Cancer Pain Management in the Era of COVID-19 Pandemic: Concerns and Adaptation Strategies
Abstract
Pain is a troublesome issue in most of the cancer patients. Under treatment of pain can lead to poor quality of life in them. Thus, it is important to maintain continuity of cancer pain management even during a pandemic situation. In literature, the strategies for adopting the cancer pain management practices in light of current scenario of pandemic are not described. The outbreak of Novel corona virus infection (COVID-19) has imposed multiple challenges including restriction of access to routine health care system, psychological stress and impositions of strict infection control strategy. In this narrative review, we discuss the potential considerations of conventional cancer pain management model during outbreak of COVID -19. Effects of common analgesics on immune system have been described backed by evidence in literature. We provide a few strategies for the cancer pain management practices, which can be adopted during the pandemic. They are prioritization of patients for in-hospital visit, considering bi logical interactions and legal limitations while prescribing medications, considering only urgent cases for pain interventions and providing a holistic care with use of digital technology. Further good quality randomized controlled trials and formulation of international consensus guidelines is the need of the hour and is highly recommended.
Introduction
Cancer is a major global health problem. As per the World Health Organization (WHO) cancer is the second leading cause of death all over the world [1]. Majority of these patients live with chronic pain due to malignancy. Almost 50% patients with malignancies and 70% patients with advanced malignancies live with the curse of cancer pain [2-3]. Among these, 50% patients suffer from moderate to severe pain, while 25% suffer from more severity of pain [4-6]. Oncological treatments are also associated with acute pain syndromes in cancer patients with chronic pain, e.g. post chemotherapy oral mucositis, chemotherapy induced peripheral neuropathy, radiotherapy induced bone pain, intervention related pain after biopsy or surgery etc [7]. Cancer pain is a complex pathophysiological process. Its exact aetiology is still uncertain, but there are multiple possible mechanisms behind it. It involves visceral, somatic and neurogenic components [8]. Thus the management requires a step wise multimodal therapies to control this complex process. But often our cancer patients remain undertreated for their pain. As per the review of existing literature by Deandrea (2008) nearly one of two patients has under treatment of cancer pain [9]. This under treatment of pain leads to a poor quality of life in cancer patients [10]. Thus managing pain is a priority in cancer patients not only for physical well-being but also for psychological and ethical needs of the patients.
Unfortunately, we are standing amidst a pandemic right now. On 11th March, 2020 the World Health Organization (WHO) has declared the outbreak of novel corona virus (COVID-19) as a global pandemic [11]. Aggressive contact tracing, identifying infected people and maintaining social distance are the major strategies for containment of infection. Many nations have imposed strict lockdown measures, which has made the access to the conventional health care systems difficult for the patients. Routine practice for cancer patients has also curtailed down in view of less manpower and to decrease footfalls of patients in the hospitals [12]. Only high priority patients are considered for routine or emergency oncological treatments [13]. Similarly we need to analyse the conventional cancer pain management approach in light of this pandemic situation. This can help to formulate a strategy to maintain continuity of pain management in cancer patients during a pandemic.
We performed a literature search through common search engines, e.g. Medline, Cochrane library and Google scholar using the following key words: ‘Cancer’, ‘pain’, ‘COVID-19’, ‘Pandemic’. We could not identify any consensus guidelines or documents describing the concerns and changes in practice for cancer pain management in the context of recent or old pandemics. Thus we here present a narrative review on the aspects of conventional cancer pain management which can be potentially affected by the current pandemic situation. We also suggest some adaptation strategies which can be helpful for a cancer pain management centre.
Conventional model of cancer pain management
The cornerstone of traditional management of cancer pain is a pain ladder proposed by the WHO in the year of 1986 [14-15]. It was a three step ladder (Figure 1) for control of cancer pain [16]. In the first step, the treatment begins with a non-opioid medication.
Figure 1: The Original World Health Organization Pain Ladder (Adopted from World Health Organization, 1987).
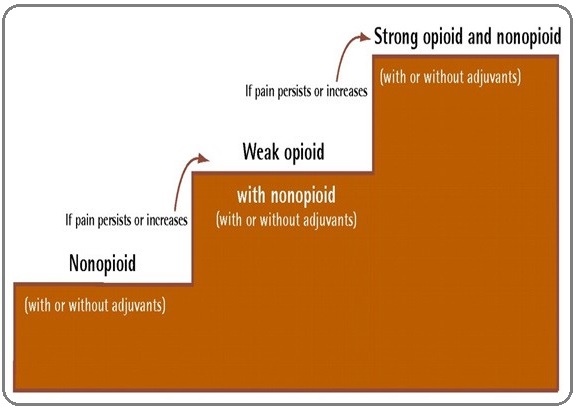
If not controlled, one needs to proceed to the second step to prescribe weak opioids along with non-opioids analgesics with or without adjuvants. If the pain is still uncontrolled, one can move towards the thyroid step where strong opioids can be prescribed and with adjuvants and non-opioids analgesics. The basic principle of prescribing drugs for cancer pain is:
• It should be by the mouth preferably.
• IT should be prescribed round the clock.
• It should be individualized.
• It should be titrated according to the individual patient’s pain score.
Over the past three decades, this ladder approach has been criticized and modified in many ways. One of the major adaptations is the addition of a fourth step to the ladder (Figure 2) advocating use of interventional pain procedures as appropriate [17].
Figure 2:New Adaptation of WHO Pain Ladder (Vargas-Schaffer G (2010), Reprinted with permission).
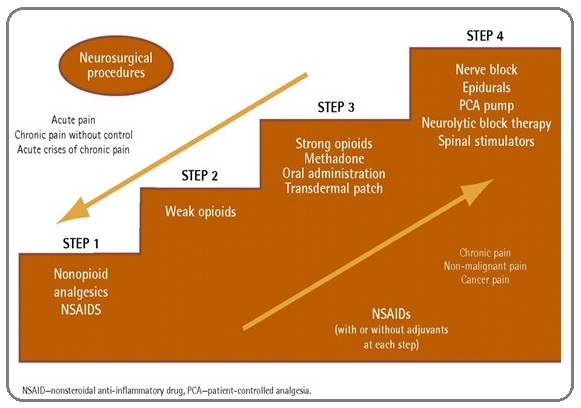
These interventions include invasive techniques, neurolysis, neuraxial implants, neurosurgical techniques etc. This bidirectional ladder approach helps the physicians to manage acute pains associated with cancer along with chronic pain [17]. Later, debate sprouted for use of an intervention at an early stage of cancer pain. Amr and Makharita (2014) performed sympathetic plexus nerve blocks for inoperable abdomino-pelvic malignancies at an early stage, before the second stage of WHO ladder [18]. They found it had a better control of pain, lesser opioid requirements and better quality of life as compared to those patients who were treated with the conventional therapies. But, there is lack of large scale quality trial which proves benefits of early integration of invasive pain procedures in cancer patients. So, the most practiced approach is to start with a conventional approach and gradually opt for a more invasive procedure. Individualized strategies for interventional pain management at an early stage of cancer pain is highly desirable [19].
