Silent High Grade Cervical Intraepithelial Neoplasia Diagnosis of Atypical Smear between Conventional and Liquid Based Papanicolaou Smear in Suburban Area of Thailand
Download
Abstract
Objectives: To evaluate the prevalence of silent high grade cervical intraepithelial neoplasia diagnose in atypical squamous cells of undetermined significance (ASC-US) in cytology result between conventional (CPP) and liquid-based cervical cytology (LBP) methods to suggest the proper management for Thai women.
Methods: This retrospective study was conducted at Bhumibol Adulyadej Hospital, Bangkok, Thailand between January 2011 and December 2016. Medical records of 28,564 patients who attended for cervical cancer screening were reviewed. Prevalence of silent high grade cervical intraepithelial neoplasia (CIN) in atypical squamous cells of undetermined significance (ASC-US) cytology result was determined
Results: During the study period, 28,564 cases were enrolled. There were 22,552 and 6,012 of CPP and LBP cases, respectively. A total of 644 cases of ASC-US cytology were enrolled. In women with ASC-US in cytology, the mean age was younger than women with negative screening cytology group and approximately 70% were in pre-menopausal status. Prevalence of high grade cervical intraepithelial neoplasia in ASC-US cytology from CPP and LBP were 9.5 and 11.9%, respectively. Ten percent (23/248) of atypical glandular cytology pattern was cancer. One-quarter of them was endometrial cancer.
Conclusion: Silent high grade cervical intraepithelial neoplasia in ASC-US cytology and the rate of cancer in atypical glandular cytology pattern were high. We recommended colposcopy for women who had the cervical cytological report as atypical squamous and glandular cytology pattern.
Introduction
The cervical cancer screening test is an important procedure to detect precancerous and cervical cancerous lesions. Cervical cancer screening can reduce the incidence of invasive cervical cancer. In Thailand, the main method of cervical cancer screening is conventional Papanicolaou test (CPP) due to its low cost which is fully supported by government health care program. Liquid-based Papanicolaou test (LBP), human papillomavirus (HPV) test, co-testing (LBP and HPV test) and HPV genotyping have been recently introduced to Thailand. These new procedures allow greater sensitivity in the detection of precancerous lesions (cervical intraepithelial neoplasia; CIN).
From several recent studies, the most common of abnormal cervical cytology were atypical squamous cells of undetermined significance (ASC-US) [1,5]. ASC-US is known as a low risk of abnormal cervical cytology. The management of ASC-US cytology of the American Society for Colposcopy and Cervical Pathology (ASCCP) is controversial [6].
In 2012, ASCCP had revised the consensus guideline for the management of abnormal cervical cancer screening tests and cancer precursors [6]. The acceptable management in women with ASC-US on cytology is either a repeat cytology at one year or an immediate HPV testing (reflex test). Colposcopy was recommended in ASC-US cases with positive result of high-risk HPV test.
From Heng’s and Lertvutivivat’s works [7,8], the ratio of prevalence of CIN 2/3 and cancer in ASC-US cytology were 16.6 to 3.5 and 0 to 1.8 percent, reported from CPP and LBP, respectively.
The objective of this study was to evaluate the prevalence of silent high grade cervical intraepithelial neoplasia (CIN 2/3 and cancer) in ASC-US cytology result between CPP and LBP methods used in our hospital to suggest the proper management based on our patient population.
