Comparison of Treatment Outcomes between Right- and Left-sided Colorectal Adenocarcinoma after Adjuvant Chemotherapy
Download
Abstract
Objective: The survival outcomes of patients with metastatic colorectal adenocarcinoma based on tumor laterality has already been established based on large-scale retrospective studies. As for the non-metastatic disease, the data is much more conflicting. Local data in this population is also scarce. In this study, we determined the difference in survival of right-sided versus left-sided colorectal cancer patients after surgery and adjuvant chemotherapy.
Patients and Methods: This retrospective study analyzed a total of 124 patients who were diagnosed with early to locally advanced (stage I to IVA) colorectal adenocarcinoma and underwent definitive surgery and adjuvant systemic treatment per physician’s preference. The patients were stratified according to the primary tumor laterality: Right-Sided Colon cancer (RCC) and Left-sided Colon cancer (LCC). The primary outcome being investigated is the disease-free survival (DFS) at 3 years and 5 years. Secondary outcomes are overall survival (OS) at 3 years and 5 years, and site of disease recurrence across laterality.
Results: The findings did not show a significant difference in the 3-year and 5-year DFS between RCC and LCC after surgery and adjuvant chemotherapy (3-year DFS: 50.0% in the RCC group and 54.3% in the LCC group; P=.671; 5-year DFS: 36.7% in the RCC group and 36.2% in the LCC group, P=.474). The OS difference was also not significant at 3 years and 5 years (3-year OS: 68.8% in the RCC group and 73.9% in the LCC group, P=.572; 5-year OS: 31.3% in the RCC group and 26.1% in the LCC group, P=.474). The overall recurrence rate was not significantly different in both groups (65.6% in the RCC group and 66.3% in the LCC group; P=.944). Majority of the recurrences were at a distant site in both groups (61.1% in the RCC group and 69.6% in the LCC group; P=.501) and the most common were in the lungs, and liver.
Conclusion: The survival outcome of non-metastatic colorectal adenocarcinoma was not significantly different between RCC and LCC after surgery and adjuvant chemotherapy. The outcome was also similar after stratification of the population into early and locally advanced disease. More diverse clinical characteristics other than tumor location may be prognostic of disease-free and survival outcomes in the non-metastatic setting of colorectal cancer. Further studies with a larger sample size are needed to validate the correlation of survival to the specific stage and anatomic location.
Introduction
Colorectal cancer (CRC) is one of the most common malignancies in the Philippines. The local data from the Global Cancer Observatory 2020 showed that it ranks 3rd amongst all the leading new cancer cases for both sexes, with an annual incidence rate of 11.3% of total malignancies in the country. It also ranks 4th in overall cancer-specific mortality (CSM) [1, 2].
In a risk analysis study using the SEER-Medicare database in 2017, the researchers identified the difference in the cancer-specific mortality (CSM) of right-sided (involving the cecum, ascending, hepatic flexure, and proximal transverse colon) versus left-sided (involving the splenic flexure, descending, sigmoid, and rectosigmoid colon) CRC. The results showed that RCC demonstrated significant increased CSM at the metastatic stage (AHR, 1.175; P < .001) [3].
In the setting of non-metastatic CRC, Weiss et al. demonstrated no difference between the 5-year OS for patients with RCC and LCC after adjusting for multiple variables; instead, they found that the mortality in patients with stage II RCC was lower than it was in those with LCC (hazard ratio [HR], 0.92; 95% confidence interval [CI], 0.87–0.97; P = .001). On the other hand, the mortality was higher in patients with stage III RCC (HR, 1.12; 95% CI, 1.06–1.18; P < 0.001) [4]. These findings were echoed in the Korean study by Lim, et. al. wherein the researchers also determined the 5-year disease-free survival (DFS) advantage of the RCC group at stage III of the disease (61.1% vs 81.9%; P<.05). Furthermore, the findings of the latter showed that patients with RCC had a more advanced nodal stage, larger tumor size, and more frequently with lymphovascular invasion, and poorly differentiated histology [5]. Results in the earlier stage however were not uniformly consistent as multiple retrospective studies done in Asia did not show a significant difference in 5-year survival in stage I to II CRC [6].
Several studies have attempted to elucidate whether the phenotypic and genetic differences between RCC and LCC correlate into a significant difference in mortality risk. These studies mostly used large population-based databases, and conflicting results have been reported [3].