Among the medications, the most commonly used drugs for cancer pain can be divided into three categories: Opioids, non-opioids and adjuvant analgesics. The opioids again can be classified into two for practical purposes: a weak opioid for step 2 and a strong opioid for step 3.The weak opioids which can be used in step 2 are: tramadol [20], codeine [21] and tapentadol [22]. The strong opioids include morphine, methadone [23], fentanyl [24] , buprenorphine [25] etc. Though the oral preparations are preferred, other preparations have also been found useful for managing moderate to severe cancer pain, e.g. intravenous, subcutaneous [26], sublingual [27] or transdermal [28].
The non-opioid analgesics are being prescribed at all the steps of the ladder from 1 to 3 [29]. The two such common drugs are acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDS). The NSAIDS are particularly useful for somatic and bone pain due to its anti-inflammatory action [30]. But, unfortunately it has some side effect profiles, e.g. Gastrointestinal bleeding, thrombocytopenia etc [30]. In such patients with refractory bone pain, a palliative radiotherapy should be considered [31]. The third class of drugs used for managing cancer pain are various adjuvant drugs. These drugs with multiple mechanisms of actions have been found especially useful for a neuropathic or mixed type cancer pain. Some of these are anxiolytics, antidepressants [32] antiepileptic [33], N-methyl-d-aspartate (NMDA) receptor antagonists [34], steroids, cannabinoids [35] etc.
Biophysiological considerations of conventional cancer pain management during COVID 19 outbreak
Cancer patients are at high risk of COVID-19 infection. In a nationwide analysis in China by Liang et al, 2020 showed that patients with cancers have a higher incidence (1% vs. 0.29%) of severe COVID-19 infection than general population [36]. In another multicentric study[37] cancer patients were found to have higher overall 30 days mortality and it was associated with risk factors specific to cancer. Thus, any therapy in cancer patients including pain management needs special considerations regarding their immunomodulatory effect. A negative immunomodulatory effect is to be avoided as it may lead to a high viral load and more complications in cancer patients. Thus, we here focus on possible immune interactions of common pain medications described in literature.
1. Opioids
Opioids are the backbone of managing moderate to severe cancer pain. But their effect on immune system remains controversial. Long term therapy with opioids for chronic pain has been found to supress the immune system [38]. Long term opioid abusers also have been found to have an increased rate of infections [39]. Multiple mechanisms of immunosuppression by exogenous has been suggested e.g. interaction with both innate and acquired immunity [40], effect on hypothalamic pituitary adrenal axis [41], effect on endocrinal systems [42] etc. Large dose and prolonged duration of therapy with opioids have a more pronounced effect on endocrinal system [43]. Different opioids have different effect on immune system. Morphine [44] and Fentanyl [45] suppress the immunity the most; whereas Buprenorphine has a better response in immunocompromised persons [46]. Large dose and prolonged duration of therapy with opioids have a more pronounced effect on endocrinal and immune system [43]. Thus, we can conclude that one needs to be cautious with the patients on high dose of chronic opioids therapy for cancer pain. They need to follow the preventive precautions from Covid-19 infection more stringently.
2. Non Opioid Analgesics:
NSAIDS are widely used for somatic and bone pain related to cancers. There are some controversies regarding use of NSAIDS in COVID patients. In large trials, NSAIDS have been found to increase the complications due to respiratory infection [47]. Indomethacin, a potent NSAIDS, potentiates the expression of the angiotensin converting enzymes (ACE2) and is hypothesized to increase the COVID-19 infection [48]. In a contrasting study result, indomethacin was found to supress viral load in vivo and in vitro against COVID 19 [49]. In hospitalized patients with COVID-19, a high proportion of patients are at high risk of developing AKI [50] due to fever and dehydration. This can be accentuated by the nephrotoxic property of NSAIDS [51]. Though inference from existing indirect links in the literature suggests a caution for use of NSAIDS in COVID-19 patients [52] there is no direct evidence of harmful effect of NSAIDS in COVID-19 patients.
3. Adjuvant analgesics
Steroids are useful adjunct to treat pain related to neuropathy [53], radiation induced pain flare [54], brain metastasis [55] and spinal cord compression [56]. Though steroids showed positive impact on immune system in majority of the literature [57-58], in some studies it showed an increase in viral load [59-60]. Thus it needs to be used with caution in suspected or confirmed COVID-19 cases.
Therapeutic concerns and adaptation strategies for managing cancer pain
As managing pain is a priority in cancer patients, we need to adapt to some strategies based on the concerns involving biophysiological interactions of analgesics and challenges imposed on systems due to pandemic. The basic principle for these strategies are minimizing the risk of infection in patients without affecting the pain management to its minimum. A summary of recommendations for adaptation strategies are presented in Table 1.
| Strategies for cancer pain managment during COVID-19: |
| Strategies for in-hospital visits |
| · Prioritize patients for in-hospital visits. |
| · Postpone all elective non-urgent pain procedures. |
| · Use telemedicine to its full capacity for triaging priority patients |
| · Consider telemedicine over face to face interaction, whenever possible. |
| ·Adhere to the national, local and institutional legal and ethical guidelines for practice of telemedicine. |
| Prescribing Opioids: |
| ·Don’t change the on-going opioid treatment regimen without significant change in pain intensity or functional status. |
| ·Use real time visual modalities of telemedicine, whenever is feasible to assess the compliance, monitoring of on-going opioid therapy and to assess the need to initiate opioids. |
| · Always document in the medical records during every visits (telemedicine and in-hospitals visits) |
| · Follow national, local or institutional policies for providing e-prescriptions of opioids. |
| · Any patient, who needs initiation of opioid therapy or change from one opioid to another, needs to have an in-hospital visit. |
| ·For institutional dispensing of opioids, identify a key caregiver during teleconsultation and ask him to come to centre to collect the drugs. If the pain is stable, dispense at least drugs for 30 – 60 days. |
| · Any patients on opioids for cancer pain should be provided with an institutional emergency 24*7 helpline number. |
| ·Educate patients and caregivers about potential side effects of opioids, including risk of infection; educate them for maintenance of hygiene and infection control strategies. |
| · Be extra careful for patients with fentanyl patch. If a patient develops fever, the patch should be removed and family should contact the emergency helpline number immediately. |
| Prescribing NSAIDS: |
| · Should be prescribed and continued in adherence with WHO pain ladder. |
| · Educate the patient to report immediately over emergency telephone helpline number if there is new onset fever or myalgia. |
| Prescribing steroids: |
| · Continuing or starting new steroid therapy for pain management in cancer patient should be individualized strategy based on benefits and risk of infection. |
| · Use dexamethasone or betamethasone whenever needed. |
| · Avoid use of steroids as adjuvants in neurolytic blocks and neuraxial administration. |
| Procedural considerations: |
| · Take up only urgent cases for pain intervention. |
| · All patients should be screened for symptoms and epidemiological link of COVID 19 before procedure. |
| · Follow local or institutional guidelines for RT-PCR testing of COVID 19 before the procedure. |
| ·For COVID negative or low risk cases, perform in non covid area and for COVID positive or high risk cases perform the procedure at a designated COVID area of hospital. |
| · Use proper and adequate personal protective equipment (PPE). |
| · Minimize movement of staffs in the room. |
| · Use disposable items; don’t bring trolley into the room. |
| · Cover all the reusable equipment in plastic covers. |
| · If general anaesthesia is required, take all precautions to minimize aerosolization. |
| Plan of palliative radiotherapy : |
| · Use single fraction (8Gy,1#) palliative radiotherapy, whenever needed for bony pain. |
| Psychosocial support: |
| · Use telemedicine and online platforms to provide access to peer support group. |
| · Involve patients on online cognitive behavioural therapy sessions from experts. |
| · Maintain physical distance instead of a social distance with family members. |
| · Refrain from panic creating social media and news. |
The major strategies are described below:
1. Prioritization of patients for in hospital visits
Decreasing the daily footfalls of patients and caregivers in hospitals for routine follow up during the on-going pandemic is important. This mandates to create a triaging method for choosing the high priority patients for managing cancer pain in the hospital setting. The high priority patients with cancer pain can be categorized as acute pain syndromes, chronic pain syndromes and acute on chronic pain syndromes (Table 2).