Materials and Methods
The retrospective study was approved by the institutional review board, Bhumibol Adulyadej Hospital, Bangkok, Thailand (IRB: 20/61). Data were reviewed from medical records stored in a computerized program. Data from all patients with CPP and LBP in 6 years period between January 2011and December 2016 were collected. Inclusion criteria were women who had cervical cytology result with ASC-US cytology. Exclusion criteria were women with pregnancy, post hysterectomy and known history of pre-invasive or invasive cervical lesion or other gynecologic cancers. Data collected from medical records included age, type of cervical cancer test, cytology results, colposcopic examination, and histopathological reports. Demographic characteristic consisted of age, menstrual status, Pap proposal, contraception, history of the sexually transmitted disease (STD) including human immunodeficiency virus (HIV), history of multiple partners, occupation, smoking, and alcohol consumption. Management of ASC-US cytology was followed by the previous ASCCP guideline by either a repeated cervical cytology testing in 6 months or a colposcopic directed biopsy (immediate colposcopy or positive high-risk HPV test). Descriptive statistics were used to analyze patient demographic data. Continuous data were expressed as the mean and standard deviation (SD). Categorized data were expressed as number and percentage. Pearson Chi-square and Fisher’s exact test were used in data analysis when appropriate. The p value of 0.05 or less was considered to be statistically significant. The analysis was performed using the SPSS statistic version 18 (SPSS, Chicago, IL, USA).
Results
This study was conducted in the Headquarter of the Royal Thai Air Force Hospital. Around one-fifth of the population in this study were air force personals and their families. The remaining patients were people who lived and worked in the nearby area around this air force base. Patients also came from a wholesale market, Talad Si Mum Muang, located in a nearby area.
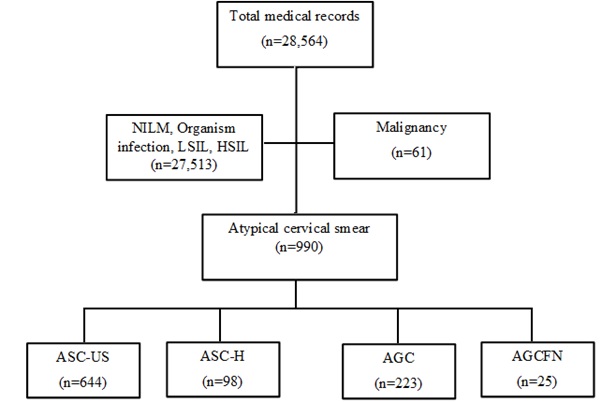
A total of 28,564 medical records were reviewed during the study period. There are 22,552 and 6,012 cases in CPP and LBP groups, respectively. A total of 990 atypical cervical cytology cases were enrolled. Only 644 cases of atypical smears cases were ASC-US reports. Other atypical squamous cells smears not included were high grade squamous intraepithelial lesion (ASC-H), atypical glandular cells (AGC) and atypical glandular cells favor neoplasia (AGCFN) at 98, 223 and 25 cases respectively (Fig. 1).
Figure 1 :. Medical Records Reviewed in this Study. NILM, negative for intraepithelial lesion or malignancy; LSIL, low-grade squamous intraepithelial lesion; HSIL, high-grade squamous intraepithelial lesion; ASC-US, atypical squamous cells of undetermined significance; ASC-H, atypical squamous cells cannot exclude high grade squamous intraepithelial lesion; AGC, atypical glandular cells; AGCFN, atypical glandular cells favor neoplasia.
Tabl 1 showed the demographic characteristic of participants in this study. There are 23,009 and 644 cases in NILM and ASC-US groups, respectively. The participants in ASC-US group had a lower age than the control group with statistically significant. The mean age of women with ASC-US versus NILM in cytology were 41.03 and 46.28 years, respectively. The clients in ASC-US also had significantly higher percentage of the multiple sexual partners and pre-menopausal status than the control group. Three-quarters of ASC-US cases (460/644) were in premenopausal status.