Materials and Methods
Patient population
Between January 2009 and June 2015, 204 patients were identified in the medical record database of St. Luke’s Medical Center, Philippines. All clinical, radiologic, and histopathologic data were reviewed retrospectively. Patients included were >18 years of age, diagnosed with non-metastatic colorectal adenocarcinoma (with surgical histopathologic and radiologic confirmation) and underwent adjuvant systemic chemotherapy per physician’s preference. Patients with distant metastasis (histopathologic or radiologic) at the outset that were not amenable for local treatment (unresectable oligometastasis/stage IVA and stage IVB) were excluded from the study. RCC was defined as the tumor location including the cecum, ascending colon, hepatic flexure, and the proximal two-thirds of the transverse colon. LCC was defined as the tumor location including the distal third of the transverse colon, splenic flexure, descending colon, sigmoid colon, and middle to high rectum (if the management approach was colon-specific). All patients that were included underwent staging scans to rule out distant metastasis (contrast-enhanced CT or PET/CT scan), underwent definitive surgery for colorectal cancer, and received adjuvant chemotherapy. Chemotherapy regimen given were oxaliplatin-based combination (FOLFOX4, and Capecitabine-Oxaliplatin) for 6 months. Only 1 patient was given capecitabine monotherapy based on the stage. The basis for giving adjuvant treatment in stage I-IIC patients was the presence of adverse features such as poorly differentiated histology, presence of lymphovascular invasion (LVI) and/or perineural invasion (PNI), intestinal obstruction, perforation, less than 12 lymph nodes harvested during surgery, and close/ indeterminate/positive surgical margins.
The primary objective of this study was to compare the survival outcomes between RCC and LCC after surgery and adjuvant treatment. The 3-year and 5-year DFS were used to measure the outcomes. Disease-Free survival was defined as the time from study entry (date of surgical histopathologic report) to the date of documented progression (radiologic and/or histopathologic) or death from any cause. The two groups were also compared according to age, gender, stage at diagnosis, and presence of adverse clinical and pathologic features.
Statistical analysis
The demographic data of the study population was stratified primarily into two groups: RCC and LCC. The patients were further dichotomized into early stage and locally advanced stage based on the presence of nodal metastasis in the post-surgical histopathology report. Categorical variables were expressed in numbers and percentages. The differences found were analyzed in a two-dimensional cross-comparison table and tested statistically by Chi-square test. The reported P values were two-sided and P values <0.05 were considered statistically significant. The time duration of years and months were calculated using an online day calculator application (https://www.timeanddate.com/date/duration.html).
Results
Patient characteristics
The patients’ baseline characteristics were listed in Table 1.
| RCC | LCC | P value | ||||
| n | % | n | % | |||
| Total | 32 | 25.8 | 92 | 74.2 | ||
| Age (years) | 0.061 | |||||
| <40 | 2 | 6.3 | 6 | 6.5 | ||
| 40-49 | 4 | 12.5 | 13 | 14.1 | ||
| 50-59 | 2 | 6.3 | 27 | 29.3 | ||
| 60-69 | 12 | 37.5 | 28 | 30.4 | ||
| ≥70 | 12 | 37.5 | 18 | 19.6 | ||
| Gender | 0.76 | |||||
| Male | 15 | 46.9 | 46 | 50 | ||
