Prognostic value of vitamin-D level in non-metastatic breast cancer patients in Saudi Arabia.
Download
Abstract
Background: Deficiency of vitamin-D (Vit-D) was associated with poor survival outcome in several studies across different tumour types. The present study aims to assess the prevalence and prognostic value of Vit-D deficiency among breast cancer patients in a single institution in Saudi Arabia.
Methods: In this retrospective study, we screened patients who presented with non-metastatic breast cancer to King Abdullah Medical City, Saudi Arabia from June 2011 to December 2015. We checked baseline Vit-D level before starting systemic therapy in addition to other clinicopathological factors. Low Vit-D was defined as Vit-D level less than 30 ng /ml. The relations of Vit-D level (taking the median as the cutoff) with clinicopathological factors were assessed using Chi-Square test. Differences in survival outcome were compared using log rank test.
Results: We screened 340 patients with non-metastatic breast cancer. Baseline Vit-D levels were available for 189 patients. The median age was 50 years (range: 26- 86 years). Noteworthy, 169 (89.4%) of patients had Vit-D level <30 ng/ml with a median of 14.9 ng/ml (range: 4.0 - 45.0). Low Vit-D level (below the median) was significantly more common in premenopausal (p=0.011) and ER-negative patients (p=0.011). However, lymphovascular invasion (p=0.001), clinically (p=0.023) and pathologically positive axillary LNs (p=0.041) were linked with higher Vit- D level. After a median follow up period of 58.2 months, 14 patients died and 40 relapsed. The 5-year disease-free survival (DFS) rates was 74.8%. The 5-year DFS rate in patients with higher Vit-D level above the median was 78.8% compared to 71.1% in patients with lower Vit-D level with no statistically significance difference (p= 0.22). The 5-year overall survival (OS) rate was 90.2%. Meanwhile, no difference in 5-year OS rate in patients with higher and lower Vit-D levels (90.3% and 89.7% respectively, p=0.6).
Conclusion: Low Vit-D level was prevalent among the studied breast cancer patients. Low Vit-D level was associated with ER-negative phenotype and premenopausal patients. Baseline Vit-D level was not significantly linked with survival outcome.
Introduction
Vitamin D (Vit-D) plays a vital role in calcium homeostasis, skeletal metabolism in addition to other vital physiological roles. Vit-D deficiency is a common health problem with numerous health consequences including osteomalacia, osteoporosis and fractures in adults [1].
Many reports showed an association between serum Vit-D deficiency and development of several types of cancer, including breast, colorectal, kidney and pancreatic cancers [2][3]. Several studies have confirmed that vitamin D receptors (VDR) are expressed in normal breast tissues and also in breast cancer biopsy specimens [4][5]. Noteworthy, Vit-D promotes apoptosis through the insulin-like growth factor receptor 1 (IGFR)- (PI3K)-Akt-dependent signaling pathway [3][4][5][6]. Therefore, deregulation of Vit-D signaling and related metabolic pathways was suggested to play an important role in tumour growth [7]. Meanwhile, large epidemiological studies suggested that Vit- D intake has a protective role against breast cancer development [8][9].
However, the prognostic value of VDR expression and circulating Vit-D level still remains controversial. Several studies reported that deficiency of Vit-D was associated with poor survival outcome across different tumour types while other studies reported different conclusions [10][11][12][13]. The present study aims to assess the prognostic value of Vit-D deficiency among non-metastatic breast cancer patients in a single institution in Saudi Arabia. This may give rise to an easy prognostic parameter that can be assessed in daily practice.
Materials and Methods
Study population
Patients with histologically confirmed non-metastatic breast cancer who presented to King Abdullah Medical City, Saudi Arabia from June 2011 to December 2015, were included. Enrolled patients must have available baseline serum Vit-D level before starting any systemic therapy.
Study design and procedures
In this retrospective study, eligible patients must have adequate medical records. We checked baseline Vit-D level before starting systemic therapy in addition to other clinicopathological factors. Different parameters were collected including age, gender, stage at diagnosis, body mass index (BMI), pathological type, grade, ER, PR and HER2 status in addition to treatment data including type and number of chemotherapy cycles, hormonal therapy and trastuzumab (if applicable). Dates of disease relapse and death if any, were recorded.