| Characteristics | NILM (n = 23,009) | ASC-US (n = 644) | p -value | |
| Age (years)* | 46.28 + 12.93 | 41.03 + 14.44 | 0.001*** | |
| Menstrual status** | 0.004*** | |||
| Pre-menopause | 13,115 (57.0) | 460 (71.4) | ||
| Menopause | 9,894 (43.0) | 184 (28.6) | ||
| Pap proposal** | 0.547 | |||
| Check up | 18,867 (82.0) | 541 (84.0) | ||
| AUB | 0 (0) | 7 (1.1) | ||
| Postpartum | 3,681 (16.0) | 63 (9.8) | ||
| Leukorrhea | 0 (0) | 4 (0.6) | ||
| Pelvic pain | 461 (2.0) | 16 (2.5) | ||
| Follow up | 0 (0) | 13 (2.0) | ||
| Contraception** | 0.017*** | |||
| None | 21,859 (95.0) | 541 (84.0) | ||
| Barrier | 0 (0) | 18 (2.8) | ||
| COC | 0 (0) | 30 (4.7) | 0.024*** | |
| Others | 1,150 (5.0) | 55 (8.5) | ||
| HIV** | 0.607 | |||
| Yes | 0 (0) | 8 (1.2) | ||
| No | 23,009 (100) | 636 (98.8) | ||
| Multiple partner** | 0.039*** | |||
| Yes | 23 (0.1) | 27 (4.2) | ||
| No | 22,986 (99.9) | 617 (95.8) | ||
| Smoked** | 0.176 | |||
| Yes | 230 (1.0) | 3 (0.5) | ||
| No | 22,779 (99.0) | 641 (99.5) | ||
| Alcohol consumption** | 0.536 | |||
| Yes | 276 (1.2) | 6 (0.9) | ||
| No | 22,733 (98.8) | 638 (99.1) | ||
| Cytology technique** | 0.076 | |||
| CPP | 18,274 (79.4) | 493 (76.6) | ||
| LBP | 4,735 (20.6) | 151 (23.4) |
a) *: mean + SD (standard deviation), b) **: n (%), c) ***: The result is significant at p < .05, NILM: negative for intraepithelial lesion or malignancy, ASC-US: atypical squamous cells of undetermined significance, AUB: abnormal uterine bleeding, COC: combined oral contraceptive pills, HIV: human immunodeficiency virus, CPP: conventional Pap smear, LBP: liquid based Pap smear.
The histopathological reports of atypical cervical cytology were represented in Tabl 2. The prevalence of less than or equal to CIN 1 and CIN 2 or higher in ASC-US reports was 90.5/88.1 and 9.5/11.9 percent in CPP and LBP groups, respectively. Ten percent (23/248) of atypical smear containing glandular cells types were cancerous. One-quarter of them was endometrial cancer.
| Cervical cytology | CPP * | LBP * | N | |||||
| ≤ CIN 1 | CIN 2/3 | Cancer | ≤ CIN 1 | CIN 2/3 | Cancer | |||
| ASC-US | 264 (90.5) | 20 (6.8) | 8 (2.7) | 74 (88.1) | 9 (10.7) | 1 (1.2) | 376 | |
| ASC-H | 61 (80.3) | 10 (13.1) | 5 (6.6) | 16 (72.7) | 4 (18.2) | 2 (9.1) | 98 | |
| AGC | 144 (89.4) | 7 (4.4) | 10 (6.2) | 55 (88.7) | 2 (3.2) | 5 (8.1) | 223 | |
| AGCFN | 11 (50) | 4 (18.2) | 7 (31.8) | 1 (33.3) | 1 (33.3) | 1 (33.3) | 25 | |
| Total | 480 | 41 | 30 | 146 | 16 | 9 | 722 |
a) *n(%), ASC-US: atypical squamous cells of undetermined significance, ASC-H: atypical squamous cells cannot exclude high grade squamous intraepithelial lesion, AGC: atypical glandular cells, AGCFN: atypical glandular cells favor neoplasia, ≤ CIN 1: cervical intraepithelial neoplasia grade 1 or less, CIN 2/ 3: cervical intraepithelial neoplasia grade 2 and 3, CPP: conventional Pap smear, LBP: liquid based Pap smear
| Watson | Ryu | Marcos | Heng | Lertvutivivat | Petousis | Present | |||
| Year | 2015 | 2015 | 2016 | 2016 | 2016 | 2017 | 2018 | ||
| Country | Columbia | Korea | Brazil | Thailand | Thailand | Greece | Thailand | ||
| Type | LBP | CPP | LBP | CPP | LBP | ||||