| Female | 17 | 53.1 | 46 | 50 | ||
| Adjuvant Chemotherapy | ||||||
| FOLFOX | 20 | 62.5 | 71 | 77.2 | ||
| Capecitabine, Oxaliplatin | 11 | 34.4 | 21 | 22.8 | ||
| Capecitabine | 1 | 3.1 | 0 | 0 | ||
| Stage | 0.22 | |||||
| Early stage (no nodal metastasis) | I | 1 | 3.1 | 0 | 0 | |
| IIA | 7 | 21.9 | 14 | 15.2 | ||
| IIB | 4 | 12.5 | 9 | 9.8 | ||
| IIC | 0 | 0 | 1 | 1.1 | ||
| Locally advanced (with nodal metastasis) | IIIA | 10 | 31.3 | 18 | 19.6 | |
| IIIB | 3 | 9.4 | 29 | 31.5 | ||
| IIIC | 7 | 21.9 | 16 | 17.4 | ||
| IVA | 0 | 0 | 5 | 5.4 | ||
| pT stage | ||||||
| Tx, T0, Tis, T1 | 0 | 0 | 0 | 0 | ||
| T2 | 10 | 31.3 | 21 | 22.9 | ||
| T3 | 11 | 34.4 | 47 | 51.1 | ||
| T4a | 10 | 31.3 | 21 | 22.9 | ||
| T4b | 1 | 3.1 | 3 | 3.3 | ||
| pN | ||||||
| NX | 0 | 0 | 0 | 0 | ||
| N0 | 12 | 37.5 | 24 | 26.1 | ||
| N1a | 0 | 0 | 16 | 17.4 | ||
| N1b | 2 | 6.3 | 7 | 7.6 | ||
| N1c | 9 | 28.1 | 17 | 18.5 | ||
| N2a | 3 | 9.4 | 19 | 20.7 | ||
| N2b | 6 | 18.8 | 9 | 9.8 | ||
| M1a | 0 | 0 | 5 | 100 | ||
| Adverse Features | ||||||
| Poorly differentiated | 22 | 68.8 | 12 | 13 | <.001 | |
| Perineural / Lymphovascular invasion (PNI/LVI) | 22 | 68.8 | 58 | 63 | 0.561 | |
| Obstruction | 2 | 6.3 | 26 | 28.3 | 0.01 | |
| Perforation | 0 | 0 | 0 | 0 | - | |
| <12 lymph nodes harvested | 3 | 9.4 | 7 | 7.6 | 0.751 | |
| Close/ Indeterminate/ Positive margins | 1 | 3.1 | 5 | 5.4 | 0.599 |
The total population included in the final analysis was 124 and was composed of 32 patients (25.8%) in the RCC group and 92 patients (74.2%) in the LCC group. Majority of the patients belonged in the age group of 50 years and above (75.0% in the RCC group and 79.4% in the LCC group), and there is no significant difference in the gender distribution (P=.760). Most of the patients received oxaliplatin-based adjuvant chemotherapy in both groups. Majority of the patients had locally advanced disease in both groups (62.6% in the RCC and 73.9% in the LCC group). The RCC group more frequently presented with poorly differentiated adenocarcinoma compared to the LCC group (68.8% vs 13.0%; P<.001). Acute intestinal obstruction was more commonly observed in the LCC than the RCC group (6.3% vs 23.3%; P=.010). There was no other significant difference in other poor risk features such as perineural and lymphovascular invasion, number of lymph nodes harvested, perforation, and close/ positive margins.
Survival outcomes
The results did not show a statistically significant difference in the 3-year and 5-year disease-free survival rate between RCC and LCC after surgery and adjuvant chemotherapy (50.0% in the RCC group and 54.3% in the LCC group did not have recurrence at 3 years; P=.671; 36.7% in the RCC group and 36.2% in the LCC group did not have recurrence at 5 years; P=.854, see Table 2).
| 3-year DFS | Right | Left | Total | P value | ||
| n | % | n | % | 0.671 | ||
| No recurrence | 16 | 50 | 50 | 54.3 | 69 | |
| With recurrence | 16 | 50 | 42 | 45.7 | 58 | |
| Total | 32 | 92 | 124 | |||
| 5-year DFS | Right | Left | Total | 0.854 | ||
| No recurrence | 11 | 34.4 | 30 | 32.6 | 41 | |
| With recurrence | 21 | 65.6 | 62 | 67.4 | 83 | |
| Total | 32 | 92 | 124 |
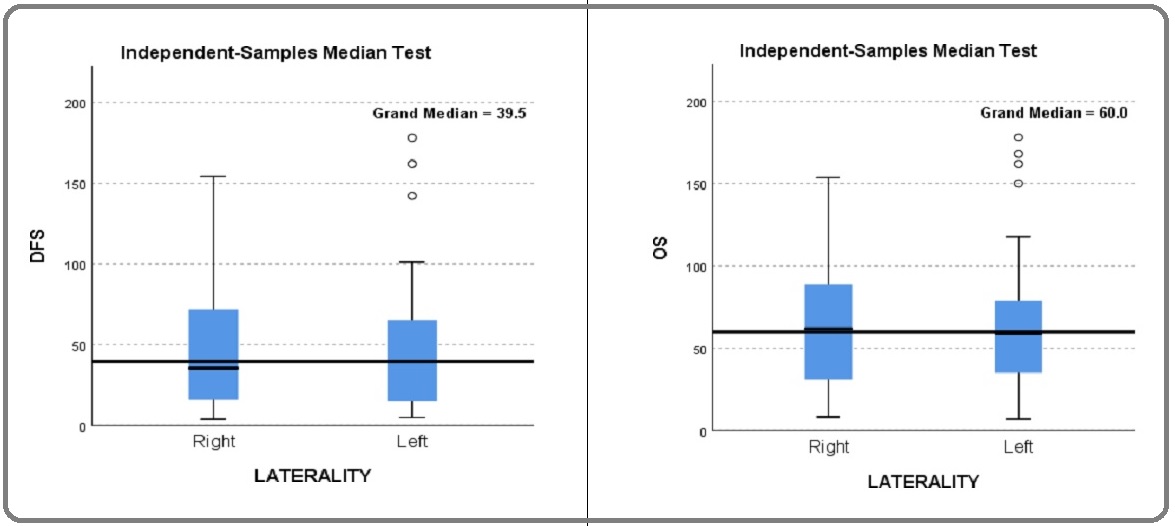
The 3-year and 5-year overall survival rate comparison also showed analogous findings (68.8% of patients in the RCC group and 73.9% in the LCC group were alive at 3 years; P=.572; 31.3% of patients in the RCC group and 26.1% in the LCC group were alive at 5 years; P=.474; see Table 3 and Figure 1a-1b).