| Acute Pain | Acute on Chronic Pain | Chronic Pain |
| 1. Severe (NRS>7/10) pain arising from treatment of anticancer treatments : | 1. Severe breakthrough pain (NRS>7/10), not subsided by oral rescue doses. | 1. New onset of opioid therapy. |
| · Grade 3 and 4 oral mucositis.*1 | 2. Severe (NRS>7/10) pain related to tumour: | 2. Change over from one opioid to another. |
| · Chemotherapy induced peripheral neuropathy WHO*2 grade 3 or 4 | · Impending vertebral collapse. | 3. Refilling of opioids. (In hospital visit at least by care giver after real time teleconsultation). |
| ·Acute post chemotherapy enterocolitis. | · Pathological fracture. | 4. Patients with side effects of opioids, e.g. respiratory depression, sedation, severe nausea and vomiting not controlled by oral medications, severe constipation not relieved by usual drugs etc. |
| ·Acute radiation induced bone pain. | · Hollow viscus perforation. | 5. Patients on fentanyl patch, having fever. |
| · Radiation induced plexopathies. | · Malignant bowel obstruction. | 6. Patients requiring urgent pain interventions: |
| · Radiation induced proctitis. | · Large malignant ascites. | • Intrathecal pump (ITP) failure, displaced or disconnection causing inadequate delivery. |
| · Acute pain flare after hormonal therapy Extravasation of cytotoxic agents. | · Raised intracranial tension in brain metastasis. | • ITP refill with medications and before expiry of battery life to prevent withdrawal symptoms |
| 2. Severe (NRS>7/10) pain arising from interventions : | · Haemorrhage, infection in tumour. | • Infection of the implants. |
| · Acute severe postoperative pain. | · Invasion of tumour into bone. | |
| · Biopsy | 3. Severe (NRS>7/10) pain related to analgesics: Opioid induced hyperalgesia. | |
| · Thoracocentesis. Catheter insertion. |
*1, Toxicity grading of oral mucositis (OM) according to World Health Organization (WHO) and National Cancer Institute Common Toxicity Criteria (NCI-CTC) criteria [83]; *2 Oncoprof. WHO toxicity scale. 2009 [84].
Some of the examples of such high priority patients for cancer pain management are as follows, but not limited to:
• Acute exacerbation of chronic pain (Numeric rating scale [NRS]>7/10), not controlled by oral therapy.
• Patients with impending spinal cord compression.
• New onset pathological fracture.
• Severe Pain following an oncological treatment.
• Patients having side effect of the pain therapies, e.g.:
overdose of opioids.
• An intrathecal pump disconnection or displaced.
• An infected pain device implant.
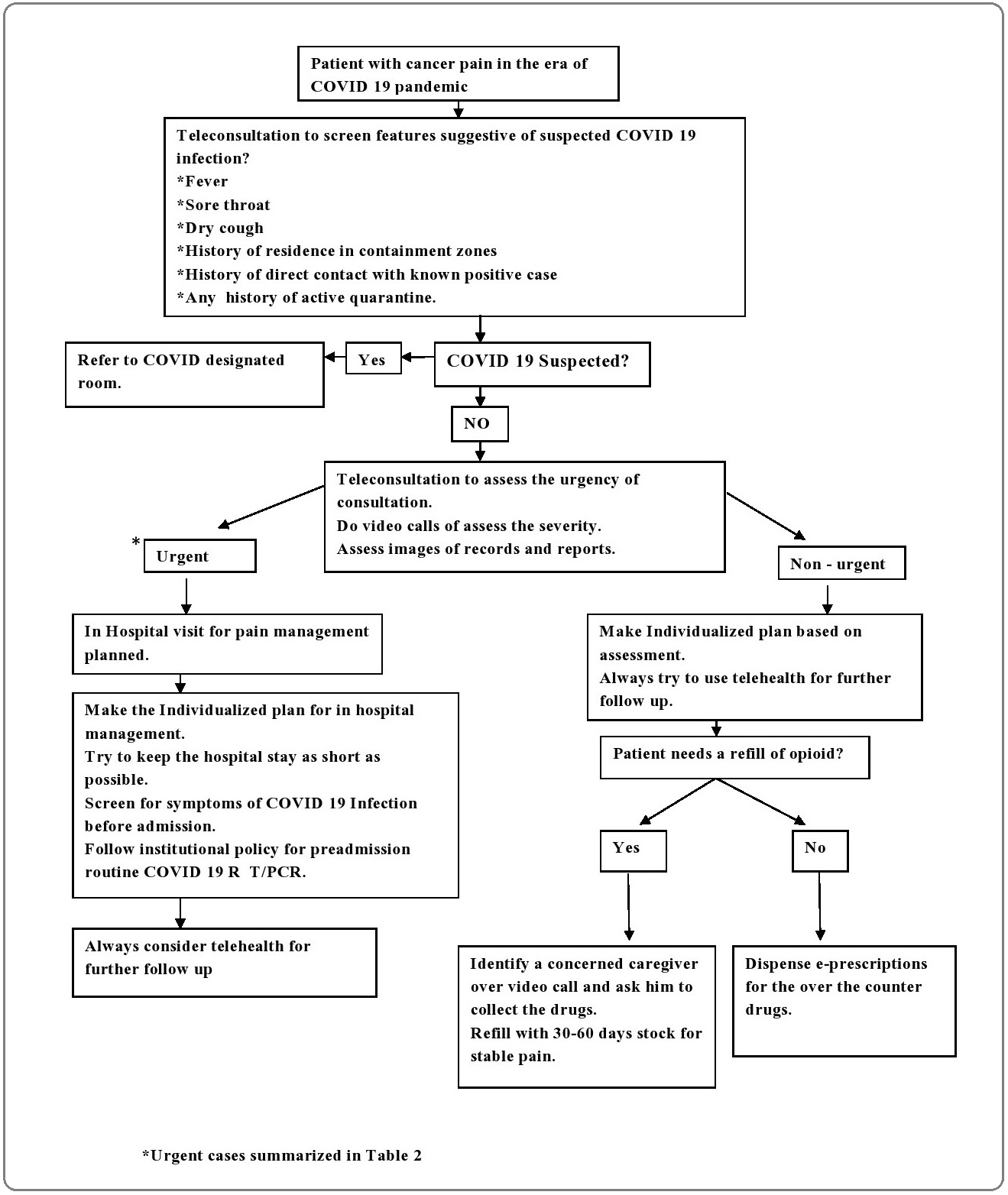
A screening method should be established for the patients before they visit the hospital for pain management. Telemedicine is a potential modality of screening patients with chronic pain for priority service. The telemedicine service has regained its popularity during pandemic as it does allow face to face interaction with patients over a video consultation with good patient acceptability [61].This can aid to physically examine the patients, checking the compliance by counting drug strips [62] identifying any reactions or side effects to the therapies and consulting with primary physicians [63] to take a shared decision. Many countries, e.g. Canada,UK, US has waived off the restrictions on previously imposed restrictions on use of telemedicine. Some of the countries, e.g. India [64] has allowed registered medical practitioners to use telemedicine mainly addressing the current pandemic situation and may be amended from time to time in future. Thus, the practitioners need to be updated about such regulations and license required for practicing pain management and prescribing drugs over telemedicine. Moreover individualized assessment for urgency and treatment plan should be made for each patient. Figure 3 describes an integrated strategy of implementing telemedicine service for prioritization of patients and prescribing medications.
Figure 3:Integrated Strategy of Prioritization Patients with Cancer Pain for in Hospital Visits During COVID-19 Pandemic.
2. Prescription strategies of analgesics
The analgesics prescription should be majorly based on conventional WHO pain ladder. Following drugs need careful consideration and some guiding principles for prescription:
A. Opioid Prescription strategies:
Opioids prescriptions need special consideration as opioids potentially supress the immune system [38]. Though there is still lack of good randomized clinical trials [65], many literature suggests that opioids cause an unfavourable modulation of immune system and increase severity of respiratory infection. Moreover, fever is one of the common symptoms in cancer patients. Fentanyl absorption from transdermal patch increases in such patients [66] precipitating the respiratory depression. Another major concern for prescribing opioids is legal barriers. In most of the countries prescriptions of opioids are regulated by strict laws with vigorous punishment. As for example, In India the prescription of opioids is regulated by the amendments of the Narcotic Drugs and Psychotropic