Disease Free Survival in Locally Advanced Breast Cancer: An Analysis of Clinical and Pathological Factors
Download
Abstract
Background: The TNM stage is the widely accepted tool to predict prognosis in breast cancer cases, but it deals with a limited range of factors and ignores patient-specific conditions, pathological or genotype characteristics and treatments. The purpose of this study was to evaluate if and how different clinical (tobacco chewing, age etc) and pathological (lymphovascular and perineural invasion etc) variables influence the disease free survival.
Material and Methods: This study involves North Eastern Indian population. Data of 101 patients with locally advanced breast cancer diagnosed in the time period of January to December 2018 was probed and they were followed up till March 2020. Association between various clinicopathological risk factors and disease free survival was assessed using univariate and multivariate models. Survival estimates were computed using the Kaplan-Meier method and differences between survival times were assessed by means of the Log rank test. Multivariate analyses were carried out using Cox’s proportional hazards model.
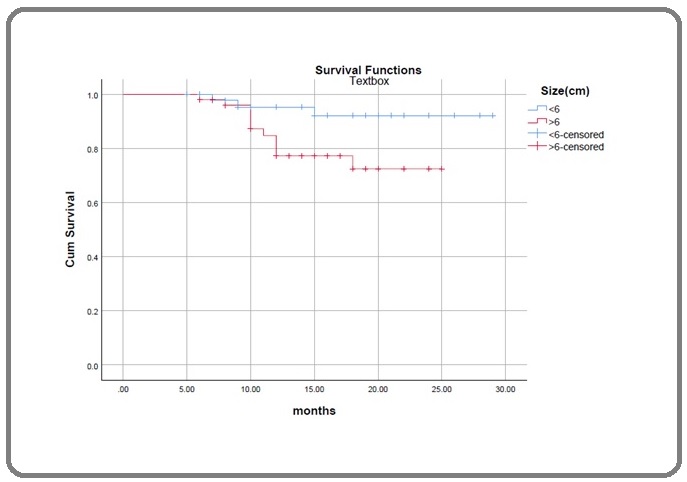
Results: During follow up period 14 patients developed metastasis. There was significantly reduced disease free survival seen trough Kaplan Meier plots in patients having tumor size >6 cm, N2/ N3 stage, triple negative receptor status, tobacco chewing and positive perineural invasion. Multivariate analysis revealed that stage (N2, N3) and positive perineural invasion are two independent variables which adversely affect the survival.
Conclusion: Bottom line of the study is that, disease free survival in LABC patients is significantly reduced with higher stage (N2, N3) and positive perineural invasion as revealed by multivariate analysis. Three other factors which adversely affect DFS are tobacco chewing, tumor size > 6cm and triple negative hormone receptor status according to univariate analysis.
Introduction
Breast cancer is a highly heterogeneous disease with diverse clinical and genetic characteristics. The overall 5-year relative survival rate is 99% for localized diseases and 86% for regional diseases, which drops to 27% for distant-stage diseases.
Locally advanced breast cancer is affected by many clinicopathologic features of patients, such as age, race, marital status, performance status as well as tumor size, lymph nodes status, metastatic sites, number of metastatic sites, pathological or genotype characteristics and previous medical treatments. Therefore, an accurate estimation of survival may benefit patients significantly in decision- making. The TNM stage is the widely accepted tool to predict the prognosis of patients, but it deals with a limited range of factors and ignores patient-specific conditions, pathological or genotype characteristics, and treatments. Therefore, it is still difficult to make precise predictions about individual prognoses for LABC using this method.
Analysis of DFS and associated factors enables a better understanding of the profile of the patients and of recurrence-related characteristics, providing a basis for more suitable therapeutic guidance. It should be noted, however, that studies in the national literature conducted to investigate the recurrence of the disease and its related factors in the North Eastern Indian population context are very scarce.
Materials and Methods
We probed a study population of 450 female breast cancer patients presenting to State Cancer Institute , Guwahati Medical College and Hospital in the year 2018 (January to December). Our study cohort consisted of 101 breast cancer patients who fulfilled the following inclusion criteria.
