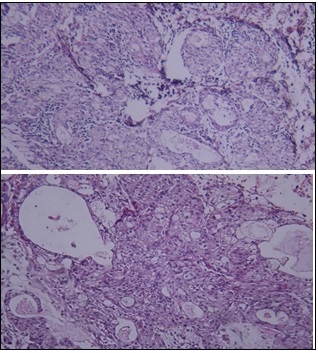
After clinical and radiographic examination, an incisional biopsy was performed and a 4 x 3 cm cream to gray tumor sample was examined. Under the microscope, neoplastic and malignant proliferation of salivary gland epithelial cells was observed, which had proliferated in the form of multiple lobules and plates. The neoplastic cells often had foamy cytoplasm with a mucoid appearance. Intermediate cells were also observed. There was formation of multiple ducts and cystic areas between the cell lobules, and the surface of the lesion was covered by hyperplastic parakeratinized squamous stratified epithelium. Therefore, considering the presence of multiple cystic and microcystic spaces and the fact that the majority of the cells were clear and mucoid, the tumor in question was diagnosed as Low Grade (Figure 4).
Figure 4. A, Histopathological view; Presence of mucous cells, epidermoid cells and cystic spaces. 100X, B: Histopathological view; Presence of mucous cells, epidermoid cells and cystic spaces. 400X.
Finally, according to clinical examinations, radiographic studies, and biopsy results, the final diagnosis was intraosseous mucoepidermoid carcinoma. The patient was referred to an oncologist. According to the specialist, chemotherapy was not needed. Surgical treatment, including tumor removal and bone grafting from the patient’s leg (fibula), was performed on September 15, 2021.
During a telephone call with the patient on November 16, 2024 (about three years after surgical treatment) for follow-up, she refused to return to the dental school in person, but the patient stated that she currently had no specific problems with his previously treated lesion.
Discussion
Intraosseous mucoepidermoid carcinoma (MEC) is a very rare malignant neoplasm originating from within the bones of the jaw. The first documented case of MEC in the mandible was reported by Lepp in1939 [8]. In total, more than 200 cases of central MEC have been documented in the scientific literature, indicating the rarity of this disease [9]. According to epidemiological studies, intraosseous MEC accounts for only 2–3% of all mucoepidermoid carcinomas of the head and neck region [10]. The mandible is more commonly involved than the maxilla, with a tendency to be posterior, especially in the premolars and molars [11].
The origin of intraosseous MEC remains controversial and several theories have been proposed. The most widely accepted theories include: (1) neoplastic transformation of mucous cells in odontogenic cysts; (2) entrapment of retromolar mucous glands within the mandible; (3) embryonic salivary gland tissue that has been encased in bone during development; and (4) alteration of mucus-secreting cells in the maxillary sinus epithelium [12]. In the present case, the association with the impacted tooth suggests neoplastic transformation from an odontogenic cyst, which supports the first theory.
Clinically, intraosseous MEC usually presents as a painless swelling with cortical expansion but no perforation [13]. This asymptomatic presentation often results in a delay in diagnosis, as patients may not seek treatment until significant expansion has occurred. Brookston and Howes proposed a clinical staging system based on the status of the overlying bone: stage I (no bony expansion), stage II (with expansion but intact cortex), and stage III (cortical perforation or lymph node involvement) [14]. It is noteworthy that the case presented here has distinctive features that differ from the typical presentation. The patient reported pain and showed cortical bone perforation, which is therefore classified as stage III according to the Brookston and Howes system. This symptomatic presentation with bone perforation is unusual and indicates a more aggressive clinical behavior than has been reported in typical cases [15]. However, given the history of pain from a year ago and the ambiguity of the type of pain, we cannot be certain that the cause of the pain is tumor-related.
Radiographically, intraosseous MEC usually appears as a well-defined, single- or multi-cavity radiolucent lesion that may resemble benign odontogenic lesions [16], as was the case in this case. This radiographic similarity to benign conditions presents a diagnostic challenge. In the present case, the radiographic appearance may initially suggest an ameloblastoma, a common misdiagnosis for these lesions. Chan et al. noted that despite their malignant nature, intraosseous MECs often maintain well-defined borders on radiographs, a feature usually associated with benign lesions [17].