Substances (NDPS) Act, 2014 [67]. The restrictions on e-prescriptions of opioids are still on, even after the recent amendment of the Indian Medical Council (Professional Conduct, Etiquette and Ethics) Regulation, 2002 by the Board of Governors (BoG) along with NITI Aayog on 25th March, 2020 [64]. A recent petition has been filed by the Indian academy of palliative care (IAPC) at the Board of Governors (BOG) of medical council of India (MCI). It seeks relaxation on refilling and changeover from one opioids to another over teleconsultation. But, the decision on this petition is still pending. Thus we recommend not providing e-prescriptions for opioids in India. But, telemedicine with real time video consultation should be used to maximum capacity to evaluate the pain, checking adherence to opioids therapy and monitoring side effects. Any initiation or changing one opioid to another needs an in-person visit. For prescription and dispensing of opioids, a responsible caregiver should be identified during teleconsultation and sent to hospital to collect it, if the patient cannot come to the clinic. As, opioids are key medications for managing moderate to severe cancer pain, it is important to balance the risk of infection and desired analgesics effect of opioids. Thus, we suggest the following principles to be followed during pandemic to prescribe opioids in cancer patients for pain management:
a. Don’t change the on-going opioid treatment regimen without any documented significant change in pain intensity or functional status.
b. Use real time visual modalities of telemedicine, whenever is feasible to assess the pain and document it in every follow up visits.
c. Use real time visual modalities of telemedicine, whenever feasible, to assess the compliance to opioids therapy by pill counts. Always cross check, document in the medical records.
d. Many countries do not allow e-prescriptions of opioids yet. Thus, providing prescriptions and dispensing of opioids should be only in person in such cases. Identify a key caregiver during teleconsultation over video calls and ask him to come to centre to collect the drugs. If the pain is stable, dispense at least drugs for 30 – 60 days to decrease the need of travel. Any initiation or changing one opioid to another needs an in-person visit.
e. Always identify a primary caregiver and educate them along with patient himself about potential side effects of opioids. Provide an emergency helpline number to assist and guide them in case of suspicion of opioid overdose.
f. Inform and educate patients and family members about the risk of infection in patients with opioid therapies, especially with high dose of long term opioid therapy. Educate them about infection control strategies, e.g. hand hygiene, coughing or sneezing hygiene, use of masks, restricted entry of visitors etc.
g. Be extra careful for patients with fentanyl patch. Patients should be educated about risk of overdose in case they have fever. If a patient develops fever, the patch should be removed. An emergency helpline number should be available with patient to help them in such situation. Such patients should be considered as a high priority patients for in hospital management with isolation facility.
B. Anti-inflammatory drugs prescription strategies:
There are some evidences, as already described earlier, that suggest that NSAIDS may aggravate the complications in a COVID-19 patient. But the evidence is not direct and concrete. Thus NSAIDS should be continued for a patient whenever needed. Although, educating patients about some warning signs of COVID-19 infection is important for them. Always provide with institutional emergency helpline number for such patients. The following major principles should be followed during the pandemic:
a. Continue the anti-inflammatory agents for all the patients who were previously on it.
b. Can start the drug in new patients if required for control of pain, especially patients with somatic or bony involvement.
c. Educate the patient to report immediately over emergency telephone helpline number if there is new onset fever or myalgia.
C. Steroids prescription strategies:
Steroids are considered as useful adjuvant in many cancer pain syndromes. But, there is risk and controversy regarding use of steroids in patients during in the pandemic, as it can lead to altered immune response [68]. Thus, following principles should be followed while using steroids for cancer pain management:
a. Continuing or starting new steroid therapy for pain management in cancer patient should be individualized strategy. The risk of infection and benefit in pain management should be weighed in case to case basis. If there is any doubt regarding this, one should take opinion from an infectious disease expert.
b. Whenever steroid needs to be used, use dexamethasone or betamethasone, as they cause short term immunosuppression as compared to methyl prednisolone [69].
c. Avoid use of steroids as adjuvants in neurolytic blocks and neuraxial administration, as evidence suggests them not to be safe [70].