Inclusion Criteria
1. Female patient with confirmed unilateral breast carcinoma.
2. TNM stages T3N1, N2-N3 with any T and T4 with any N.
3. Patients who completed their treatment.
Disease free survival period was calculated from the date of diagnosis. Outcome of interest (event) is the recurrence of disease either in the form of local recurrence or distant metastasis. DFS is expressed as number of months from the date of diagnosis till occurrence of event. Triple Negative cases were defined as those with ER, PR and Her2 Neu receptors negative. After diagnosis and proper staging, cases were discussed in Multidisciplinary tumor board meeting and treatment plan was charted for each patient. According to the plan neoadjuvant chemotherapy, surgery, adjuvant chemotherapy, radiation therapy and hormonal therapy was administered. Patients were followed till March 2020.
Statistical analysis
In this study, the clinical-pathological parameters analyzed were age, tobacco chewing, tumor size, biopsy report, clinical stage of lymph nodes involvement, ER, PR status, Her2Neu status and triple negative cases. Then after surgery, important features in histopath report like lymphovascular invasion (LVI), perineural invasion (PNI), number of nodes which revealed metastasis and microscopic involvement of nipple areola complex (NAC). The baseline characteristics of patients and treatment were described using summary statistics, with continuous variables being shown as mean ± standard deviation.
Survival estimates were computed using the Kaplan- Meier method and Log-rank test was used for comparison of the survival functions for each variable. Factors with statistical significance (p<0.05) in univariate analysis were taken into multivariate analysis and then analysed. Multivariate analyses were carried out using Cox’s proportional hazards model. We used Cox regression model for proportional hazards, calculating the hazard ratio (HR) and confidence intervals of 95%. All statistical analyses were carried out using the SPSS (version 19.0) software package. P<0.05 was considered significant.
Results
The clinicopathological parameters of 101 patients included in our study are summarized in Table 1.
| Parameters | Metastasis Present (n=14) | Metastasis Absent (n=87) | P value (Log Rank) |
| Age (yrs) | |||
| <45 (n=43) | 7 | 36 | 0.853 |
| ≥45 (n=58) | 7 | 51 | |
| Tobacco | 0.011 | ||
| Yes (n=48) | 11 | 37 | |
| No (n=53) | 3 | 50 | |
| Biopsy | 0.109 | ||
| IDC (n=97) | 13 | 84 | |
| Others (n=4) | 1 | 3 | |
| Size | 0.034 | ||
| < 6cm (n=48) | 3 | 45 | |
| ≥ 6cm (n=53) | 11 | 42 | |
| ER,PR | 0.159 | ||
| Pos (n=56) | 6 | 50 | |
| Neg (n=45) | 8 | 37 | |
| Stage (N) | <.001 | ||
| N1 (n=58) | 3 | 55 | |
| N2,N3 (n=43) | 11 | 32 | |
| Her2neu | |||
| Pos (n=42) | 7 | 35 | 0.451 |
| Neg (n=59) | 7 | 52 | |
| LVI | |||
| Present (n=36) | 7 | 29 | 0.604 |
| Absent (n=65) | 7 | 58 | |
| Pos Nodes in HPE | 0.374 | ||
| <5 (n=69) | 9 | 60 | |
| ≥5 (n=32) | 5 | 27 | |
| PNI | |||
| Present (n=9) | 5 | 4 | <.001 |
| Absent (n=92) | 9 | 83 | |
| Triple Neg case | 0.004 | ||
| Yes (n=22) | 7 | 15 | |
| No (n=79) | 7 | 72 | |
| NAC involved | 0.465 | ||
| Yes (n=10) | 2 | 8 | |
| No (n=91) | 12 | 79 |
Disease free survival for the population studied was 86% at 29 months. Mean follow up period was 14.88 months (Range 6-29). The mean age of our population is 45.7 years. Mean tumor size was 6.03±1.02 cm. 97 (96.4%) patients were found to have IDC (infiltrating ductal carcinoma), 2 patients with infiltrating lobular carcinoma, 1 each with metaplastic carcinoma and carcinosarcoma. 48 (47.8%) patients were tobacco chewers. During follow up period 14 patients developed metastasis. 3 patients with pulmonary, 2 skeletal, 2 local recurrence, 3 brain and 4 had multiple sites metastasis.
Table 1 demonstrates the relation between different clinicopathological factors and their association with recurrence of disease. 48 patients (out of 101) were tobacco chewers and 11 of them developed recurrence. Similarly 9 patients had positive perineural invasion and 5 of these developed recurrence. 43 patients were suffering from N2, N3 disease and 11 out of these developed recurrence. Univariate analysis revealed that positive perineural invasion, N2/N3 stage, tobacco chewing, tumor size > 6 cm and triple negative hormone receptor status have significant association with occurrence of metastasis after full treatment.
