The Effect of Protocol- based Education on Number of Errors in Radiotherapy
Download
Abstract
Introduction: Education is important and plays a vital role in all fields of science. During radiotherapy, some errors may happen that can have detrimental effects on treatment outcomes. We designed this study to investigate the effect of using a protocol on the range of errors.
Materials and Methods: A checklist, including 5 sets of errors was designed to investigate whether having a certain protocol has any effect on workflow. To reach that, 106 patient profiles compiled randomly to ascertain those five factors in two radiotherapy and oncology centers.
Results: Based on the concluded data from statistical analyze, all 5 factors, including the monitor unit, shield, coach rotation, field size, and second phase had a significant change in terms of statistic (p<0.05).
Conclusion: Education has utmost importance in any type of skill, especially when it comes to patients' affairs. Radiotherapy; however, has its errors sets in which the rate of human uncertainty must be reduced. Furthermore, having certain rules to determine every one’s responsibility seems to be essential.
Introduction
Radiotherapy has been considered as one of the principal modalities in cancer treatment [1]. To begin treatment procedure, several steps should be taken, such as taking a history of patient, considering different modalities to treat, prescription of treatment dose, imaging and target volume definition, treatment planning, quality assurance (QA) and verification of the plan, patient set up, treatment delivery, and verification of its precision. Moreover, to establish more accuracy of each step, periodic QA is needed [2, 3]. There is a group of staff, including radiotherapists, radiotherapy technicians , medical physicists, and radiation safety officer [4]. There are so many difficulties in which each electronic-portal image- device step could turn into error prone opportunity [5]. The main two subdivisions of errors are systemic and operator. For instance, using a linear accelerator equipped with the multileaf collimator in which some of the leaves do not move correctly is systemic error, while the wrong patient's set up is operator error [6]. Since 1995, some standards have been suggested to reduce the occurrence of errors in radiotherapy from different organizations such as the World Health Organization (WHO), American Association of Physicists in Medicine (AAPM), European Society for Therapeutic Radiation Oncology (ESTRO) and Clinical Oncology Information Network (COIN) [4,7]. Thorough these years, some new cutting edge facilities such as record and verification (R and V) system and electronic portal image device (EPID) have been produced to reduce some of these errors in data transfer and management of treatment procedure [7]. Every center around the globe, reports their probable errors and their reasons either to improve the knowledge or share the experiences [8]. Ishikura from the National Cancer Center in Japan, based on a review, made a QA improvement article, focusing on the advanced program for patient safety [11]. Gerard et al. from France established IMRT quality assurance methods to reduce the statistical problems with statistical process control tools [12]. Gluhchev in 2002 evaluated radiotherapy procedure according to the random and systematic errors. His assay led to suggestion of an optimal value for the systematic errors to make a smaller deviation after correction [11].
This article tried to either emphasize the necessity of exploring reasons of errors or reducing their rates by means of enforcing some internal rules in every therapeutic center.
Materials and Methods
According to the effect size of 0.5, the power of 0.95 and probability level of 0.05, the sample size of each group was determined to be 106 cases. Based on the possible errors in any radiotherapy ward, 5 factors from 2 centers were chosen to be assessed, namely the monitor unit (MU), custom block arrangement (shield), coach rotation (coach), field size, and calculations related to the second phase of treatment (second phase). To assess the impact of education, some formal rules in terms of having work log, arranging excel file, and weekly review of events to come were set up. In a 6-month period, 106 profiles were investigated randomly and the effect of rules was checked in the second half of the year.
Statistical Analysis
To analyze the obtained data, which was normal and categorical, SPSS (version 23) was used and chi-Square test with confidence level of 95% was run.
Results
As statistical analyze showed, all factors except the field size had significant changes (p<0.05) that would be elaborated in following. In center 1, the percentage of the MU went down from 19 cases to 4 cases, the percentage for shield dived down from 15 cases to 4, coach errors, which was 11 cases reached just 3 ones, field size had 10 errors in the first half of year, which went through a rapid reduction to see 5 cases; the figures for the second phase registered a dramatic drop, which had 13 documented errors to reach merely 2 cases (p= 0.001, 0.007, 0.025, 0.142 and 0.003, respectively) errors (Fig. 3).
Figure 1: Time-Incidence of Errors Separated by the Type of Cancer in First Center.