3. Strategies for interventional procedures for cancer pain:
Interventional pain procedures are now an integral part of cancer pain management [71]. Different interventions, e.g. intrathecal pump placement with continuous neuraxial drug delivery, neuromodulation, neurolytic blocks etc have shown a better quality of life in terminal cancer patients. But, pain procedures are known to cause several complications, including serious life threatening infections [71-72]. Thus two main adaptation strategies should be adopted for pain intervention procedures in cancer patients during this pandemic:
a. Choose only “urgent” cases as eligible for interventional procedures.
b. Follow procedural considerations for strict infection control.
a. Choosing “urgent” cases for pain intervention:
Though modification of WHO ladder suggests an early integration of interventional procedures for cancer pain, the scientific evidences are limited and not robust. Thus an individualized approach should be considered for patients requiring interventional pain procedures. Only cases where benefits clearly outweigh the risks should be considered for eligibility. All new insertion of implants should be avoided. Pain interventions often need hospital admission for the patient and even administration of anaesthesia for it. During a pandemic, when decreasing footfalls of patients at hospital is a priority, we need to be very careful to choose only those patients who require pain interventions urgently. Examples of such “urgent” conditions may include, but not limited to the following: [73]
• Intrathecal pump (ITP) failure, displaced or disconnection causing inadequate delivery.
• ITP refill with medications and before expiry of battery life to prevent withdrawal symptoms
• Infection of the implants.
b. Procedural considerations and strategies [74].
Any intervention needs special precautions during a pandemic regarding infection control strategy. At our centre, All urgent cases of intervention undergo a screening for COVID -19 (RT-PCR) before the procedure, as per our institutional protocol. We suggest following local or institutional protocol regarding preprocedure testing. History taking and examination should take place over video consultation before calling every patient to the hospital. History taking should rule out features suggestive of a suspected case of COVID-19, e.g. fever, dry cough, history of residence in containment zones, history of direct contact with known positive case or any history of active quarantine. Usually the procedures are less aerosol generating, they are considered as low risk cases. But, the procedures, if needs an administration of anaesthesia, it should be considered as highly aerosol generating and high risk procedures [75-76]. The strategies are summarized in Table 3.
| COVID 19 negative and low risk cases | COVID 19 positive and high risk cases: |
| 1. Patient to be managed at a clean non covid area. | 1. All patients to be called at designated COVID areas. |
| 2. Patient should enter wearing a surgical mask. | 2. All staff should wear full personal protective equipment (PPE). |
| 3. Minimize the staff numbers in the room to minimum. 4. All staffs should wear impervious gown, well fitted N95 mask, head cap, shoe cover, face shield and sterile gloves. 5. Arrange all the drugs and equipment beforehand; bring them to the procedure room in a clean plastic bag. 6. Cover the ultrasound probe with plastics to avoid contamination. | 3. Airway management during anaesthesia should be done by most experienced person with rapid sequence intubation. Bag mask ventilation should be avoided. The intubation should be performed under a customized intubation box or plastic cover. Always use two viral filters, e.g. one at patient end and one at expiratory limb of ventilator [73-74] |
| 7. Doff and Perform hand hygiene properly at the end of procedure. | 4. Rest precautions are as same as for low risk cases. |
4. Considerations for palliative radiotherapy (RT):
Palliative radiotherapy is an useful adjuvant modality for managing resistant bony pain due to metastatic cancer. Providing radiotherapy needs in hospital visit by patients. Moreover acute side effects of palliative radiotherapy may be seen after radiotherapy up to 4-6 weeks [31]. Thus, it is the need of the hour to decrease the dose and duration of palliative radiotherapy. The European Study Group of Bone Metastases (GEMO) has already published their recommendations for palliative radiotherapy in painful bony metastasis [77]. The following principles should be followed in view of the current pandemic:
a. Palliative radiotherapy should be considered pain due to bony metastases which is not responsive to strong opioids, patients with acute intolerance to opioids, with impending spinal cord compression.
b. Use single fraction radiotherapy (8Gy/1#) instead of conventional fractionated treatment (20GY, 5#) [77].
c. If a repeat session is required, wait for at least 4 weeks [78]
d.In metastatic spinal cord compression, routine use of high dose steroids during radiotherapy is poorly supported by evidence in literatures. Thus we suggest using a short course of corticosteroids (Dexamethasone 16 mg daily) only if there is high chance of acute inflammatory oedema after radiotherapy [77]. A suspicion of COVID-19 infection needs to be ruled out in all such patients who will be considered for corticosteroids.
5. Providing holistic care for pain:
Cancer pain can be multifactorial and needs multimodal approach of management. Dame Cicely Saunders coined the term “total pain” for describing multidimensional domains of pain [79]. The same concept has been adopted for managing cancer pain time and again. et al. showed that managing psychological distress helps to manage cancer pain better and improves overall quality of life. Social distancing and quarantine in the era of pandemic has tremendous impact on psychological distress of the patients [80]. Social stigma and restrictions in mobility tends to cause barriers for the patients to access the social support groups and trained psychologists. Telemedicine can be an effective alternative to provide this psychological support to them. Feasibility and viability of an online system for managing chronic pain with multidisciplinary approach has been already established [81]. As compared to a face to face session, online individualized cognitive behavioural therapies for cancer patients can be really helpful and effective to deal with the psychological distress [82]. Different types of nonpharmacological interventions that can be provided through an online platform are providing mindfulness therapies, interactive peer support groups, expert counselling for grief and bereavement, physical rehabilitation training and cognitive therapies.
In conclusion, management of cancer pain is a priority service during pandemic for health care providers due to its physical and ethical considerations. The possible biophysiological considerations of different analgesics with COVID 19 infection should be kept in mind. The strategies adopted for safe and effective management of cancer pain includes prioritization of patients for in hospital visits and urgent interventions, special precautions for prescribing high dose of opioids, steroids and NSAIDS, modification in dose of palliative radiotherapy and using telehealth whenever feasible for screening, triaging, managing therapies and providing psycho-social support. Further high quality clinical trials and an international collaborative consensus guideline for managing cancer pain is the need of hour and highly recommended.
References
- World Health Organization 2018 [Available from: https:// www.who.int/news-room/fact-sheets/detail/cancer .