There was significantly reduced disease free survival seen through Kaplan Meier plots in these patients. The difference is significant when compared with log rank test. Figures 1, 2, 3, 4 and 5 show the Kaplan Meier survival plots depicting DFS in the significantly associated factors.
Figure 1. DFS According to PNI.
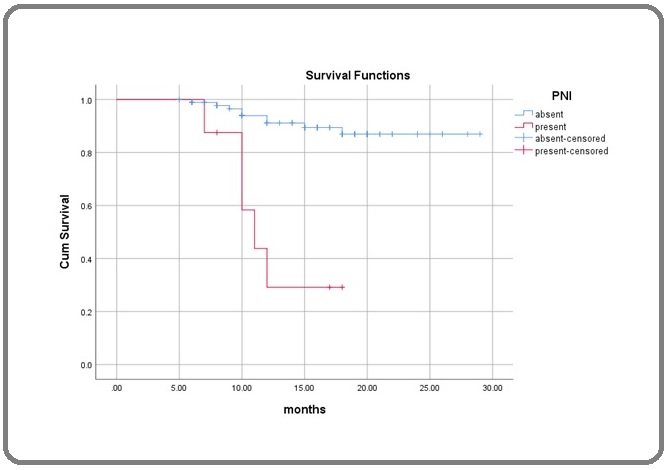
Figure 2. DFS According to Lymph Node Stage.
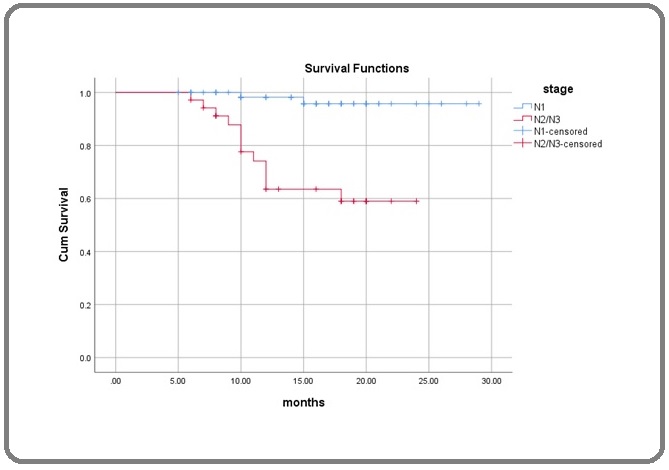
Figure 3. DFS According to Tobacco Chewing Habit.
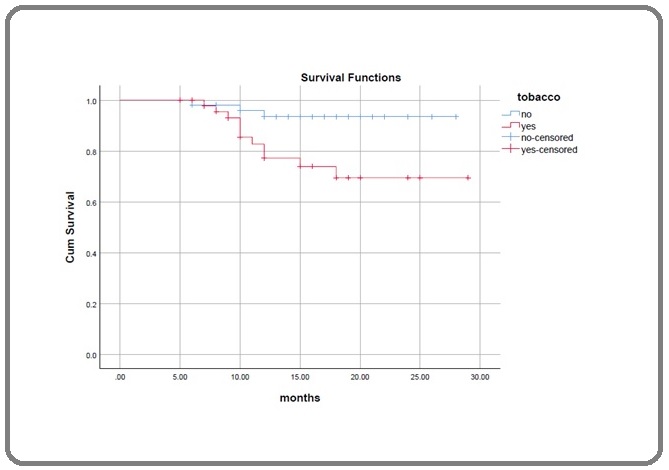
Figure 4. DFS in (TNeg) Triple Negative Hormone Receptor Cases.
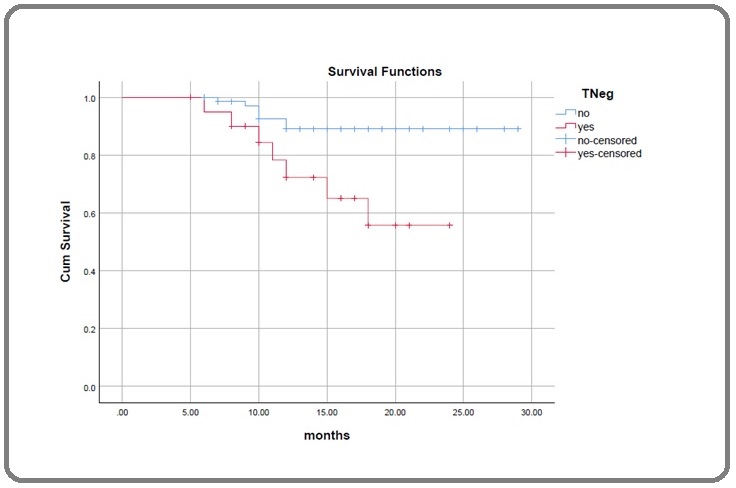
Figure 5. DFS According to Tumor Size.