Histopathologically, MEC is characterized by a mixture of mucous, epidermoid, and intermediate cells arranged in varying proportions. The World Health Organization classifies MEC into low, intermediate, and high grade based on cellular composition, cystic spaces, nuclear atypia, and mitotic activity [18]. Low-grade tumors have a prominent cystic appearance, minimal cellular atypia, and a higher proportion of mucinous cells, whereas high-grade tumors exhibit solid growth patterns with predominant epidermoid cells and significant cellular atypia [19]. The case presented here showed features of low-grade MEC (the presence of numerous cystic and microcystic spaces and a predominance of clear and mucinous cells on histopathological examination of the lesion), which usually has a better prognosis than higher grades.
Molecular studies have identified genetic alterations in MEC, particularly fusions of the CRTC1 and MAML2 genes, which are present in approximately 70% of cases and are associated with low- to intermediate-grade tumors and favorable outcomes [20]. This genetic marker has diagnostic and prognostic value, although it has not been evaluated in our case. Unfortunately, molecular testing was not performed in this case, which is a limitation as such markers could have provided additional diagnostic and prognostic information.
The treatment of intraosseous MEC mainly consists of surgical resection with adequate margins. In a comprehensive review, Kochaji et al. reported recurrence rates up to 40% with conservative treatments such as curettage, whereas radical resection reduced recurrence to approximately 4% [7]. Therefore, segmental mandibulectomy with clean margins is the treatment of choice for these lesions. Adjuvant radiotherapy is recommended for high-grade tumors, non-clean surgical margins, neurovascular invasion, or lymph node metastasis [21]. In our patient, chemotherapy was not indicated because the tumor was low-grade, surgical margins were clear, and there was no evidence of nodal or distant metastasis.
The prognosis of intraosseous MEC varies based on histological grade and clinical stage. Low-grade tumors usually have an excellent prognosis with a 5-year survival rate of more than 95% after appropriate treatment [22]. However, high-grade tumors and those with cortical perforation or lymph node involvement have a less favorable prognosis and an increased risk of recurrence and metastasis [14]. Written informed consent was obtained from the patient for the publication of this case report and accompanying clinical details. This case highlights the necessity of performing biopsy and histopathological evaluation for atypical exophytic jaw lesions, as their benign clinical appearance may mask underlying malignancies.
In conclusion, Intraosseous mucoepidermoid carcinoma is a rare but significant malignancy of the jaws that can mimic benign odontogenic lesions. Although it most often presents as a painless swelling, our case highlights that atypical features such as pain and cortical perforation may also occur. Definitive diagnosis requires histopathological evaluation, underscoring the importance of biopsy in atypical jaw lesions. Radical surgical excision with reconstruction remains the mainstay of treatment, with excellent outcomes for low-grade tumors. Future studies on molecular markers, such as CRTC1-MAML2 fusions, may enhance diagnostic accuracy and provide prognostic insights. Long-term follow-up is essential to monitor for recurrence.
Conflict of Interest
The authors declare no conflict of interest.
Patient Consent Statement
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images. The patient’s identity has been protected, and all efforts have been made to ensure confidentiality.
Originality Declaration for Figures
All figures included in this manuscript are original and have been created by the authors specifically for the purposes of this study. No previously published or copyrighted images have been used. The authors confirm that all graphical elements, illustrations, and visual materials were generated from the data obtained in the course of this research or designed uniquely for this manuscript.
References
- Intraoral Oncocytic Mucoepidermoid Carcinoma - A Rare Case Report and Review of the Literature Sripodok P, Poomsawat S, Juengsomjit R, Kosanwat T. Annals of Maxillofacial Surgery.2021;11(2). CrossRef
- Advances in the Treatment of Mucoepidermoid Carcinoma Sama S, Komiya T, Guddati AK . World Journal of Oncology.2022;13(1). CrossRef
- Mucoepidermoid Carcinoma of Palate Treated with Temporalis Muscle Flap Reconstruction Howayw Y, Zobia N, Salah KB . Libyan International Journal of Oncology.2023.
- Epidemiology, prognostic factors, and treatment of head and neck mucoepidermoid carcinoma: Analysis of the surveillance, epidemiology, and end results database Gui L, Zhu Y, Zhang Y, Tang , Yao J. Brazilian Journal of Otorhinolaryngology.2024;90(5). CrossRef
- Mucoepidermoid carcinoma of oral mucosa Jain R, Mohan R, Janardhan A, Jain R. BMJ case reports.2015;2015. CrossRef
- Mucoepidermoid lung tumor. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan– [Updated 2023 Sep 4] Limaiem F, Lekkala MR , Sharma S. .