Statistical analysis
SPSS version 21 statistical program was used. Descriptive statistics were performed for all clinical, laboratory and pathological data. Low Vit-D was defined as Vit-D level less than 30 ng /ml. The relations of Vit-D level (taking 30 ng/ ml and the median as the cutoffs) with clinico-pathological factors were assessed using Chi-Square test. Different potential prognostic factors were assessed in relation with disease free survival (DFS) and overall survival (OS). Survival data was presented by Kaplan Meier method where cases with no recorded events (death or relapse) were censored at the date of last contact. Comparisons of survival outcome among different parameters were assessed using the log rank test. A two-sided alpha was set at 0.05. DFS was defined as the time from date of breast surgery to date of documented tumour relapse or death. OS was defined as the time from the date of diagnosis of breast cancer till the date of death.
Results
Patients’ and tumor characteristics
We screened 340 patients with non-metastatic breast cancer. Baseline Vit-D levels were available for 189 patients with a median level of 14.9 ng/ml (range: 4.0 - 45.0). Noteworthy, 169 (89.4%) of patients had Vit-D level <30 ng/ml. Using 30 ng/ml as the cutoff, there was no significant association between different parameters and Vit-D level. We therefore, used the median Vit-D level as the cutoff to have enough patients for comparison. The median age was 50 years (range: 26- 86 years) and it was significantly lower in patients with lower compared to higher Vit-D levels (47 vs. 51 years respectively, p=0.04). Similarly, Low Vit-D level (below the median) was significantly more common in premenopausal compared to postmenopausal patients (59.4%, 40.9%, respectively, p=0.01) and ER-negative vs. positive patients (63.1% vs 43.5%, respectively, p=0.01). However, lymphovascular invasion (LVI) (72.2% vs. 27.8%, p=0.001), clinically (62.5% vs. 37.5% respectively, p=0.02) and pathologically positive axillary LNs (p=0.04) were linked with higher Vit- D level. However, other clinicopathological factors did not significantly differ according to Vit-D level (Table 1).
| Parameters | Total=189 No |
Vitamin D |
Vitamin D ≥median No (%) | P |
| Median age (range) | 50 (26-86) | 47 (26-76) | 51 (31-86) | 0.04 |
| Menopausal status | ||||
| Premenopausal | 96 | 57 (59.4) | 39 (40.6) | 0.01 |
| Postmenopausal | 93 | 38 (40.9) | 55 (59.1) | |
| Body mass index | ||||
| <25 | 19 | 13 (68.4) | 6 (31.6) | |
| 25-29.9 | 69 | 31 (44.9) | 38 (55.1) | 0.25 |
