Rare Case of Mediastinal Myeloid Sarcoma
Download
Abstract
Myeloid sarcoma is a rare tumor mass with extra medullary growth pattern, composed of myeloblast or immature myeloid cells. Myeloid sarcoma (MS) is a distinct clinical presentation of acute myeloid leukemia (AML) where less than 1% of patients present with prominent extra medullary disease which most commonly involves the bone, skin, lymph node, soft tissues, gastrointestinal tract or testes. The recommended treatment regimen in isolated myeloid sarcoma or with bone marrow involvement is upfront systemic chemotherapy. We report a case of a young female with anterior mediastinal mass diagnosed as myeloid sarcoma which was refractory to chemotherapy.
Introduction
Myeloid sarcoma (MS) also called granulocytic sarcoma (GS), myeloblastoma, or chloroma may present simultaneously with or precede bone marrow disease. Typically, myeloid sarcoma may develop as part of acute myeloid leukemia (AML), myeloproliferative neoplasm, myelodysplastic syndrome or it may manifest at relapse, especially in patients following allogenic hematopoietic stem cell transplant [1-3]. As per WHO definition, the tumor itself consists of myeloid blast with or without maturation occurring at an anatomic site other than the bone marrow [4]. The clinical and pathological diagnosis of MS can be highly challenging. The European Society for Hematology recognizes variety of extramedullary manifestation of myeloid neoplasm:
1) MS with concurrent AML; 2) extramedulllary relapse of AML; 3) blast phase/transformation of myeloprolifrative neoplasm; and 4) isolated MS [5]. Isolated MS is a rare entity and has also distinct clinical presentation, reflecting variation in the location and size of MS lesions and most commonly involves the bone, skin, lymph node, soft tissues, gastrointestinal tract and testes.
We are discussing a rare presentation of MS located at unusual anatomical site i.e. anterior mediastinum with poor response to standard treatment.
Case
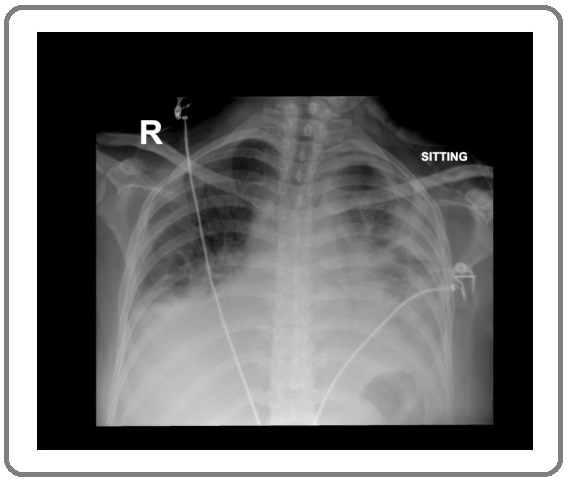
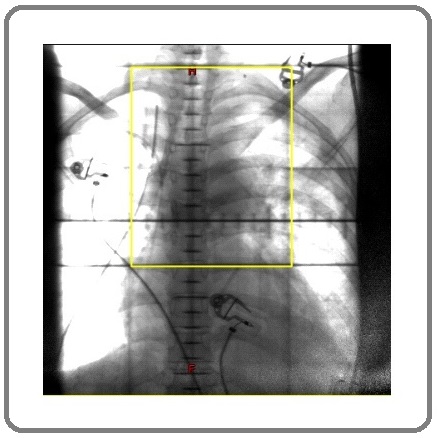
A 25-year-old female presented with history of shortness of breath associated with chest pain, fever, and weight loss for two months. On presentation she was dyspneic. Initial laboratory investigations showed hemoglobin of 11 g/dL, platelet count, 533 × 109/L and white blood cell count (WBC) of 22 × 109/L with differential count of 82 % neutrophils, 10 % lymphocytes, 7 % monocytes, 1 % eosinophils and normal RBC indices. Achest X-ray was done which revealed left sided moderate effusion and right sided mild effusion with mediastinal widening (Figure 1).