| Number | 993,238 | 40,608 | 2,144 | 22,552 | 6,012 | ||||
| ASC-US * | 45,049 (4.5) | 3,223 (8.0) | 703 | 187 | 65 (3.0) | 134 | 493 (2.2) | 151 (2.5) | |
| Colposcopy | 14.6 | 32 | 100 | 100 | 100 | 100 | 59.2 | 55.6 | |
| HPV test | 62.8 | 100 | 4 | ||||||
| F/U Pap | 8.6 | 7.5 | 15.9 | ||||||
| loss F/U | 33.3 | 28.5 | |||||||
| Diagnosis | |||||||||
| Normal | 40.2 | 63.7 | 90 | 50.8 | 80.7 | 39.6 | 52.1 | 39.3 | |
| CIN 1 | 46.5 | 19.3 | 7.3 | 32.6 | 14 | 33.6 | 38.4 | 48.8 | |
| CIN 2/3 | 11.8 | 16.4 | 2.7 | 16.6 | 3.5 | 26.8 | 6.8 | 10.7 | |
| Cancer | 0.2 | 0.6 | 0 | 0 | 1.8 | 0 | 2.7 | 1.2 |
a) *n(%), ASC-US: atypical squamous cells of undetermined significance, HPV: human papillomavirus, F/U: follow up, CIN 1: cervical intraepithelial neoplasia grade 1, CIN 2/3: cervical intraepithelial neoplasia grade 2 and 3, CPP: conventional cervical Pap smear, LBP: liquid based cytology
Discussion
ASC-US is the most common cytological abnormality in cervical cytology. It carried the lowest risk of CIN 3 or cancer because one third to two third was not HPV associated [9]. From ASCCP guideline, there was three tier of management in the women who had ASC-US cytological reports, namely repeat cervical cytology, immediate colposcopy, and HPV testing. The women who had positive HPV testing for high risk with ASC-US reports would undergo colposcopic directed biopsy. From the ASCCP 2012 consensus, the management of women with ASC-US on cytology is a repeat cytology at one year or an HPV testing. For women with HPV-positive ASC-US, either from reflex HPV testing or co-testing, a colposcopy is recommended. Repeat co-testing at one year was recommended in women with HPV-negative ASC-US, whether it was from reflex HPV testing or co-testing. Immediate colposcopy was not further recommended because ASC-US had less than 3 percent CIN 3 or cancer development in 5 year period [9].
In the present study, the prevalence of CIN 2/3 and cancer in ASC-US cytology were 9.5 and 11.9% from CPP and LBP group, respectively. From the previous investigations, the prevalence of CIN 2/3 and cancer were between 5.3-26.8 percent [7,8, 10,12]. The result of our study supported the former studies. In this study, the prevalence of CIN 2+ from either CPP or LBP was no statistical difference (p = 0.752).
Colposcopy with direct biopsy is a gold standard method for diagnosis of pre or invasive cervical cancer. During the study period, the management of ASC-US cytology was conducted based on previous ASCCP guideline. The ASC-US cases were undergoing repeat cervical cytology, immediate colposcopy, and colposcopy after the positive result of the high-risk HPV test. In our study, more than half (376/644) of ASC-US cases underwent colposcopic directed biopsy. Most physicians preferred to repeat cytology as a follow-up method due to its economical expense and ease of operation in Thailand. The sensitivity and specificity of CPP and LBP for the detection of CIN 2/3 and cancer were approximately 55.2 to 57.1 and 96.7 to 97.0 percent, respectively [13]. Our study revealed 80% of participants received CPP for cervical cancer screening.