| 30-39.9 | 79 | 38 (48.1) | 41 (51.9) | |
| ≥40 | 22 | 13 (59.1) | 9 (40.9) | |
| Pathology | ||||
| IDC | 178 | 89 (50.0) | 89 (50.0) | 0.07 |
| ILC | 7 | 2 (28.6) | 5 (71.4) | |
| Other | 4 | 4 (100.0) | 0 (0.0) | |
| Grade | ||||
| Grade 1 | 11 | 8 (72.7) | 3 (27.3) | |
| Grade 2 | 104 | 51 (49.0) | 53 (51.0) | 0.07 |
| Grade 3 | 63 | 34(54.0) | 29 (46.0) | |
| Unknown | 11 | 2 (18.2) | 9 (81.8) | |
| Lymphovascular invasion | ||||
| Yes | 54 | 15 (27.8) | 39 (72.2) | <0.001 |
| No | 127 | 76 (59.8) | 51 (40.2) | |
| ER status | ||||
| Negative | 65 | 41 (63.1) | 24 (36.9) | |
| Positive | 124 | 54 (43.5) | 70 (56.5) | 0.01 |
| PR Status | ||||
| Negative | 82 | 46 (56.1) | 36 (43.9) | 0.16 |
| Positive | 107 | 49 (45.8) | 58 (54.2) | |
| HER2 status | ||||
| Negative | 124 | 62 (50.0) | 62 (50.0) | |
| Positive | 62 | 33 (53.2) | 29 (46.8) | 0.19 |
| Unknown | 3 | 0 (0.0) | 3 (100.0) | |
| Clinical Stage | ||||
| Stage I | 20 | 12 (60.0) | 8 (40.0) | |
| Stage II | 88 | 41 (46.6) | 47 (53.4) | |
| Stage IIIA | 52 | 30 (57.7) | 22 (42.3) | 0.42 |
| Stage IIIB | 17 | 6 (35.3) | 11 (64.7) | |
| Unknown | 12 | 6 (50.0) | 6 (50.0) | |
| Clinical T stage | ||||
| Tx | 13 | 8 (61.5) | 5 (38.5) | |
| T0 | 9 | 4 (44.4) | 5 (55.6) | |
| T1 | 32 | 18 (56.3) | 14 (43.8) | 0.18 |
| T2 | 80 | 34 (42.5) | 46 (57.5) | |
| T3 | 28 | 18 (64.3) | 10 (35.7) | |
| T4 | 11 | 3 (27.3) | 8 (72.7) | |
| Clinical LN status | ||||
| Negative | 65 | 38 (58.5) | 27 (41.5) | |
| Positive | 72 | 27(37.5) | 45 (62.5) | 0.02 |
| Nx | 52 | 30 (57.7) | 22 (42.3) | |
| Pathological N | ||||
| Nx | 5 | 1 (20.0) | 4 (80.0) | |
| N0 | 91 | 54 (59.3) | 37 (40.7) | |
| N1 | 49 | 18 (36.7) | 31 (63.3) | 0.04 |
| N2 | 28 | 16 (57.1) | 12 (42.9) | |
| N3 | 16 | 6 (37.5) | 10 (62.5) | |
| Relapse | ||||
| Yes | 40 | 23 (57.5) | 17 (42.5) | 0.30 |
| No | 149 | 72 (48.3) | 77 (51.7) |
Survival outcome
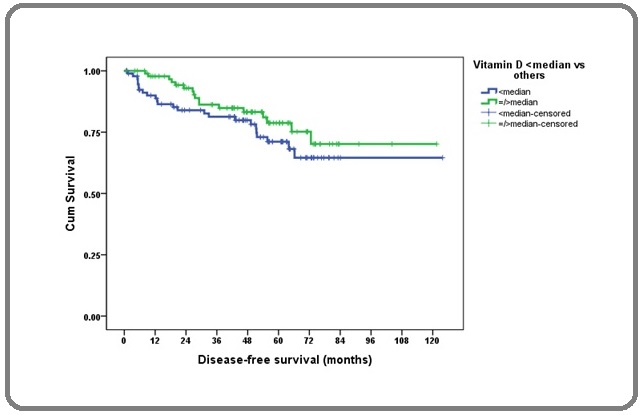
After a median follow up period of 58.2 months, 14 patients died and 40 relapsed. No difference in the rate of relapse between patients with lower vs. higher Vit-D level using different cutoffs, (Table 1). The 5-year DFS rate was 74.8%. Using 30 ng/ml as the cutoff, no difference in DFS between higher and lower Vit-D levels (73.5% vs. 75%, p=0.38) was found. Using the median as the cutoff, the 5-year DFS rates were 78.8% vs. 71.1%, in patients with higher compared to lower Vit-D levels, respectively. However, it did not reach statistical significance (p= 0.22) (Figure 1).
Figure 1: Disease-free survival of study patients according to vitamin D level.