| 3-year OS | Right | Left | Total | P value | ||
| n | % | n | % | 0.572 | ||
| Alive at 3 years | 22 | 68.8 | 68 | 73.9 | 90 | |
| Expired at 3 years | 10 | 31.3 | 24 | 26.1 | 34 | |
| Total | 32 | 92 | 124 | |||
| 5-year OS | Right | Left | Total | 0.474 | ||
| Alive at 3 years | 18 | 56.3 | 45 | 48.9 | 63 | |
| Expired at 3 years | 14 | 43.8 | 47 | 51.1 | 61 | |
| Total | 32 | 92 | 124 |
Figure 1. 1a. Median DFS Across Tumor Laterality; 1b. Median OS Across Tumor Laterality.
Majority of the patients’ death were cancer-related in both groups (63.2% in the RCC group and 70.0% in the LCC group; P=.576, see Table 4).
| Cause of Death | Right | Left | Total | P value | ||
| n | % | n | % | 0.262 | ||
| Cancer-related | 12 | 63.2 | 42 | 70 | 54 | |
| Non-cancer related | 5 | 26.3 | 7 | 11.7 | 12 | |
| Unknown | 2 | 10.5 | 11 | 18.3 | 13 | |
| Total | 19 | 100 | 60 | 100 | 79 |
Furthermore, the DFS and OS were still not significantly different after stratification of the population into two subgroups according to stage (early stage for stages I-IIC, and locally advanced stage for stages IIIA-IVA; see Tables 5a and 5b).
| 3-year DFS | RCC | LCC | P value | RCC | LCC | P value | |||||
| Stage I-IIC | n | % | n | % | 0.624 | Stage IIIA-IVA | n | % | n | % | 0.694 |
| Disease-Free at 3 years | 7 | 58.3 | 16 | 66.7 | Disease-Free at 3 years | 9 | 45 | 34 | 50 | ||
| Recurred at 3 years | 5 | 41.7 | 8 | 33.3 | Recurred at 3 years | 11 | 55 | 34 | 50 | ||
| 12 | 24 | 20 | 68 | ||||||||
| 5-year DFS | RCC | LCC | P value | RCC | LCC | P value | |||||
| Stage I-IIC | n | % | n | % | 0.333 | Stage IIIA-IVA | n | % | n | % | 0.612 |
| Disease-Free at 5 years | 6 | 50 | 16 | 66.7 | Disease-Free at 5 years | 5 | 25 | 21 | 30.9 | ||
| Recurred at 5 years | 6 | 50 | 8 | 33.3 | Recurred at 5 years | 15 | 75 | 47 | 69.1 | ||
| 12 | 24 | 20 | 68 |
| 3-year OS | RCC | LCC | P value | RCC | LCC | P value | |||||
| Stage I-IIC | n | % | n | % | 1 | Stage IIIA-IVA | n | % | n | % | 0.371 |
| Alive at 3 years | 10 | 83.3 | 20 | 83.3 | Alive at 3 years | 12 | 60 | 48 | 70.6 | ||
| Expired at 3 years | 2 | 16.7 | 4 | 16.7 | Expired at 3 years | 8 | 40 | 20 | 29.4 | ||
| 12 | 24 | 20 | 68 | ||||||||
| 5-year OS | RCC | LCC | P value | RCC | LCC | P value | |||||
| Stage I-IIC | n | % | n | % | 0.629 | Stage IIIA-IVA | n | % | n | % | .728 |
| Alive at 5 years | 8 | 66.7 | 14 | 58.3 | Alive at 5 years | 10 | 50 | 31 | 45.6 | ||
| Expired at 5 years | 4 | 33.3 | 10 | 41.7 | Expired at 5 years | 10 | 50 | 37 | 54.4 | ||
| 12 | 24 | 20 | 68 |
The total recurrence rate of the entire population in their lifetime was at 66.1%. The incidence of disease recurrence is also similarly distributed between both groups (65.6% in the RCC group and 66.3% in the LCC group; P=.944) (see Table 6).