HPV testing had higher accuracy than repeat cytology method. It led to faster and more complete diagnosis of pre and invasive cervical diseases. Cuzick’s work showed that in women with ASC-US cytology, time to CIN3+ detection was much shorter in women with HPV testing than without testing [14].
Nowadays HPV testing has not been performed as a primary screening test in government hospitals. Limitation of its usage was its higher expense, and a copayment was needed in a government health setting. From another Thai hospital study, women with ASC-US cytology had a 40 percent risk of HPV [8]. In the present study, four percent (26/644) of the patient with ASC-US in cytology underwent HPV testing. Half of HR-HPV test in ASC-US cases had the positive result. All cases of ASC-US with positive or negative HR-HPV testing had no CIN2+.
In this study, the finding suggested all patients with ASC-US cytology from both methods for cervical screening (CPP vs LBP) should undergo immediate colposcopic directed biopsy. This suggestion was not following the latest ASCCP guideline because our finding showed a high prevalence of high grade cervical intraepithelial lesions (CIN 2+) (9.5 to 11.9 %). Our result is similar to previous works done in Thailand [8, 15,16]. Our data showed that the silent of CIN2+ in ASC-US group was as high as LSIL group. The suggestion from this study did not follow the latest guideline of ASCCP. The ASCCP guideline was created on the data of the populations whose had the lower incidence of cervical cancer than the present study population.
In this study, ten percent (23/248) of atypical smear containing glandular cells types were cancerous. One-quarter of them was endometrial cancer. From the previous study, AGC in women at age of 35 or older usually contained cancer around 3% compared to 10 % in this study [17]. This report showed the higher prevalence of cancer. This study supported the recommendation of colposcopy and endometrial biopsy followed by ASCCP guideline.
In conclusion, the silent high-grade CIN in ASC-US cases was higher than the data of the ASCCP guideline. Based on our patient population, we recommended colposcopy in the women who had cervical cytology report of ASC-US without HPV testing result and AGC. The suggestion might be applied to the referral center that the incidence of silent high-grade CIN was high.
References
[1]. Laiwejpithaya S, Rattanachaiyamont M, Benjapibal M, Khuakoonratt N, Boriboonhirunsarn D, Laiwejpithaya S, et al. Comparison between Siriraj liquid-based and conventional cytology for detection of abnormal cervicovaginal smears: a split-sample study. Asian Pac J Cancer Prev 2008; 9(4): 575-80.
[2]. Tanabodee J, ThepsuwanK, Karalak A, Laoaree O, Krachang A, Manmatt K, et al. Comparison of Efficacy in Abnormal Cervical Cell Detection between Liquid-based Cytology and Conventional cytology. Asian Pac J Cancer Prev 2015;16(16): 7381-4.
[3]. Kingnate C, Tangjitgamol S, Khunnarong J, Manusirivithaya S. Abnormal uterine cervical cytology in a large tertiary hospital in Bangkok metropolis: Prevalence, management, and outcomes. Indian J cancer 2016; 53(1): 67-73.
[4]. Mu-Mu-Shwe, Harano T, Okada S, Aye-Aye-Win, Khin-Saw-Aye, Hlaing-Myat-Thu, et al. Prevalence of high-risk human papillomavirus (HR-HPV) infection among women with normal and abnormal cervical cytology in Myanmar. Acta Med Okayama 2014; 68(2): 79-87.
[5]. Hav M, Eav S, Heang N, Pich P, Lim D, Leung V, et al. Prevalence of Abnormal Cervical Cytology in HIV Negative Women Participating in a Cervical Cancer Screening Program in Calmette Hospital, Cambodia. Asian Pac J Cancer Prev 2016; 17(7): 3101-3.
[6]. Massad LS, Einstein MH, Huh WK, Katki HA, Kinney WK, Schiffman M, et al. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis 2013; 17(5): s1-27.