Lower clinical (p=0.001) and pathological stages (stage I, II) (0.001) and higher BMI (p=0.04) were the only factors associated with better DFS rates. Other clinico-pathological parameters were not linked with DFS outcome (Table 2).
| Parameters | Total=189 No | 5-year DFS (%) | P |
| Body mass index | |||
| <25 | 19 | 81.7% | |
| 25-29.9 | 69 | 63.2% | 0.04 |
| 30-39.9 | 79 | 82.6% | |
| ≥40 | 22 | 79.5% | |
| Menopausal status | |||
| Premenopausal | 96 | 70.4% | 0.27 |
| Postmenopausal | 93 | 78.9% | |
| Clinical Stage | |||
| Stag I-II | 108 | 83.0% | 0.001 |
| Stage III | 69 | 66.1% | |
| Clinical T | |||
| T0-2 | 121 | 80.6% | <0.001 |
| T3-4 | 39 | 58.9% | |
| Clinical LN status | |||
| Negative | 65 | 77.1% | |
| Positive | 72 | 74.2% | 0.70 |
| Nx | 52 | 74.0% | |
| Pathology | |||
| IDC | 178 | 74.6% | |
| ILC | 7 | 60.0% | 0.42 |
| Other | 4 | 100.0% | |
| Multicentricity | |||
| Yes | 26 | 61.7% | 0.22 |
| No | 163 | 76.5% | |
| Lymphovascular invasion | |||
| Yes | 54 | 69.1% | |
| No | 127 | 77.1% | 0.11 |
| Grade | |||
| Grade 1 | 11 | 66.7% | |
| Grade 2 | 104 | 74.2% | 0.51 |
| Grade 3 | 63 | 80.8% | |
| Unknown | 11 | 62.3% | |
| ER status | |||
| Negative | 65 | 70.8 % | 0.18 |
| Positive | 124 | 76.7 % | |
| PR Status | |||
| Negative | 82 | 72.3 % | 0.40 |
| Positive | 107 | 76.5 % | |
| HER2 status | |||
| Negative | 124 | 77.9 % | |
| Positive | 62 | 70.1 % | 0.28 |
| Unknown | 3 | 0.00 % | |
| Pathological T | |||
| T0-2 | 159 | 76.2% | 0.44 |
| T3-4 | 24 | 65.2% | |
| Pathological N | |||
| N0 | 91 | 86.8 % | 0.001 |
| N+ | 93 | 62.3% | |
| Pathologic Stage | |||
| Stage 0-II | 130 | 79.6 % | 0.02 |
| Stage III | 57 | 65.2% | |
| Chemotherapy cycles Number | |||
| ≤6 | 74 | 70.6 % | 0.67 |
| >6 | 91 | 74.3 % | |
| Chemotherapy Type | |||
| Anthracycline & Taxane | 135 | 70.9 % | |
| Anthracycline only | 23 | 78.3% | 0.69 |
| Taxane only | 7 | 83.3% | |
| Vitamin D | |||
|
|
95 | 71.1% | 0.22 |
| ≥ median | 94 | 78.8% |
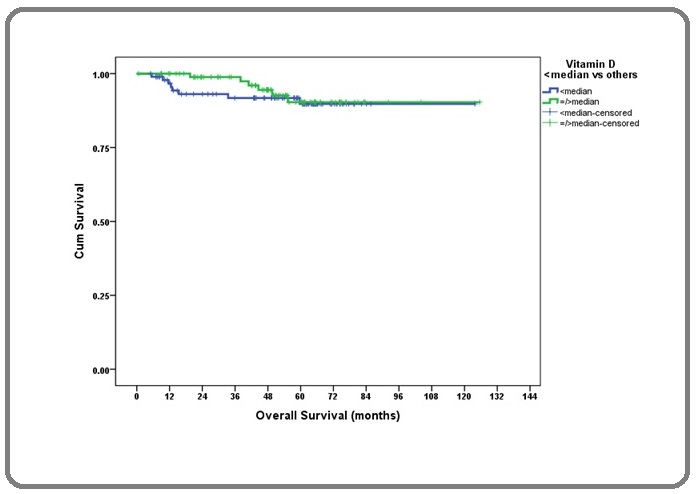
The 5-year OS rate was 90.2%. Using 30 ng/ml as the cutoff, no difference in OS between higher and lower Vit-D levels (93.5% vs. 85%, p=0.09) was found. Similarly, using the median as the cutoff, no difference in 5-year OS rate in patients with higher and lower Vit-D levels (90.3% and 89.7% respectively, p=0.6) (Figure 2).
Figure 2: overall survival of study patients according to vitamin D level.
OS was significantly higher in patients with lower pathologic stage (stage I, II), (p= 0.006). Meanwhile, no difference in OS outcome according to other clinico-pathological factors (Table 3).