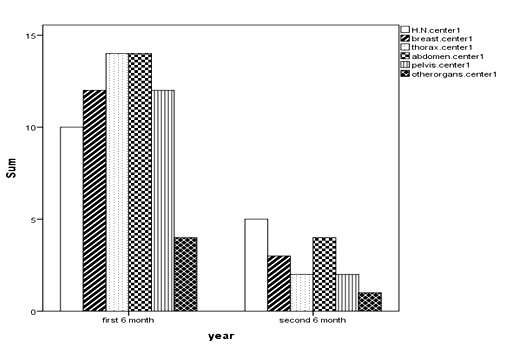
Figure 2: Time-Incidence of Errors Separated by the Type of Cancer in Second Center.
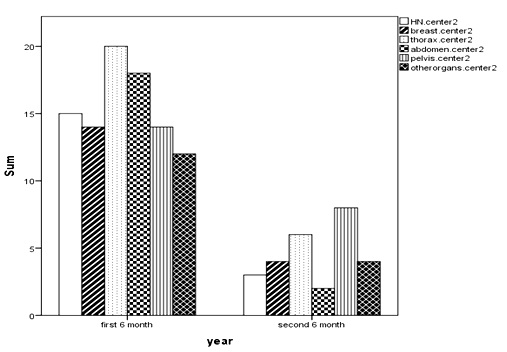
Figure 3: Time- Incidence of Investigating Factors in Center.
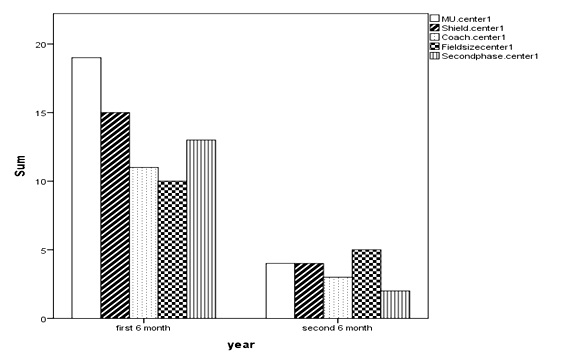
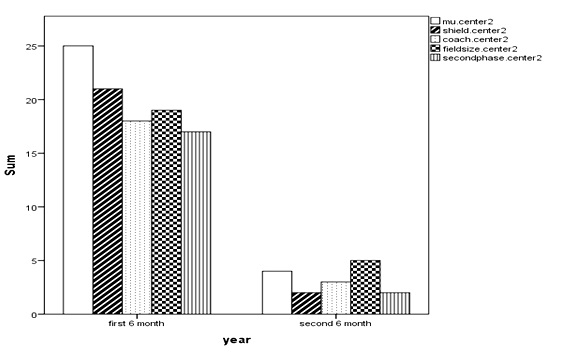
Figure 4: Time- Incidence of Investigating Factors in Center.
2
| Location of error | Head and Neck | Breast | Thorax | Abdomen | Pelvis | Other organs | Total |
| Grouping | |||||||
| Center 1 | 15 | 15 | 16 | 18 | 16 | 6 | 86 |
| Center 2 | 18 | 18 | 26 | 20 | 22 | 16 | 116 |
These data in the second center were as follows: MU errors saw a half decline from 25 to 4 errors, the shield factor decreased from 21 to 2 events, coach incidences were 18 then they dived to 3; at first the number of field size errors were 19 , but in the second half of year reached to 5 cases. The 17 events related to the second phase calculation met 2 incidences in the second half of year (p= 0.000, 0.000, 0.000, 0.002 and 0.000, respectively).
Discussion
Errors in radiotherapy as a therapeutic procedure, which deals with human life, have to be considered as an important issue, so it should be reduced as much as possible. Having protocol could decrease some of vivid error-prone procedures to meet the lesser incidence. During this study, the role and effect of having consensus criteria were assessed. The main goal of this study was the reduction of all predefined factors to reach a 'safe beach' where at least some probable and incipient events were cleared and prohibited.
During this study, before setting up a protocol, 25% of incidents were notified before the happening, 58% during the treatment course, and 17% were found during regular visits, which were done after completion of treatment. After enforcing criteria, those entire rate which mentioned above decreased, especially those which were in the middle of treatment (p=0.000).