Figure 1. Chest Xray (AP view) Showing Left Sided Moderate Effusion and Right Sided Mild Effusion with Mediastinal Widening.
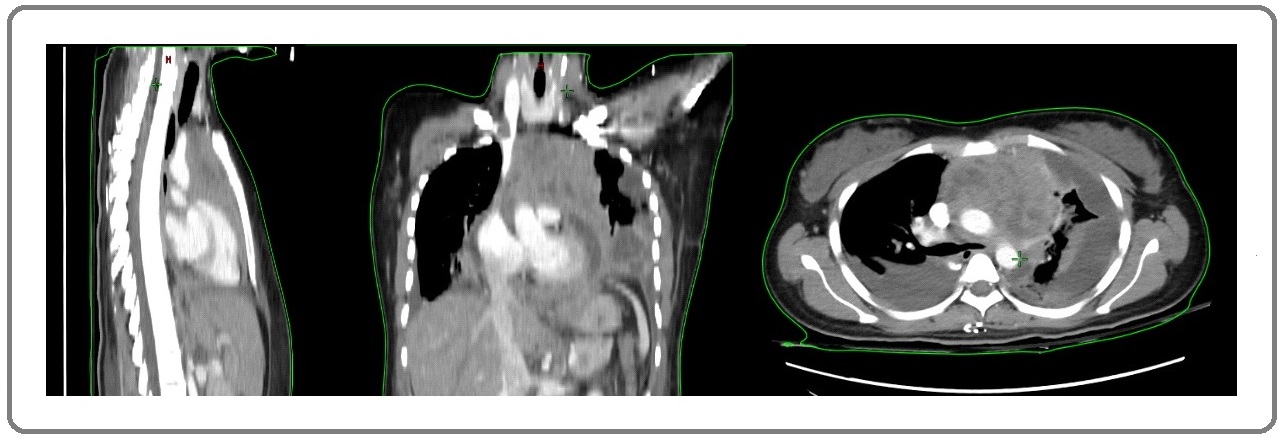
Subsequently, contrast enhanced CT chest, abdomen and pelvis was done which showed, anterior mediastinal heterogeneous soft tissue lesion abutting and displacing the major mediastinal vessels, measuring approximately 95 x 37 x 74 mm in transverse, anteroposterior, and craniocaudal dimensions respectively. (Figure 2).
Figure 2. Pre- chemotherapy CT Scan in Sagittal, Coronal, and Transverse Images Shows a Large Heterogeneously Enhancing Soft Tissue with Internal Necrotic Areas within Anterior Mediastinum, Abutting and Displacing the major Mediastinal Vessels without Evidence of Invasion. Bi basal atelectasis with moderate right pleural effusion and loculated left effusion with enhancing plural suggesting.
Concomitantly, there was presence of pulmonary embolism involving subsegmental branches of right lower pulmonary artery with right sided pleural effusion and left sided loculated effusion (Figure 1). After discussion in multidisciplinary case discussion meeting, it was recommended to perform pleural fluid drainage followed by left sided video-assisted thoracoscopic surgery (VATS) for decortication and biopsy of mediastinal mass. The patient received broad spectrum antibiotics along with therapeutic anticoagulation with insertion of bilateral chest tubes. Morphologically, the mediastinal mass biopsy showed presence of sheets of neoplastic cells which were pleomorphic, with vesicular nuclei, variably prominent nucleoli and abundant eosinophilic to clear cytoplasm (Figure 3).
Figure 3. Showing Images at 40 X, Sheets of Neoplastic Cells with Positive MPO, CD43, and Increase Ki-67.