[7]. Heng S, Sirichaisutdhikorn D. Incidence of High-Grade Squamous Intraepithelial Lesions in Patients with Atypical Squamous Cells of Undetermined Significance Papanicolaou Smears at Naresuan University Hospital. Asian Pac J Cancer Prev 2016; 17(5): 2411-4.
[18]. Lertvutivivat S, Chanthasenanont A, Muangto T, Nanthakomon T, Pongrojpaw D, Bhamarapravatana K, et al. Silent High-Grade Cervical Intraepithelial Neoplasia in Atypical Smears from Liquid-Based Cervical Cytology: Three Years Experience in Thammasat University Hospital. Asian Pac J Cancer Prev 2016; 17(9): 4353-6.
[19]. Katki HA, Schiffman M, Castle PE, Fetterman B, Poitras NE, Lorey T, et al. Five-year risks of CIN 3+ and cervical cancer among women with HPV testing of ASC-US Pap results. J Low Genit Tract Dis 2013; 17(5): s36-42.
[20]. Watson M, Nenard V, Lin L, Rockwell T, Royalty J. Provider management of equivocal cervical cancer screening results among underserved women, 2009-2011: follow-up of atypical squamous cells of undetermined significance. Cancer causes control 2015; 26(5): 759-64.
[21]. Ryu K, Lee S, Min K, Kim JW, Hong JH, Song JY, et al. Reflex human papillomavirus test results as an option for the management of Korean women with atypical squamous cells cannot exclude high-grade squamous intraepithelial lesion. Oncologist 2015; 20(6): 635-9.
[22]. Petousis S, Kalogiannidis I, Margioula-Siarkou C, Mamopoulos A, Mavromatidis G, Prapas N, et al. Cumulative High-Grade Squamous Intraepithelial Lesion Rate and Need for Surgical Intervention of Atypical Squamous Cells of Undetermined Significance Cytology-Diagnosed Patients: A Prospective Study. Gynecol Obstet Invest 2017; 82(3): 247-51.
[23]. Arbyn M, Bergeron C, Klinkhamer P, Martin-Hirsch P, Siebers AG, Bulten J. Liquid compared with conventional cervical cytology: a systemic review and meta-analysis. Obstet Gynecol 2008; 111(1): 167-77.
[24]. Cuzick J, Myers O, Lee JH, Shi Y, Gage JC, Hunt WC, et al. Outcomes in women with cytology showing atypical squamous cells of undetermined significance with vs without human papillomavirus testing. JAMA Oncol 2017; 3(10): 1327-34.
[25]. Tantitamit T, Termrungruanglert W, Oranratanaphan S, Niruthisard S, Tanbirojn P, Havanond P. Cost-effectiveness analysis of different management strategies for detection CIN2+ of women with atypical squamous cells of undetermined significance (ASC-US) Pap smear in Thailand. Asian Pac J Cancer Prev 2015; 16(16): 6857-62.
[26]. Perksanusak T, Sananpanichkul P, Chirdchirm W, Bhamarapravatana K, Suwannarurk K. Colposcopy requirement of Papanicolaou smear after atypical squamous cells of undetermined significance (ASC-US) by follow-up protocol in an urban gynaecology clinic, a retrospective study in Thailand. Asian Pac J Cancer Prev 2015; 16(12): 4977-80.
[27]. Katki HA, Schiffman M, Castle PE, Fetterman B, Poitras NE, Lorey T, et al. Five-year risks of CIN 3+ and cervical cancer among women with HPV-positive and HPV-negative high-grade Pap results. J Low Genit Tract Dis. 2013; 17(5): s50-5.
[28]. Marcos Lopes AC, Campener AB, Henrique LQ. Prevalence of High-Grade Intraepithelial Neoplasia in Patients with Cytology Presenting Atypical Squamous Cells of Undetermined Significance. Acta Cytol. 2016; 60(2): 139-44.
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times