| Recurrence | Right | Left | Total | P value | ||
| n | % | n | % | 0.944 | ||
| Yes | 21 | 65.6 | 61 | 66.3 | 81 | |
| No | 11 | 34.4 | 31 | 33.7 | 43 | |
| Total Count | 32 | 92 | 124 |
New malignancies occurred in 8.7% of the entire population and was more commonly observed in the RCC group (21.7% of recurrences in the RCC group and 5.1% in the LCC group; P=.022). Majority of the patients in both groups had recurrence in distant site/s (61.1% in the RCC group and 69.4% in the LCC group; P=.501; see Table 7).
| Metastatic Site | Right | Left | Total | P value | ||
| n | % | n | % | 0.06 | ||
| Locoregional | 7 | 30.4 | 17 | 28.8 | 24 | |
| Distant | 11 | 47.8 | 39 | 66.1 | 50 | |
| New cancer | 5 | 21.7 | 3 | 5.1 | 8 | |
| Total | 23 | 59 | 82 | |||
| Site of distant metastasis across laterality* | ||||||
| Brain | 2 | 18.2 | 0 | 0 | 2 | |
| Lung | 5 | 45.5 | 24 | 61.5 | 29 | |
| Liver | 5 | 45.5 | 19 | 48.7 | 24 | |
| Non-regional lymph node | 0 | 0 | 1 | 2.6 | 1 | |
| Bone | 1 | 9.1 | 2 | 5.1 | 3 | |
| Adrenal | 1 | 9.1 | 0 | 0 | 1 | |
| Kidney | 0 | 0 | 1 | 2.6 | 1 |
*Distant metastatic lesions which occurred synchronously and metachronously were both included.
The most common site of distant metastasis in both groups were the lungs, and liver. Majority of patients in both groups (65.6% in the RCC and 67.4% in the LCC group; P=.854) already had disease recurrence at 5 years and only 2 patients (1.6%) developed recurrence beyond 5 years.
Discussion
There is abundance of evidence on the survival outcomes of patients with metastatic colorectal cancer. However, the prognostic data on the non-metastatic setting are inconsistent when stratified according to stage and remains under investigation. Multiple retrospective studies showed a better DFS rate in the LCC as compared to RCC population in the adjuvant setting, especially at stage III [3-5]. In contrast, a larger study using the SEER-Medicare database in Northern America showed a lower mortality in the RCC compared to the LCC group in the patients with stage II disease (adjusted hazard ratio, 0.865; P=.001) [6]. In this study, we determined the survival outcomes of patients with early to locally advanced colorectal adenocarcinoma (stage I to IVA) after definitive treatment and its correlation with tumor laterality. The incidence of LCC is higher than the RCC in the entire population across all stages (74.2% vs 25.8%), and is similar to current figures reported in the United States [7]. Both age and sex ratio were not significantly different between the two groups in contrast to various cohort studies citing propensity of RCC to females and the occurrence of LCC more frequently in age of 50 years and above as compared to RCC [8-10]. Almost all of the patients in both groups received adjuvant oxaliplatin- based chemotherapy on the basis of stage, and adverse clinical features such as: poorly differentiated histology, perineural/lymphovascular invasion, obstruction and/ or perforation at the time of diagnosis, harvested lymph nodes <12 during surgery, and close/indeterminate/ positive margins of resection. Majority of the patients had a locally advanced stage at diagnosis in both groups (62.6% in the RCC and 73.9% in the LCC group).
The results of this study paralleled the findings of Lim, et. al exhibiting more frequent poorly differentiated histology in the RCC group (68.8% vs 13.0%; P<.001). However, other poor prognostic features (such as more advanced N stage, larger tumor size, more positivity of PNI/LVI) that were present in the RCC group of the former study were not found to be similar in our findings. Obstruction at diagnosis was more commonly observed in the LCC group (6.3% vs 28.3%; P=.005) and is consistent with well-known differences in clinical presentation in which the RCC group often presents with symptoms of anemia and weight loss, whereas the LCC group presents with changes in bowel habits, and overt bleeding [11]. No cases of intestinal perforation were noted in both groups. Other clinical adverse features were also similarly distributed.