- Central Mucoepidermoid carcinoma: Case report, literature review for missing and available information and guideline proposal for coming case reports Kochaji N, Goossens A, Bottenberg P. Oral Oncology Extra.2025;40(8-9). CrossRef
- Central Mucoepidermoid carcinoma of mandible - A case report and review of the literature Simon D, Somanathan T, Ramdas K, Pandey M. World Journal of Surgical Oncology.2003;1(1). CrossRef
- Primary intraosseous mucoepidermoid carcinoma of the jaw: Reappraisal of The MD Anderson Cancer Center experience Bell D, Lewis C, El-Naggar AK , Weber RS . Head & Neck.2016;38 Suppl 1. CrossRef
- Intraosseous Mucoepidermoid Carcinoma of the Anterior Mandible: A Case Report Khataniar H, Senthil S, Deep SS , Ramesh R, Inchara YK . Cureus.2022;14(5). CrossRef
- Central mucoepidermoid carcinoma of the mandible: report of four cases with long-term follow-up Pires F. R., Paes de Almeida O., Lopes M. A., Elias da Cruz Perez D., Kowalski L. P.. International Journal of Oral and Maxillofacial Surgery.2003;32(4). CrossRef
- Aggressive growth and neoplastic potential of odontogenic cysts: with special reference to central epidermoid and mucoepidermoid carcinomas Eversole L. R., Sabes W. R., Rovin S.. Cancer.1975;35(1). CrossRef
- Intraosseous mucoepidermoid carcinoma: report of two cases Atarbashi Moghadam S., Atarbashi Moghadam F.. Journal of Dentistry (Shiraz, Iran).2014;15(2).
- Central salivary gland tumors of the maxilla and mandible: a clinicopathologic study of 11 cases with an analysis of the literature Brookstone M. S., Huvos A. G.. Journal of Oral and Maxillofacial Surgery: Official Journal of the American Association of Oral and Maxillofacial Surgeons.1992;50(3). CrossRef
- Intraosseous Mucoepidermoid Carcinoma of the Mandible Arising From a Cystic Lesion: A Case Report Jamalpour MR , Dehghan A, Nadripour R, Fatehi F, Nahidfar H, Naderi H. Avicenna Journal of Dental Research.2023;15(4). CrossRef
- Intraosseous mucoepidermoid carcinoma: a review of the diagnostic imaging features of four jaw cases Chan KC, Pharoah M, Lee L, Weinreb I, Perez-Ordonez B. Dentomaxillofacial Radiology.2013;42(4). CrossRef
- An unusual case of intraosseous mucoepidermoid carcinoma of the mandible: A case report and literature review Li X, Wang F, Wang Y, Sun S, Yang H. Medicine.2018;97(51). CrossRef
- Central mucoepidermoid carcinoma: Case report with review of literature Singh H, Yadav AK , Chand S, Singh A, Shukla B. National Journal of Maxillofacial Surgery.2019;10(1). CrossRef
- Clear cell variant of intraosseous mucoepidermoid carcinoma: Report of a rare entity Varma S, Shameena P, Sudha S., Nair RG , Varghese IV . Journal of oral and maxillofacial pathology: JOMFP.2012;16(1). CrossRef
- Genomic profiles and CRTC1-MAML2 fusion distinguish different subtypes of mucoepidermoid carcinoma Jee KJ , Persson M, Heikinheimo K, Passador-Santos F, Aro K, Knuutila S, Odell EW , et al . Modern Pathology: An Official Journal of the United States and Canadian Academy of Pathology, Inc.2013;26(2). CrossRef
- Central mucoepidermoid carcinoma of the mandible Freije J. E., Campbell B. H., Yousif N. J., Clowry L. J.. Otolaryngology--Head and Neck Surgery: Official Journal of American Academy of Otolaryngology-Head and Neck Surgery.1995;112(3). CrossRef
- Central mucoepidermoid carcinoma of the jaw with distant metastasis: a case report and review of the literature Lebsack J. P., Marrogi A. J., Martin S. A.. Journal of Oral and Maxillofacial Surgery: Official Journal of the American Association of Oral and Maxillofacial Surgeons.1990;48(5). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2025
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times