These five parameters whose p value was <.05 in log rank test were analysed in Multivariate analysis using Cox Regression method. Stage (N2/N3) was found to have hazard ratio 6.732, {95% C.I. 1.376-32.976} with a p value of .019. Therefore it was strongest risk factor for reduced disease free survival. Following the stage was positive perineural invasion (PNI) carrying the risk of recurrence 4.378 times more {95% C.I. 1.196-16.028}. With p value .026, PNI was also found to be significantly associated with poor DFS. None of the other factors were significantly attributable to poor DFS. Although, tobacco chewer patients carried 2.463 times and triple negative cases 2.144 times more risk of recurrence.
| Characteristic | Hazard Ratio | 95% Confidence Interval | P value |
| Tobacco | 2.463 | .624 -- 9.729 | 0.198 |
| PNI | 4.378 | 1.196 -- 16.028 | 0.026 |
| Stage | 6.732 | 1.376 -- 32.926 | 0.019 |
| Size | 2.308 | .598 -- 8.911 | 0.225 |
| Triple Neg | 2.144 | .658 -- 6.991 | 0.206 |
Review of literature
In this study, we found significant association between tumour size (≥6 cm) and decreased DFS, it is in accordance with the findings of Ru Wang et al. [1]. They found that T3 and T4 stage patients are more likely to develop lung metastasis. Similar were the findings of Andy et al. [2] who concluded that unabated tumour growth can contribute to metastasis by selecting for metastatically competent cells. One very important conclusion from our study was that N2/N3 stages significantly reduce DFS. It was confirmed in univariate as well as multivariate analysis. Axillary lymph node involvement is a strong predictor of metastasis and death. Fixed, matted nodes (stage N2/N3) were significantly associated with decreased disease free survival as was the finding of Kyoung ju et al. [3] who classified patients into low, intermediary and high risk according to tumor size, positive lymph node and nuclear grade. Patients who had none of the three risk factors were in the low-risk, with one of these risk factors were classified into the intermediate risk and patients with two or more of these risk factors were classified into the high- risk group. The 5-year disease-free survival rates of the low, intermediate and high risk groups were 93%, 94% and 81%, respectively [3]. In our study, only 5.1% of N1 cases developed recurrence whereas 25.5% of N2/N3 patients had recurrence in the follow up period. Patients having higher nodal stage had significantly less DFS.
Consuming tobacco in the form of oral chewable powder is very common prevalence in North Eastern India. This habit is equally found in males and females. About half of the patients in our study used tobacco and 23% of these developed recurrence. Cigarette smoke exposure is associated with an increase in the total pulmonary metastatic burden in the murine model of metastatic mammary cell cancer [4]. As concluded by Jennifer et al. [5], recurrence was significantly more frequent in current smokers than in never smokers. Current smokers tended to recur sooner than never smokers. Takada et al. [6] studied the recurrence in great detail and found that smoking may induce increased HER2 expression in recurrent breast tumor. Although in all these studies tobacco was used in the form of cigarette smoking which is not the case in our population.
Whereas, the correlation between triple negative receptor status and clinical outcome of patients affected by breast cancer has already been examined in several clinical trials. Other studies focus on molecular subtypes and their association with recurrence of disease and overall survival. We could confirm the results published by Cheng et al. [7] who found that Tneg status decreases DFS in univariate analysis, although in our study Tneg was not an independent prognostic factor in multivariate analysis as was the case with Cheng etal. Tneg status leading to reduced overall survival is widely analysed , it is found to be independent prognostic factor to negatively affect overall survival [8-11]
Compared to other prognostic factors, perineural invasion has received much less attention in literature. Some studies have reported perineural invasion in the name of direct infiltration of nerves, vessels and lymphatic vessels around the nerve tumor. In other studies, perineural infiltration is indicated as a completely separate entity with infiltration of lymphatic vessels and veins. It is emphasized that this is not a true invasion but instead one that results from various mechanisms that promote active epithelial infiltration into the perineural spaces, mechanical implantation due to biopsy trauma and aberrant regeneration of neural and epithelial tissues. Duraker et al. [13] could not identify a correlation of DFS and PNI. Additionally, in earlier studies, no association was found between breast cancer recurrence and PNI. In contrast, the study of Koca et al. [14] and Deger et al. [12] revealed a significant relationship between PNI and DFS, and PNI was associated with the worst prognosis.