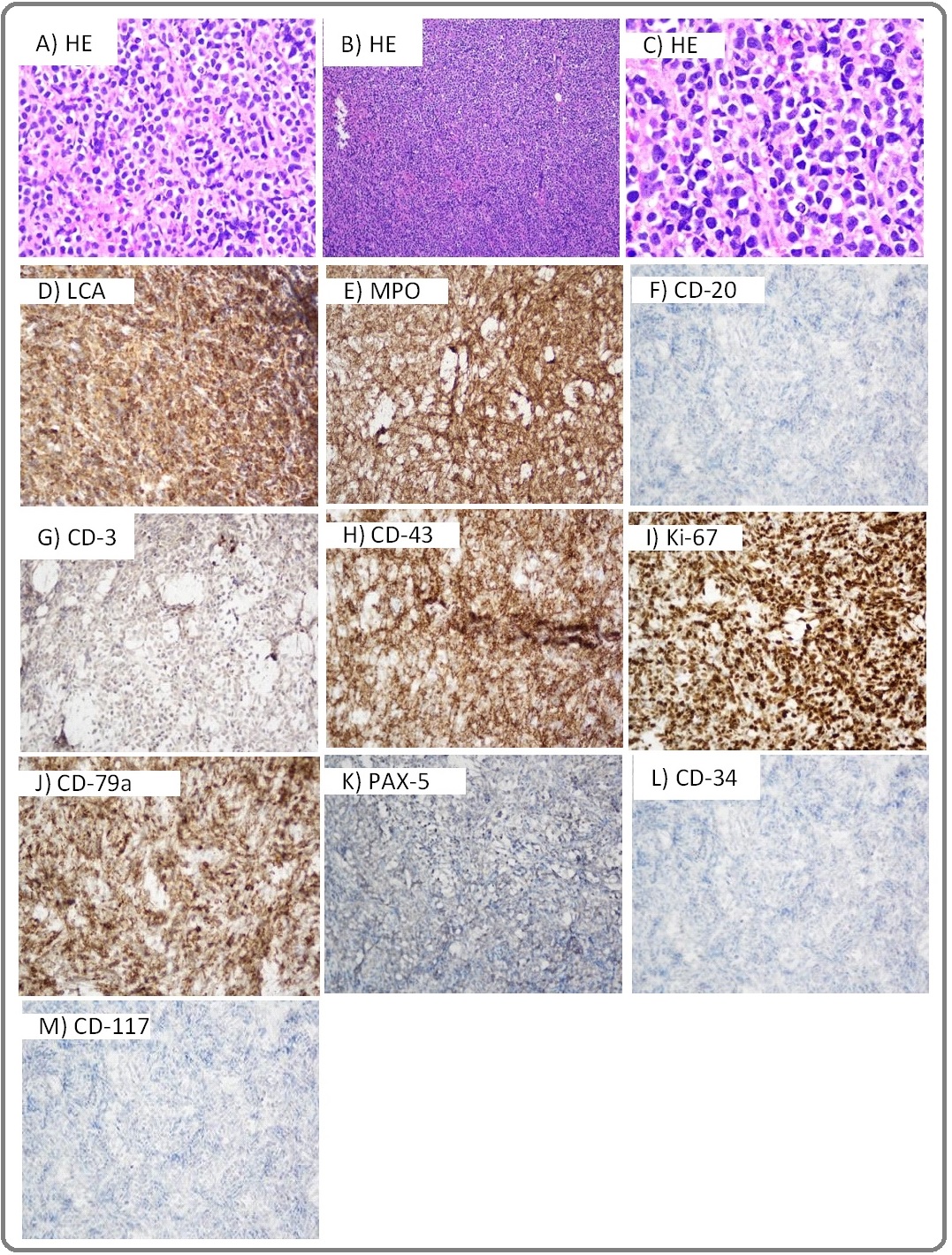
Immunohistochemistry stained positive for myeloperoxidase (MPO), CD-79a and CD-43 while it was negative for CD3, CD-20, PAX-5, CD-23, CD-117, CD-68, CD-30 and CD34. Considering her diagnosis bone marrow biopsy and immunophenotyping by flowcytometry of pleural fluid was done which showed no involvement with blast cells. Therefore, she was labelled as a case of primary myeloid sarcoma.