| Parameters | Total 189 | 5-year OS (%) | P |
| Body mass index | |||
| <25 | 19 | 92.9% | |
| 25-29.9 | 69 | 85.3% | 0.17 |
| 30-39.9 | 79 | 91.2% | |
| ≥40 | 22 | 100.0% | |
| Body mass index | |||
| <30 | 88 | 86.7% | 0.06 |
| ≥ 30 | 101 | 93.0% | |
| Clinical Stage | |||
| Stag I-II | 108 | 92.0% | 0.16 |
| Stage III | 69 | 87.2% | |
| Pathology | |||
| IDC | 178 | 91.1% | |
| ILC | 7 | 53.3% | 0.05 |
| Other | 4 | 100.0% | |
| Menopausal status | |||
| Premenopausal | 96 | 86.6% | 0.18 |
| Postmenopausal | 93 | 93.4% | |
| Clinical T | |||
| T0-2 | 121 | 92.8% | 0.17 |
| T3-4 | 39 | 87.3% | |
| Lymphovascular invasion | |||
| Yes | 54 | 85.9% | 0.13 |
| No | 127 | 92.2% | |
| Grade | |||
| Grade 1 | 11 | 100.0% | |
| Grade 2 | 104 | 87.0% | 0.52 |
| Grade 3 | 63 | 94.9% | |
| Unknown | 11 | 87.5% | |
| Clinical LN status | |||
| Negative | 65 | 91.3% | |
| Positive | 72 | 89.0% | 0.79 |
| Nx | 52 | 91.0% | |
| ER status | |||
| Negative | 65 | 86.8 % | 0.13 |
| Positive | 124 | 91.8 % | |
| PR Status | |||
| Negative | 82 | 87.6 % | 0.21 |
| Positive | 107 | 91.8 % | |
| HER2 status | |||
| Negative | 124 | 93.3 % | |
| Positive | 62 | 85.9 % | 0.14 |
| Unknown | 3 | 0.00 % | |
| Pathological T | |||
| T0-2 | 159 | 91.1 % | 0.22 |
| T3-4 | 24 | 85.7 % | |
| Pathological N | |||
| N0 | 91 | 94.0 % | 0.09 |
| N+ | 93 | 87.5 % | |
| Pathologic Stage | |||
| Stage 0-II | 130 | 94.0 % | 0.01 |
| Stage III | 57 | 82.9 % | |
| Chemotherapy | |||
| Yes | 165 | 90.4 % | 0.95 |
| No | 24 | 86.3 % | |
| Chemotherapy cycles Number | |||
| ≤6 | 74 | 90.4 % | 0.87 |
| >6 | 91 | 90.5 % | |
| Chemotherapy Type | |||
| Anthracycline & Taxane | 135 | 89.0% | |
| Anthracycline only | 23 | 95.0% | 0.61 |
| Taxane only | 7 | 100.0% | |
| Vitamin D | |||
|
|
95 | 89.7 % | 0.60 |
| ≥ median | 94 | 90.3 % |
Discussion
In this study, we assessed the prognostic value of baseline Vit-D level in a cohort of early breast cancer patients in a single institution in Saudi Arabia. Noteworthy, the great majority of patients (89%) had low Vit-D level below the reference value and even half of the patients had considerably low values (< 14 ng/ml).This highlights the prevalence of low Vit-D levels among Saudi patients with a median age of 50 years. This points to the magnitude of the problem of low Vit-D even among this cohort of generally young healthy patients in Saudi Arabia.
Noteworthy, lower Vit-D level was significantly linked with ER-negative phenotype and premenopausal status, features generally linked with more aggressive tumour behavior. Meanwhile, higher Vit-D values were linked with clinically and pathologically-positive lymph nodes and lymphovascular invasion. This conflicting data highlights the need to explore those findings in a larger cohort of patients.
Several studies reported an association between Vit-D deficiency and poor survival. In a prospective study including 512 patients with early breast cancer, low Vit-D was significantly linked with the risk of distant recurrence and overall survival [11]. Similarly, low Vit-D level was significantly associated with poor OS and DFS in a larger cohort of 1,295 postmenopausal breast cancer patients [13]. However, despite the fact that several epidemiologic and clinical studies suggested that Vit- D deficiency may be associated with breast cancer outcome, other studies did not display any association. This may be attributed to timing of measurement of the vitamin D, stage, menopausal status and hormonal receptor status [14]. Noteworthy, the association of Vit-D level and survival outcome were assesses in two meta-analyses, involving 8 and 5 studies. These meta-analyses showed an association of low Vit-D level with recurrence in addition to overall and breast cancer-specific mortality in breast cancer patients [15][16].
In our study, Vit-D level was not linked with survival outcome. Meanwhile, almost all patients with low Vit-D, received calcium and Vit-D supplementation later on in their disease course, which may mitigate or modulate any potential prognostic value. Furthermore, only 10% of patients had normal Vit-D levels above the reference value which limits the validity of comparing the survival outcome of low vs. normal Vit-D levels in our study. Meanwhile, there was a trend towards improved DFS in those with higher Vit-D level taking the median as the cutoff. However, that analysis was actually comparing low vs. higher (but still almost lower than normal value). Furthermore, only 14 patients died among the study population, which limits assessment of OS as data is still immature for OS comparison.
In conclusion, low Vit-D level was prevalent among the studied breast cancer patients. Low Vit-D level was associated with ER-negative phenotype and premenopausal patients. Baseline Vit-D level was not significantly linked with survival outcome.
Acknowledgements
-This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
-The authors declare no conflict of interest.