Our study results showed in both univariate and multivariate analyses, PNI adversely affects the disease free survival. Therefore, PNI should be considered as a separate prognostic factor that can indicate a poor prognosis
The ASCO and National Comprehensive Cancer Network have released guidelines for breast cancer surveillance [15,16]. Despite minor differences between the guidelines, both recommend history taking and physical examinations every 3 to 12 months for 5 years and then annually. Mammographic evaluation should be done annually. The use of laboratory or imaging studies for metastases screening, such as complete blood counts, chemistry panels, bone scans, chest radiographs, liver ultrasounds, pelvic ultrasounds, computed tomography scans, positron emission tomography scans, magnetic resonance imaging, and tumor markers is not recommended for routine follow-up in the absence of clinical signs and symptoms that suggest disease recurrence. Breast cancer- related costs are increasing and this increase is becoming a social burden [17-19]. Most patients experience a fear of recurrence [20], which is why individual tailored follow-up plans are needed instead of ready-made plans. We aimed to identify whether some patients might need continuous close surveillance whereas, in other patients it might be possible to omit some tests or extend the intervals between surveillance tests. The results of our study lead us to suggest that minor changes in the guidelines for breast cancer surveillance and the follow-up schedule might be worthwhile. From the results from our study, we suggest that the surveillance and follow-up plans should be more frequent for patients who had N2,N3 stage or with positive perineural invasion in the histopath specimen or who have tobacco chewing habit. These patients need continuous care. Mammogram, bone scan, abdominal and pulmonary imaging to screen for metastases/recurrence may be included in their follow ups more liberally as compared to other cases. On the other hand, other patients may need to have only an annual history and physical examination plan with the same mammography schedule if they have been disease free for >3 years.
1.In conclusion N2/ N3 stage, presence of perineural invasion, tobacco chewing, tumor size >6 cm and triple negative hormone receptor status significantly reduce disease free survival according to univariate analysis.
2. In Multivariate analysis Stage (N2, N3) was found to be the strongest risk factor to adversely affect disease free survival followed by perineural invasion.
3. These findings can help to personalize and individualize adjuvant therapy and the follow up examinations. We can schedule the follow up visits of these patients more frequently and for longer duration, as is not anywhere in guidelines till now.
References
- The Clinicopathological features and survival outcomes of patients with different metastatic sites in stage IV breast cancer Wang Ru, Zhu Yayun, Liu Xiaoxu, Liao Xiaoqin, He Jianjun, Niu Ligang. BMC Cancer.2019;19(1). CrossRef
- Lung metastasis genes couple breast tumor size and metastatic spread Minn A. J., Gupta G. P., Padua D., Bos P., Nguyen D. X., Nuyten D., Kreike B., Zhang Y., Wang Y., Ishwaran H., Foekens J. A., van de Vijver M., Massague J.. Proceedings of the National Academy of Sciences.2007;104(16). CrossRef
- Treatment Results and Prognostic Factors of Early Breast Cancer Treated with a Breast Conserving Operation and Radiotherapy Kim K. J.. Japanese Journal of Clinical Oncology.2005;35(3). CrossRef
- The Effect of Cigarette Smoke Exposure on Pulmonary Metastatic Disease in a Murine Model of Metastatic Breast Cancer Murin Susan, Pinkerton Kent E., Hubbard Neil E., Erickson Kent. Chest.2004;125(4). CrossRef
- Smoking and Breast Cancer Recurrence after Breast Conservation Therapy Bishop Jennifer D., Killelea Brigid K., Chagpar Anees B., Horowitz Nina R., Lannin Donald R.. International Journal of Breast Cancer.2014;2014. CrossRef