- Pain in cancer patients: pain assessment by patients and family caregivers and problems experienced by caregivers Ovayolu Özlem, Ovayolu Nimet, Aytaç Sema, Serçe Sibel, Sevinc Alper. Supportive Care in Cancer.2014;23(7). CrossRef
- Change in Cancer Pain Management in Korea Between 2001 and 2006: Results of Two Nationwide Surveys Hong Sook Hee, Roh Sang Young, Kim Si Young, Shin Sang Won, Kim Chul Soo, Choi Jin Hyuk, et al . Journal of Pain and Symptom Management.2011;41(1). CrossRef
- Impact of Epidural Analgesia on Quality of Life and Pain in Advanced Cancer Patients He Qun-Hui, Liu Qing-Ling, Li Zhen, Li Ke-Zhong, Xie Yong-Gang. Pain Management Nursing.2015;16(3). CrossRef
- High prevalence of pain in patients with cancer in a large population-based study in The Netherlands van den Beuken-van Everdingen Marieke H.J., de Rijke Janneke M., Kessels Alfons G., Schouten Harry C., van Kleef Maarten, Patijn Jacob. Pain.2007;132(3). CrossRef
- Cancer-related pain: a pan-European survey of prevalence, treatment, and patient attitudes Breivik H., Cherny N., Collett B., de Conno F., Filbet M., Foubert A.J., Cohen R., Dow L.. Annals of Oncology.2009;20(8). CrossRef
- Pain Syndromes in Patients with Cancer Foley Kathleen M.. Medical Clinics of North America.1987;71(2). CrossRef
- Pathophysiology of Pain in Cancer von Gunten Charles F.. Journal of Pediatric Hematology/Oncology.2011;33. CrossRef
- Prevalence of undertreatment in cancer pain. A review of published literature Deandrea S., Montanari M., Moja L., Apolone G.. Annals of Oncology.2008;19(12). CrossRef
- Impact of Undertreatment of Cancer Pain With Analgesic Drugs on Patient Outcomes: A Nationwide Survey of Outpatient Cancer Patient Care in Taiwan Shen Wen-Chi, Chen Jen-Shi, Shao Yu-Yun, Lee Kuan-Der, Chiou Tzeon-Jye, Sung Yung-Chuan, et al . Journal of Pain and Symptom Management.2017;54(1). CrossRef
- World Health Organization . WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020 2020 [Available from: Available from: https:// www.who.int/dg/speeches/detail/who-director-general-s- opening-remarks-at-the-media-briefing-on-covid-19---11- march-2020..
- The impact of the COVID-19 pandemic on cancer care Richards Mike, Anderson Michael, Carter Paul, Ebert Benjamin L., Mossialos Elias. Nature Cancer.2020;1(6). CrossRef
- COVID-19 and Cancer: a Comprehensive Review Gosain Rohit, Abdou Yara, Singh Abhay, Rana Navpreet, Puzanov Igor, Ernstoff Marc S.. Current Oncology Reports.2020;22(5). CrossRef
- WHO guidelines for the use of analgesics in cancer pain Ventafridda V, Saita L, Ripamonti C, De Conno F. Int J Tissue React.1985;7(1):96-96.
- World Health Organization .Cancer pain relief. Geneva. 1986 [Available from: https://apps.who.int/iris/bitstream/ handle/10665/43944/9241561009_eng.pdf..
- [Treatment of pain in the oncology patient] Araujo AM, Gómez M, Pascual J, Castañeda M, Pezonaga L, Borque JL. An Sist Sanit Navar.2004;27(Suppl 3):63-75.
- Is the WHO analgesic ladder still valid? Twenty-four years of experience Vargas-Schaffer G. Can Fam Physician. 2010;56(6):514-7.2010;56(6):514-517, e202-5.
- Neurolytic Sympathectomy in the Management of Cancer Pain—Time Effect: A Prospective, Randomized Multicenter Study Amr Yasser M., Makharita Mohamed Y.. Journal of Pain and Symptom Management.2014;48(5). CrossRef
- Individualized interventional pain management technique in early stage of cancer pain: A desirable protocol for improving quality of life Bhatnagar Sushma. Indian Journal of Palliative Care.2011;17(2). CrossRef
- The role of tramadol in cancer pain treatment—a review Leppert Wojciech, Łuczak Jacek. Supportive Care in Cancer.2004;13(1). CrossRef
- Codeine, alone and with paracetamol (acetaminophen), for cancer pain Straube Carmen, Derry Sheena, Jackson Kenneth C, Wiffen Philip J, Bell Rae Frances, Strassels Scott, Straube Sebastian. Cochrane Database of Systematic Reviews.2014. CrossRef
- Tapentadol for Cancer Pain Management: A Narrative Review Carmona-Bayonas Alberto, Jiménez Fonseca Paula, Virizuela Echaburu Juan. Pain Practice.2017;17(8). CrossRef
- Methadone for cancer pain Nicholson Alexander B, Watson Graeme R, Derry Sheena, Wiffen Philip J. Cochrane Database of Systematic Reviews.2017. CrossRef
- Transdermal fentanyl for cancer pain Hadley Gina, Derry Sheena, Moore R Andrew, Wiffen Philip J. Cochrane Database of Systematic Reviews.2013. CrossRef
- Buprenorphine for treating cancer pain Schmidt-Hansen Mia, Bromham Nathan, Taubert Mark, Arnold Stephanie, Hilgart Jennifer S. Cochrane Database of Systematic Reviews.2015. CrossRef
- Intermittent Subcutaneous Opioids for the Management of Cancer Pain Parsons Henrique A., Shukkoor Abdul, Quan Hue, Delgado-Guay Marvin O., Palmer J. Lynn, Fainsinger Robin, Bruera Eduardo. Journal of Palliative Medicine.2008;11(10). CrossRef
- Rational Use of Sublingual Opioids in Palliative Medicine Reisfield Gary M., Wilson George R.. Journal of Palliative Medicine.2007;10(2). CrossRef
- Transdermal opioids for cancer pain Skaer Tracy L. Health and Quality of Life Outcomes.2006;4(1). CrossRef
- The importance of non-opioid analgesics for cancer pain relief according to the guidelines of the World Health Organization Grond S, Zech D, Schug SA, Lynch J, Lehmann KA. Int J Clin Pharmacol Res.1991;11(6):253-260.
- Use of non-steroidal anti-inflammatory drugs in the treatment of pain in cancer. Ventafridda V, Fochi C, Conno D, Sganzerla E. British Journal of Clinical Pharmacology.1980;10(S2). CrossRef
- Palliative radiotherapy Spencer Katie, Parrish Rhona, Barton Rachael, Henry Ann. BMJ.2018. CrossRef
- Antidepressants in cancer pain Panerai AE, Bianchi M, Sacerdote P, Ripamonti C, Ventafridda V, De Conno F. J Palliat Care.1991;7(4):42-44.