In 2009, Baiotto et al declared that a verification, which could be manually, was an impressive opportunity to notify the treatment situation [13]. These data support our reduced rate of occurrence, which resulted from our manually provided criteria. The accidental events could be managed if some instruments and periodic surveys accomplish, as a vivid example having record and verification system and EPID or setting up report files related to errors [14]. Because there have not been such facilities in our two centers, only human related systemic errors were assessed. International atomic energy agency proposed a several - step prevention policy toward lesser accidental events in which for MU, firstly the output of linear accelerator and then a comparison of achieved data with a calibrated source should be defined [15,16].
Further investigation in this field especially to compare the application based on human interventional criteria in terms of outcome would be mandatory.
In conclusion, identification of errors is one of utmost important factors through which both quality and clinical outcomes of treatment would improve. This study promulgated the positive effects of having event restricting criteria emphasizing human related errors.
Funding
This work was supported by Shahid Beheshti University of Medical Sciences.
Acknowledgments
The authors are grateful to radiotherapy staff of Emam Hossein and Bo Ali Hospitals for accompanying us in this study.
Conflicts of interest :The authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest ( such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
References
[1]. Delaney G, Jacob S, Featherstone C, Barton M. The role of radiotherapy in cancer treatment: estimating optimal utilization from a review of evidence-based clinical guidelines. Cancer. 2005;104(6):1129-37.
[2]. World Health Organization (2008). Radiotherapy Risk Profile Technical Manual.
[3]. Moller TR, Ceberg J, Einhorn N, Lindholm C, Nyhle:n U, Svensson S, for the SBU Survey Group. Radiotherapy techniques in current use in Sweden. Acta Oncol.2003; 42: 376- 86.
[4]. Moller TR, Ceberg J, Einhorn N, Lindholm C, Nylen U, Svensson H. Radiotherapy techniques in current use in Sweden. Acta Oncologica. 2003 Jan 1;42(5-6):376-86.
[5]. Thwaites D, Scalliet P, Leer JW, Overgaard J. Quality assurance in radiotherapy. European Society for Therapeutic Radiology and Oncology Advisory Report to the Commission of the European Union for the 'Europe against Cancer Program. Radiother Oncol. 1995; 35(1):61-73.
[6]. Fuangrod T, Greer PB, Woodruff HC, Simpson J, Bhatia S, Zwan B, Timothy A, McCurdy BM, Middleton RH. Investigation of a real-time EPID-based patient dose monitoring safety system using site-specific control limits. Radiation Oncology. 2016 Aug 12;11(1): 106.
[7]. Fraass B, Doppke K, Hunt M, Kutcher G, Starkschall G, Stern R, Van Dyke J. American Association of Physicists in Medicine Radia-on Therapy Committee Task Group 53: Quality assurance for clinical radiotherapy treatment planning. Med Phys. 1998;25(10): 1773-1829.
[8]. Karp SJ. The Clinical Oncology Information Network (COIN) Project: background, purpose and products. J Eval Clin Pract. 1999;5(2):179-87.
[9]. Ortiz Lopez P, Cosset JM, Dunscombe P, Holmberg O, Rosenwald JC, Pinillos Ashton L, et al. ICRP publication 112. A report of preventing accidental exposures from new external beam radiation therapy technologies. Ann ICRP. 2009;39(4):1-86.
[10]. Pennsylvania Patient Safety Advisory. Errors in Radiation Therapy. 2009;6(3):87-92.
[11]. Ishikura S. Quality assurance of radiotherapy in cancer treatment: toward improvement of patient safety and quality of care. Jpn J Clin Oncol. 2008;38(11):723-9.
[12]. Gerard K, Grandhaye J, Marchesi V, Aletti P, Husson F, Noel A, Kafrouni H. Feasibility study of using statistical process control to optimize quality assurance in radiotherapy quality assurance in radiotherapy. J Qual Maint Eng. 2009;15: 331-43.
[13]. Baiotto B, Bracco C, Bresciani S, Mastantuoni A, Gabriele P, Stasi M. Quality assurance of a record-and-verify system. Tumori. 2009 Jul 1;95(4):467-72.
[14]. Asnaashari K, Gholami SO, Khosravi HR. Lessons learnt from errors in radiotherapy centers. Int. J. Radiat. Res. 2014 Oct 1;12(4):361-7.
[15]. Shafiq J, Barton M, Noble D, Lemer C, Donaldson LJ. An international review of patient safety measures in radiotherapy practice. Radiotherapy and Oncology. 2009 Jul 31;92(1):15-21.
[16].Holmberg O. Accident prevention in radiotherapy. Biomed Imaging Interv J. 2007;3(2):e27.
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times