- The effect of smoking on biological change of recurrent breast cancer Takada Koji, Kashiwagi Shinichiro, Asano Yuka, Goto Wataru, Kouhashi Rika, Yabumoto Akimichi, Morisaki Tamami, Fujita Hisakazu, Shibutani Masatsune, Takashima Tsutomu, Hirakawa Kosei, Ohira Masaichi. Journal of Translational Medicine.2020;18(1). CrossRef
- Prognostic effect analysis of molecular subtype on young breast cancer patients Hong-Liang Chen , Ang Ding , Fu-Wen Wang , et al . . CrossRef
- Evaluation of clinical parameters influencing the development of bone metastasis in breast cancer Diessner Joachim, Wischnewsky Manfred, Stüber Tanja, Stein Roland, Krockenberger Mathias, Häusler Sebastian, Janni Wolfgang, Kreienberg Rolf, Blettner Maria, Schwentner Lukas, Wöckel Achim, Bartmann Catharina. BMC Cancer.2016;16(1). CrossRef
- Molecular Subtypes and Prognostic Factors among Premenopausal and Postmenopausal Thai Women with Invasive Breast Cancer: 15 Years Follow-up Data Tubtimhin Sopit, Promthet Supannee, Suwanrungruang Krittika, Supaattagorn Pongsatorn. Asian Pacific Journal of Cancer Prevention.2018;19(11). CrossRef
- Disease-free survival in patients with non-metastatic breast cancer Diniz Roberta Wolp, Guerra Maximiliano Ribeiro, Cintra Jane Rocha Duarte, Fayer Vívian Assis, Teixeira Maria Teresa Bustamante. Revista da Associação Médica Brasileira.2016;62(5). CrossRef
- The Clinicopathological features and survival outcomes of patients with different metastatic sites in stage IV breast cancer Wang Ru, Zhu Yayun, Liu Xiaoxu, Liao Xiaoqin, He Jianjun, Niu Ligang. BMC Cancer.2019;19(1). CrossRef
- Association between well-known histopathological criteria and overall survival in invasive ductal carcinoma Aysenur Deger , Filiz Ozyigitl , et al . Int J Clin Exp Pathol.2015;8(9):9772-9781 www.ijcep.com.
- Perineural invasion has no prognostic value in patients with invasive breast carcinoma Duraker N., Çaynak Z.C., Türköz K.. The Breast.2006;15(5). CrossRef
- Outcomes of locally advanced breast cancer patients with ≥10 positive axillary lymph nodes Koca Emre, Kuzan Taha Y., Dizdar Omer, Babacan Taner, Sahin Ilyas, Ararat Erhan, Altundag Kadri. Medical Oncology.2013;30(3). CrossRef
- NCCN Clinical Practice Guidelines in Oncology Breast Cancer Version 1.2016 Available at: http://www.nccn.org/professionals/physician_gls/ pdf/breast.pdf [accessed May 9, 2016]..
- Breast Cancer Follow-Up and Management After Primary Treatment: American Society of Clinical Oncology Clinical Practice Guideline Update Khatcheressian James L., Hurley Patricia, Bantug Elissa, Esserman Laura J., Grunfeld Eva, Halberg Francine, Hantel Alexander, Henry N. Lynn, Muss Hyman B., Smith Thomas J., Vogel Victor G., Wolff Antonio C., Somerfield Mark R., Davidson Nancy E.. Journal of Clinical Oncology.2013;31(7). CrossRef
- Older Women With Localized Breast Cancer: Costs And Survival Rates Increased Across Two Time Periods Feinstein Aaron J., Long Jessica, Soulos Pamela R., Ma Xiaomei, Herrin Jeph, Frick Kevin D., Chagpar Anees B., Krumholz Harlan M., Yu James B., Ross Joseph S., Gross Cary P.. Health Affairs.2015;34(4). CrossRef
- Long-Term Financial Burden of Breast Cancer: Experiences of a Diverse Cohort of Survivors Identified Through Population-Based Registries Jagsi Reshma, Pottow John A.E., Griffith Kent A., Bradley Cathy, Hamilton Ann S., Graff John, Katz Steven J., Hawley Sarah T.. Journal of Clinical Oncology.2014;32(12). CrossRef
- Dealing with the financial burden of cancer: perspectives of older breast cancer survivors Pisu Maria, Martin Michelle Y., Shewchuk Richard, Meneses Karen. Supportive Care in Cancer.2014;22(11). CrossRef
- Worry about breast cancer recurrence: a population-based analysis Tewari A, Chagpar AB. Am Surg 2014;80:640–5. Paik et al. Medicine (2017) 96:1 www.md-journal.com..
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times