- A critical appraisal of gabapentinoids for pain in cancer patients Jordan Roberta I., Mulvey Matthew R., Bennett Michael I.. Current Opinion in Supportive and Palliative Care.2018;12(2). CrossRef
- Intranasal Ketamine and Its Potential Role in Cancer-Related Pain Singh Vinita, Gillespie Theresa W., Harvey Robert Donald. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy.2018;38(3). CrossRef
- Cannabinoids for adult cancer-related pain: systematic review and meta-analysis Boland Elaine G, Bennett Michael I, Allgar Victoria, Boland Jason W. BMJ Supportive & Palliative Care.2020;10(1). CrossRef
- Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China Liang Wenhua, Guan Weijie, Chen Ruchong, Wang Wei, Li Jianfu, Xu Ke, et al . The Lancet Oncology.2020;21(3). CrossRef
- Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study Kuderer Nicole M, Choueiri Toni K, Shah Dimpy P, Shyr Yu, Rubinstein Samuel M, Rivera Donna R, et al . The Lancet.2020;395(10241). CrossRef
- The Effectiveness and Risks of Long-Term Opioid Therapy for Chronic Pain: A Systematic Review for a National Institutes of Health Pathways to Prevention Workshop Chou Roger, Turner Judith A., Devine Emily B., Hansen Ryan N., Sullivan Sean D., Blazina Ian, Dana Tracy, Bougatsos Christina, Deyo Richard A.. Annals of Internal Medicine.2015;162(4). CrossRef
- Opiate abuse, innate immunity, and bacterial infectious diseases Wang Jinghua, Barke Roderick A., Ma Jing, Charboneau Richard, Roy Sabita. Archivum Immunologiae et Therapiae Experimentalis.2008;56(5). CrossRef
- Role of the mu-opioid receptor in opioid modulation of immune function Ninković Jana, Roy Sabita. Amino Acids.2011;45(1). CrossRef
- Dysfunction of the Hypothalamic–Pituitary–Adrenal Axis in Opioid Dependent Subjects: Effects of Acute and Protracted Abstinence Zhang Guo-Fu, Ren Yan-Ping, Sheng Li-Xia, Chi Yong, Du Wan-Jun, Guo Song, et al . The American Journal of Drug and Alcohol Abuse.2008;34(6). CrossRef
- Opioids and Their Endocrine Effects: A Systematic Review and Meta-analysis de Vries Friso, Bruin Mees, Lobatto Daniel J, Dekkers Olaf M, Schoones Jan W, van Furth Wouter R, Pereira Alberto M, Karavitaki Niki, Biermasz Nienke R, Zamanipoor Najafabadi Amir H. The Journal of Clinical Endocrinology & Metabolism.2019;105(4). CrossRef
- Opioid endocrinopathy: A clinical problem in patients with cancer pain MERDIN ALPARSLAN, MERDIN FATMA AVCI, GÜNDÜZ ŞEYDA, BOZCUK HAKAN, COŞKUN HASAN ŞENOL. Experimental and Therapeutic Medicine.2016;11(5). CrossRef
- Evidence for central opioid receptors in the immunomodulatory effects of morphine: review of potential mechanism(s)of action Mellon R.Daniel, Bayer Barbara M. Journal of Neuroimmunology.1998;83(1-2). CrossRef
- Effects of Fentanyl on Natural Killer Cell Activity and on Resistance to Tumor Metastasis in Rats Shavit Yehuda, Ben-Eliyahu Shamgar, Zeidel Alexander, Beilin Benzion. Neuroimmunomodulation.2004;11(4). CrossRef
- Opioids and the Management of Chronic Severe Pain in the Elderly: Consensus Statement of an International Expert Panel with Focus on the Six Clinically Most Often Used World Health Organization step III Opioids (Buprenorphine, Fentanyl, Hydromorphone, Methadone, Morphine, Oxycodone) Pergolizzi Joseph, Böger Rainer H, Budd Keith, Dahan Albert, Erdine Serdar, Hans Guy, et al . Pain Practice.2008;8(4). CrossRef
- Risks Related to the Use of Non-Steroidal Anti-Inflammatory Drugs in Community-Acquired Pneumonia in Adult and Pediatric Patients Voiriot Guillaume, Philippot Quentin, Elabbadi Alexandre, Elbim Carole, Chalumeau Martin, Fartoukh Muriel. Journal of Clinical Medicine.2019;8(6). CrossRef
- Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Fang Lei, Karakiulakis George, Roth Michael. The Lancet Respiratory Medicine.2020;8(4). CrossRef
- Indomethacin has a potent antiviral activity against SARS coronavirus Amici C, Di Caro A, Ciucci A, Chiappa L, Castilletti C, Martella V, et al . Antivir Ther.2006;11(8):1021-1030.
- Acute kidney injury in patients hospitalized with COVID-19 Hirsch Jamie S., Ng Jia H., Ross Daniel W., Sharma Purva, Shah Hitesh H., Barnett Richard L., et al . Kidney International.2020;98(1). CrossRef
- Non-steroidal anti-inflammatory drug induced acute kidney injury in the community dwelling general population and people with chronic kidney disease: systematic review and meta-analysis Zhang Xinyu, Donnan Peter T, Bell Samira, Guthrie Bruce. BMC Nephrology.2017;18(1). CrossRef
- Non-steroidal anti-inflammatory drugs and covid-19 Little Paul. BMJ.2020. CrossRef
- The Role of Corticosteroids in the Treatment of Pain in Cancer Patients Leppert Wojciech, Buss Tomasz. Current Pain and Headache Reports.2012;16(4). CrossRef
- Dexamethasone in the prophylaxis of radiation-induced pain flare after palliative radiotherapy for bone metastases: a double-blind, randomised placebo-controlled, phase 3 trial Chow Edward, Meyer Ralph M, Ding Keyue, Nabid Abdenour, Chabot Pierre, Wong Philip, et al . The Lancet Oncology.2015;16(15). CrossRef
- Effects of methylprednisolone on peritumoral brain edema Yamada Kazuo, Ushio Yukitaka, Hayakawa Toru, Arita Norio, Yamada Noriko, Mogami Heitaro. Journal of Neurosurgery.1983;59(4). CrossRef
- ?Disappearing? spinal cord compression: Oncolytic effect of glucocorticoids (and other chemotherapeutic agents) on epidural metastases Posner Jerome B., Howieson John, Cvitkovic Esteban. Annals of Neurology.1977;2(5). CrossRef
- Description and clinical treatment of an early outbreak of severe acute respiratory syndrome (SARS) in Guangzhou, PR China Zhao Z.. Journal of Medical Microbiology.2003;52(8). CrossRef
- Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome WONG C. K., LAM C. W. K., WU A. K. L., IP W. K., LEE N. L. S., CHAN I. H. S., et al . Clinical & Experimental Immunology.2004;136(1). CrossRef
- The management of coronavirus infections with particular reference to SARS Wong S. S. Y., Yuen K.-Y.. Journal of Antimicrobial Chemotherapy.2008;62(3). CrossRef
- Cytokine Responses in Porcine Respiratory Coronavirus-Infected Pigs Treated with Corticosteroids as a Model for Severe Acute Respiratory Syndrome Zhang Xinsheng, Alekseev Konstantin, Jung Kwonil, Vlasova Anastasia, Hadya Nagesh, Saif Linda J.. Journal of Virology.2008;82(9). CrossRef
- What is the patient acceptability of real time 1:1 videoconferencing in an orthopaedics setting? A systematic review Gilbert Anthony W., Jaggi Anju, May Carl R.. Physiotherapy.2018;104(2). CrossRef
- Unannounced Telephone-Based Pill Counts: A Valid and Feasible Method for Monitoring Adherence Fredericksen R., Feldman B. J., Brown T., Schmidt S., Crane P. K., Harrington R. D., Dhanireddy S., McReynolds J., Lober W. B., Bangsberg D. R., Kitahata M. M., Crane Heidi M.. AIDS and Behavior.2014;18(12). CrossRef
- Physician-to-Physician Telephone Consultations for Chronic Pain Patients: A Pragmatic Randomized Trial Clark Alexander J, Taenzer Paul, Drummond Neil, Spanswick Christopher C, Montgomery Lori S, Findlay Ted, Pereira John X, Williamson Tyler, Palacios-Derflingher Luz, Braun Ted. Pain Research and Management.2015;20(6). CrossRef
- Telemedicine Practice Guidelines 2020 [Available from: Available from: https://www.mohfw.gov.in/pdf/ Telemedicine.pdf..