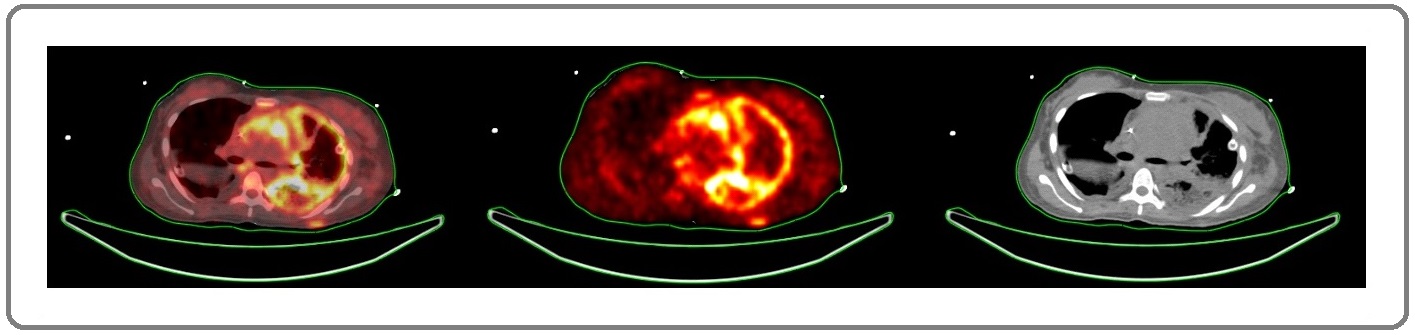
She received induction chemotherapy with 3+7 regimen i.e., Daunorubicin 50mg/m2 (3 days) and Cytarabine 100 mg/m2 (7 days). Her subsequent radiological scans showed no significant improvement, indicative of refractory/resistant disease (Figure 4).
Figure 4. Post Induction Chemotherapy after 3 Weeks, FDG PET/CT for Response Evaluation Showed Ill-defined Soft Tissue Mass with Nonhomogeneous Metabolic Activity is Seen in Anterior Mediastinum Inseparable from Large Vessels, no Appreciable Change in Size Seen.
Clinically, her condition worsened as she remained on continuous non-invasive ventilation support (bilevel positive airway pressure – BiPAP) for persistent tachycardia and tachypnea which was secondary to worsening pleural effusion and bronchopneumonia. After expert consultation with the cardiothoracic team, she underwent repeat right sided VATS and decortication for loculated pleural effusion.
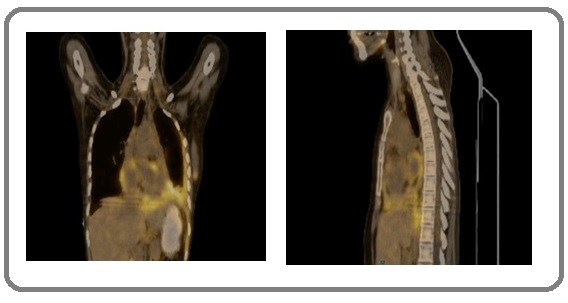
Considering chemo resistant disease, radiation oncology was consulted for treatment and was offered radiation therapy on urgent basis with initial 2D (2 dimensional) technique (Figure 5).
Figure 5. 2-D Based Radiation Therapy, Yellow Lines show Radiation Portal Field that was Treated with Anterior - posterior Arrangement.
After 2 fractions of radiation therapy her clinical condition improved significantly (BiPAP support was discontinued) so it was proposed to switch her to CT Based 3D (3 dimensional) conformal radiation therapy which shows a response to initial two fractions of radaition therapy (Figure 6 and 7).
Figure 6. Coronal, Sagittal and Axial Cuts Showing Response in Mediastinal Mass in Radiation Planning CT Scan.

Figure 7. Coronal, Sagittal and Axial Views Showing 50% Iso Dose Levels (in blue – at periphery) and Red Isodose Dose Wash (at center) Covering 95% Isodose Coverage for Target Region to be Covered with 30 Gray in 10 Fractions at 3 Gray Per Fraction.