References
- Vitamin D and Breast Cancer: Latest Evidence and Future Steps Atoum Manar, Alzoughool Foad. Breast Cancer: Basic and Clinical Research.2017;11. CrossRef
- Role of Vitamin D Metabolism and Activity on Carcinogenesis Wu Xiayu, Zhou Tao, Cao Neng, Ni Juan, Wang Xu. Oncology Research Featuring Preclinical and Clinical Cancer Therapeutics.2015;22(3). CrossRef
- Vitamin D signalling pathways in cancer: potential for anticancer therapeutics Deeb Kristin K., Trump Donald L., Johnson Candace S.. Nature Reviews Cancer.2007;7(9). CrossRef
- Measurement of 1,25-dihydroxyvitamin D3 receptors in breast cancer and their relationship to biochemical and clinical indices Freake HC, Abeyasekera G, Iwasaki J, Marcocci C, MacIntyre I, et al . Cancer Res.1984;44:1677-1681.
- Vitamin D and the mammary gland: a review on its role in normal development and breast cancer Lopes Nair, Paredes Joana, Costa José Luis, Ylstra Bauke, Schmitt Fernando. Breast Cancer Research.2012;14(3). CrossRef
- Interactions between vitamin D and IGF-I: from physiology to clinical practice Ameri Pietro, Giusti Andrea, Boschetti Mara, Murialdo Giovanni, Minuto Francesco, Ferone Diego. Clinical Endocrinology.2013;79(4). CrossRef
- Prognostic Role of Vitamin D Status and Efficacy of Vitamin D Supplementation in Cancer Patients: A Systematic Review Buttigliero C., Monagheddu C., Petroni P., Saini A., Dogliotti L., Ciccone G., Berruti A.. The Oncologist.2011;16(9). CrossRef
- The Association Between Breast Cancer Prognostic Indicators and Serum 25-OH Vitamin D Levels Peppone Luke J., Rickles Aaron S., Janelsins Michelle C., Insalaco Michael R., Skinner Kristin A.. Annals of Surgical Oncology.2012;19(8). CrossRef
- Triple negative breast cancer patients presenting with low serum vitamin D levels: a case series Rainville Christa, Khan Yasir, Tisman Glenn. Cases Journal.2009;2(1). CrossRef
- Prognostic value of vitamin D receptor and insulin-like growth factor receptor 1 expression in triple-negative breast cancer Soljic Martina, Mrklic Ivana, Tomic Snjezana, Omrcen Tomislav, Sutalo Nikica, Bevanda Milenko, Vrdoljak Eduard. Journal of Clinical Pathology.2017;71(1). CrossRef
- Prognostic Effects of 25-Hydroxyvitamin D Levels in Early Breast Cancer Goodwin Pamela J., Ennis Marguerite, Pritchard Kathleen I., Koo Jarley, Hood Nicky. Journal of Clinical Oncology.2009;27(23). CrossRef
- Vitamin D Deficiency is Correlated with Poor Outcomes in Patients with Luminal-type Breast Cancer Kim Hee Jeong, Lee Yu Mi, Ko Beon Seok, Lee Jong Won, Yu Jong Han, Son Byung Ho, Gong Gyung-Yub, Kim Sung Bae, Ahn Sei Hyun. Annals of Surgical Oncology.2010;18(7). CrossRef
- Serum 25-hydroxyvitamin D and postmenopausal breast cancer survival: a prospective patient cohort study Vrieling Alina, Hein Rebecca, Abbas Sascha, Schneeweiss Andreas, Flesch-Janys Dieter, Chang-Claude Jenny. Breast Cancer Research.2011;13(4). CrossRef
- Prognostic Significance of Serum Vitamin D Levels in Egyptian Females with Breast Cancer Ismail Abeer, El Awady Rehab, Abdelsalam Ghada, Hussein Marwa, Ramadan Shimaa. Asian Pacific Journal of Cancer Prevention.2018;19(2). CrossRef
- Circulating 25-hydroxyvitamin D and postmenopausal breast cancer survival: Influence of tumor characteristics and lifestyle factors? Vrieling Alina, Seibold Petra, Johnson Theron S., Heinz Judith, Obi Nadia, Kaaks Rudolf, Flesch-Janys Dieter, Chang-Claude Jenny. International Journal of Cancer.2013;134(12). CrossRef
- Serum 25-hydroxyvitamin D levels and survival in colorectal and breast cancer patients: Systematic review and meta-analysis of prospective cohort studies Maalmi Haifa, Ordóñez-Mena José Manuel, Schöttker Ben, Brenner Hermann. European Journal of Cancer.2014;50(8). CrossRef
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times