In this study, there is no statistically significant difference in the 3-year and 5-year DFS between the two groups (see Table 2). Similarly, the 3-year and 5-year OS rates were also non-significant in both groups (see Table 3). Unfortunately, the study is not powered to conclude a stage-specific correlation of survival due to the limited sample size. However, when the stage groups were dichotomized into early and locally advanced clusters, the results did not show a significant difference in all survival outcomes across the stage and laterality (see Tables 5a and 5b).
The development of new malignancies in other organs has been more frequently observed in the RCC group (21.7% vs 5.1%; P= .002). This finding concurs with the literature that hereditary syndromes as cause of CRC are most often seen in the right side of the colon apart from Familial Adenomatous Polyposis (FAP) which tend to occur more in the left side [12].
There are several limitations in this study including the retrospective study design, small sample size that precluded the correlation of outcomes to specific stages and anatomic tumor location and being done in a single institution. Further studies are necessary to validate the findings of this research, ideally with a larger sample size and in a multicenter setting. Insights on the genomic and molecular profile of these patients can help future researchers analyze the possible linkages to the difference in outcomes in the context of stage-specific management.
In conclusion, the findings did not show significant difference in the survival outcomes in non-metastatic colorectal adenocarcinoma when compared by laterality. More diverse clinical characteristics other than tumor location may be of prognostic value in this population.
References
- 2015 Philippine Cancer Facts and Estimates Laudico A V, Mirasol-Lumague MR, Medina V, Mapua CA, Valenzuela FG, Pukkala E, et al . Philipp Cancer Soc.2015;:1-79.
- Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, et al . Available from: https://gco.iarc.fr/today, accessed [20 May 2021]..
- Differences in Cancer-Specific Mortality of Right- Versus Left-Sided Colon Adenocarcinoma: A Surveillance, Epidemiology, and End Results Database Analysis Wang Chenyang, Wainberg Zev A., Raldow Ann, Lee Percy. JCO Clinical Cancer Informatics.2017;(1). CrossRef
- Mortality by Stage for Right- Versus Left-Sided Colon Cancer: Analysis of Surveillance, Epidemiology, and End Results–Medicare Data Weiss Jennifer M., Pfau Patrick R., O'Connor Erin S., King Jonathan, LoConte Noelle, Kennedy Gregory, Smith Maureen A.. Journal of Clinical Oncology.2011;29(33). CrossRef
- Comparison of oncological outcomes of right-sided colon cancer versus left-sided colon cancer after curative resection Lim Dae Ro, Kuk Jung Kul, Kim Taehyung, Shin Eung Jin. Medicine.2017;96(42). CrossRef
- Comparison of 627 patients with right- and left-sided colon cancer in China: Differences in clinicopathology, recurrence, and survival Qin Qiong, Yang Lin, Sun Yong-Kun, Ying Jian-Ming, Song Yan, Zhang Wen, Wang Jin-Wan, Zhou Ai-Ping. Chronic Diseases and Translational Medicine.2017;3(1). CrossRef
- Colorectal cancer statistics, 2017 Siegel Rebecca L., Miller Kimberly D., Fedewa Stacey A., Ahnen Dennis J., Meester Reinier G. S., Barzi Afsaneh, Jemal Ahmedin. CA: A Cancer Journal for Clinicians.2017;67(3). CrossRef
- Are there two sides to colorectal cancer? Iacopetta Barry. International Journal of Cancer.2002;101(5). CrossRef
- Review of Histopathological and Molecular Prognostic Features in Colorectal Cancer Marzouk Ola, Schofield John. Cancers.2011;3(2). CrossRef
- A nationwide Danish cohort study challenging the categorisation into right-sided and left-sided colon cancer Jess Per, Hansen Iben Onsberg, Gamborg Michael, Jess Tine. BMJ Open.2013;3(5). CrossRef
- Left and right sided large bowel cancer Richman S.. BMJ.2002;324(7343). CrossRef
- Difference Between Left-Sided and Right-Sided Colorectal Cancer: A Focused Review of Literature Baran Burcin, Mert Ozupek Nazli, Yerli Tetik Nihal, Acar Emine, Bekcioglu Omer, Baskin Yasemin. Gastroenterology Research.2018;11(4). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2021
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times