- Opioids and the immune system – friend or foe Plein Lisanne Mirja, Rittner Heike L. British Journal of Pharmacology.2017;175(14). CrossRef
- Important Health Advisory: Safety WARNINGS Regarding Use of Fentanyl Transdermal Patch 2008 [updated Last accessed on 13/06/2020 Available from: https://www.health. ny.gov/diseases/aids/providers/prevention/harm_reduction/ opioidprevention/docs/fentanyl_alert.pdf..
- The NDPS Act 1985, was amended in 2014 [updated [Last accessed on 2018 Sep 18] Available from: Available from: http://www.mpsja.mphc.gov.in/Joti/pdf/LU/NDPS%20 SINGH%20SIRdocx%20corrected.pdf..
- Perioperative Steroid Management Liu Melanie M., Reidy Andrea B., Saatee Siavosh, Collard Charles D.. Anesthesiology.2017;127(1). CrossRef
- Systemic effects of epidural steroid injections for spinal stenosis Friedly Janna L., Comstock Bryan A., Heagerty Patrick J., Bauer Zoya, Rothman Micol S., Suri Pradeep, Hansen Ryan, Avins Andrew L., Nedeljkovic Srdjan S., Nerenz David R., Akuthota Venu, Jarvik Jeffrey G.. PAIN.2018;159(5). CrossRef
- Safe Use of Epidural Corticosteroid Injections: Recommendations of the WIP Benelux Work Group Van Boxem Koen, Rijsdijk Mienke, Hans Guy, de Jong Jasper, Kallewaard Jan Willem, Vissers Kris, van Kleef Maarten, Rathmell James P., Van Zundert Jan. Pain Practice.2018;19(1). CrossRef
- Interventional Techniques for the Management of Cancer-Related Pain: Clinical and Critical Aspects Kurita Geana, Sjøgren Per, Klepstad Pål, Mercadante Sebastiano. Cancers.2019;11(4). CrossRef
- Interventional Pain Procedures and the Risk of Infection Provenzano D. A, Hanes M. C, Deer T. R. Essentials of Pain Medicine.2018.
- Caring for patients with pain during the COVID ‐19 pandemic: consensus recommendations from an international expert panel Shanthanna H., Strand N. H., Provenzano D. A., Lobo C. A., Eldabe S., Bhatia A., Wegener J., Curtis K., Cohen S. P., Narouze S.. Anaesthesia.2020;75(7). CrossRef
- Acute Intrathecal Baclofen Withdrawal: A Brief Review of Treatment Options Ross James C., Cook Aaron M., Stewart Gary L., Fahy Brenda G.. Neurocritical Care.2010;14(1). CrossRef
- All India difficult airway association (AIDAA) consensus guidelines for airway management in the operating room during the COVID-19 pandemic Garg Rakesh, Patwa Apeksh, Shah Amit, Divatia JigeeshuVasishtha, Kundra Pankaj, Doctor JesonRajan, Shetty SumalathaRadhakrishna, Ahmed SyedMoied, Das Sabyasachi, Myatra SheilaNainan. Indian Journal of Anaesthesia.2020;64(14). CrossRef
- Consensus guidelines for managing the airway in patients with COVID ‐19 Cook T. M., El‐Boghdadly K., McGuire B., McNarry A. F., Patel A., Higgs A.. Anaesthesia.2020;75(6). CrossRef
- Adapting palliative radiation therapy for bone metastases during the Covid-19 pandemic: GEMO position paper Thureau Sébastien, Faivre Jean Christophe, Assaker Richard, Biver Emmanuel, Confavreux Cyrille B., Debiais Françoise, et al . Journal of Bone Oncology.2020;22. CrossRef
- Single versus multiple fractions of repeat radiation for painful bone metastases: a randomised, controlled, non-inferiority trial Chow Edward, van der Linden Yvette M, Roos Daniel, Hartsell William F, Hoskin Peter, Wu Jackson S Y, et al . The Lancet Oncology.2014;15(2). CrossRef
- Dame Cicely Saunders C R . BMJ.2005;331(7510):238.80.
- The psychological impact of quarantine and how to reduce it: rapid review of the evidence Brooks Samantha K, Webster Rebecca K, Smith Louise E, Woodland Lisa, Wessely Simon, Greenberg Neil, Rubin Gideon James. The Lancet.2020;395(10227). CrossRef
- Reboot Online: A Randomized Controlled Trial Comparing an Online Multidisciplinary Pain Management Program with Usual Care for Chronic Pain Smith Jessica, Faux Steven G, Gardner Tania, Hobbs Megan J, James Mathew A, Joubert Amy E, et al . Pain Medicine.2019;20(12). CrossRef
- Consolidation and prediction of long-term treatment effect of group and online mindfulness-based cognitive therapy for distressed cancer patients Cillessen L., Schellekens M. P. J., Van de Ven M. O. M., Donders A. R. T., Compen F. R., Bisseling E. M., Van der Lee M. L., Speckens A. E. M.. Acta Oncologica.2018;57(10). CrossRef
- Radiation-Induced Oral Mucositis Maria Osama Muhammad, Eliopoulos Nicoletta, Muanza Thierry. Frontiers in Oncology.2017;7. CrossRef
- WHO toxicity scale. 2009 Oncoprof . Avilable at www. oncoprof.net/Generale2000/g09_Chimiotherapie/ Complements/g09-gb_comp01.htm. Last accesed on 11.08.2020..
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times