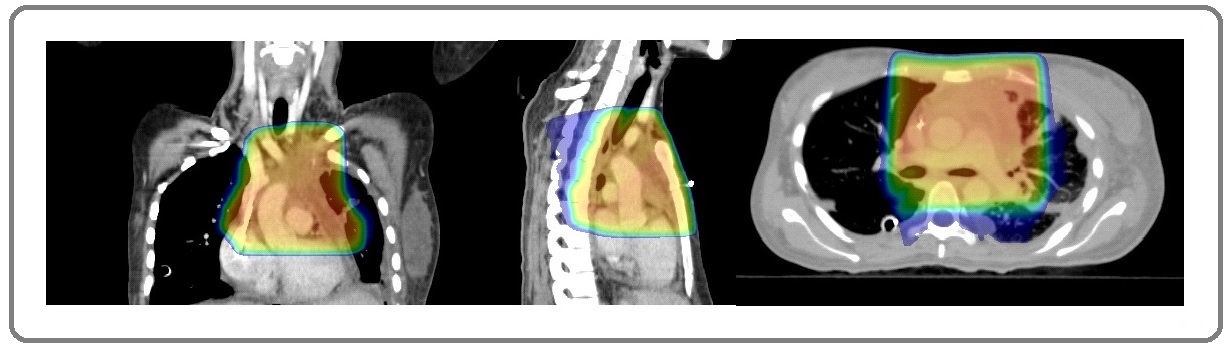
She completed 10 fractions at 3 Gray per fraction over two weeks with cumulative dose of 30 Gray. Eventually, she was discharged from in-patient services in a stable condition and without NIV support.
Four weeks after discharge, her follow up contrast enhanced CT scan of chest, abdomen and pelvis showed further reduction in the size of anterior mediastinal mass, however there was development of pleural thickening along the left crus of the diaphragm and few retroperitoneal nodes. Subsequently, PET/CT scan after two weeks showed further reduction in size and FDG uptake of anterior mediastinal mass (Figure 8). She was then planned for systemic second line chemotherapy.
Figure 8. Post Radiation PETCT Shows Interval Regression in Size and FDG Avidity in Ill-defined Soft Tissue Mass in Anterior Mediastinum (greater than 30% metabolic regression).
She was then planned for systemic second line chemotherapy.
Discussion
As isolated myeloid sarcoma is a very rare entity frequently resembling lymphoma in clinical presentation. It poses a major diagnostic challenge for both pathologists and clinicians. We report a similar case of a 25-year- old female who was diagnosed as myeloid sarcoma on anterior mediastinal mass. Mediastinal primary myeloid sarcoma (MS) is extremely rare and only few case reports have been published in literature. This entity has a high rate of misdiagnosis. i.e., 46% and is misdiagnosed as lymphoma [6]. Immunohistochemical detection of intracellular myeloperoxidase (MPO), a major constituent of primary granules of neutrophilic myeloid cells, confirms a diagnosis of MS. The diagnosis is based on immunohistochemical stains which include CD13 and CD68 (markers for granular monocytic and macrophagic cells), MPO and CD117 (markers for myeloid differentiation), lysozyme marker for monocytic lineage, CD43 (marker for myeloid cells, T and B cells), and CD34 and terminal deoxynucleotidyl transferase (TdT) (markers for immature cells) [7]. In our patient’s case, immunohistochemical evaluation revealed strong positivity of MPO and CD43. Due to limited prospective trials, treatment strategies for MS are not well established but because most of patients with isolated MS progress to AML, systemic chemotherapy is recommended treatment of choice followed by consolidation similar to AML [8]. Retrospective series have demonstrated that isolated MS treated with local radiotherapy alone has a high rate of progression to AML and a short no leukemic interval [9, 10]. The use of radiotherapy is also not well studied as a prospective means of treatment of MS but can produce excellent, durable local control at the targeted site; however, it is also an inadequate treatment option unless used in combination with systemic chemotherapy [11].
A series of 21 patients with isolated MS demonstrated that disease recurrence was lower in a group that received chemo-radiotherapy than those receiving radiotherapy alone [12]. Another retrospective series that included 90 patients also demonstrated that, local radiotherapy had no effect on overall survival. Hematopoietic stem cell transplantation (HSCT) also used, retrospectively, in MS patients, reported data showed an advantage of both auto or allo-HSCT in MS patients with or without concomitant AML irrespective of age, gender, anatomic location clinical presentation or cytogenetic status [8, 10, 13]. Our patient did not respond to standard systemic chemotherapy, but she showed excellent reduction of mediastinal mass after low dose radiotherapy. According to literature, radiation therapy for the MS is effective to achieve response but it does not improve the disease-free interval and the overall survival. Therefore, chemotherapy is recommended even with initial response to radiation similar to the treatment of acute myeloid leukemia [10]. This patient has been planned for systemic chemotherapy followed by allogenic stem cell transplant.
In Conclusion, myeloid sarcoma is a rare entity and lacks standardized treatment protocols. Our patient with anterior mediastinal mass diagnosed as MS who was chemo-refractory but responded to radiation therapy, way forward will be to treat her with systemic chemotherapy followed by allogeneic stem cell transplant.
References
- Myeloid Sarcoma Campidelli Cristina, Agostinelli Claudio, Stitson Richard, Pileri Stefano A.. American Journal of Clinical Pathology.2009;132(3). CrossRef
- Trilineage extramedullary myeloid cell tumor in myelodysplastic syndrome Hancock JC, Prchal JT, Bennett JM, Listinsky CM. Archives of pathology & laboratory medicine.1997;121(15):520.
- Lateral pharyngeal wall myeloid sarcoma as a relapse of acute biphenotypic leukemia: a case report and review of the literature Alrumaih Redha, Saleem Muhammad, Velagapudi Suresh, Dababo Mohammad Anas. Journal of Medical Case Reports.2013;7(1). CrossRef
- Non-leukemic myeloid sarcoma involving the vulva, vagina, and cervix: a case report and literature review Yu Yuan, Qin Xuemei, Yan Shuxin, Wang Wenxia, Sun Yanlin, Zhang Maohong. OncoTargets and Therapy.2015. CrossRef
- Extramedullary Manifestations of Myeloid Neoplasms Wilson Carla S., Medeiros L. Jeffrey. American Journal of Clinical Pathology.2015;144(2). CrossRef
- Extramedullary myeloid cell tumors in acute nonlymphocytic leukemia: a clinical review. Byrd J C, Edenfield W J, Shields D J, Dawson N A. Journal of Clinical Oncology.1995;13(7). CrossRef
- Acute Myeloid Leukaemia Diagnosed by Intra-Oral Myeloid Sarcoma. A Case Report Papamanthos Mattheos K., Kolokotronis Alexandros E., Skulakis Haralampos E., Fericean Angela-Monika A., Zorba Matina T., Matiakis Apostolos T.. Head and Neck Pathology.2010;4(2). CrossRef
- How I treat extramedullary acute myeloid leukemia Bakst Richard L., Tallman Martin S., Douer Dan, Yahalom Joachim. Blood.2011;118(14). CrossRef
- Is there a “gold” standard treatment for patients with isolated myeloid sarcoma? Antic D, Elezovic I, Milic N, Suvajdzic N, Vidovic A, Perunicic M, et al . Biomedicine & Pharmacotherapy.2013;67(1):72-77.
- Comparison in treatments of nonleukemic granulocytic sarcoma Yamauchi Kunihiko, Yasuda Masami. Cancer.2002;94(6). CrossRef
- The Chemokine SDF-1 Is a Chemoattractant for Human CD34+ Hematopoietic Progenitor Cells and Provides a New Mechanism to Explain the Mobilization of CD34+ Progenitors to Peripheral Blood Aiuti A., Webb I.J., Bleul C., Springer T., Gutierrez-Ramos J.C.. Journal of Experimental Medicine.1997;185(1). CrossRef
- Radiation Therapy for Chloroma (Granulocytic Sarcoma) Bakst Richard, Wolden Suzanne, Yahalom Joachim. International Journal of Radiation Oncology*Biology*Physics.2012;82(5). CrossRef
- Prognostic Factors of Treatment Outcomes in Patients with Granulocytic Sarcoma Lan Tsung-Yu, Lin Dong-Tsamn, Tien Hwei-Fang, Yang Rong-Sen, Chen Chih-Yu, Wu Karl. Acta Haematologica.2009;122(4). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2021
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times