Technical Challenges to the Delivery of Quality Radiation Therapy During the COVID-19 Unlock Period: Medical Physics Perspective
Abstract
The Covid-19 onset was very pandemic for all of society all over the world. To overcome this state of affairs, the country’s government had done the lockdown in their respective countries. The lockdown helped the people from spreading the Covid-19 virus among people, however, it affected another part of life such as people becoming unemployed. The health care sector was affected a lot by the lockdown as the patient faced lots of problems such as reaching the hospital, meeting the concerned staff, getting the treatment on time, etc. Covid-19 affected the cancer patients most, during the lockdown. After awareness of Covid-19, when the world has started towards the unlock down. With the little negligence of people, the world has started facing the peak of Covid-19. And, there was more crowd in the health care sectors, therefore the hospital staff got infected a lot, as the patient treatment cannot be carried out from home. Cancer patient treatment, which comes under radiotherapy, has already existed in chronic medical conditions, such as lung cancer patients, esophagus cancer patients, heart disease patients, etc, has a higher risk of Covid-19 infection. During treatment, when such a patient comes in contact with a radiation oncologist, medical physicist, and radiation technologist, then some of the staff get infected through patients. To prevent such spread, all the medical staff should strictly follow the rules made for staff. In this article, we are sharing the challenges for the medical physics team and some suggestions during patient care.
Introduction
Radiotherapy
Radiation therapy is an integral component in the management of almost 50-60% of cancers. It is a great challenge to deliver uninterrupted treatment at the best of times and has become even more of a daunting task during the present crisis.
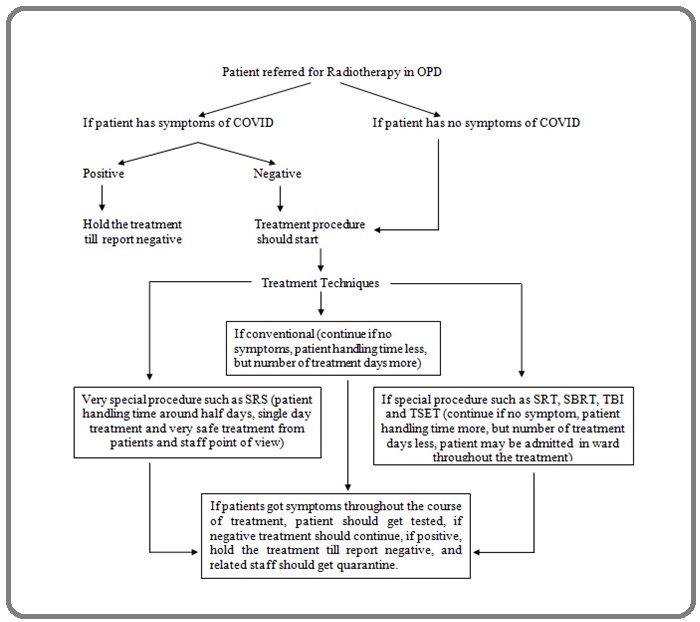
The staff in the department of radiation oncology face similar challenges as they are exposed to patients who travel regularly for treatment as outpatients. This implies that all the stakeholders in the process, the patient, his/ her attendant, the radiotherapy personnel are all at constant risk of exposure and may get infected at any time. The risk seems to be higher in asymptomatic cases despite the enforcement of the infection prevention protocols. The patient treatment decision chart is followed in Figure 1.
Figure 1. Patient Treatment Decision Chart During COVID-19 Crises.
Challenges faced by the Medical Physicist
Medical Physicists play an essential role in radiotherapy who acts as a conduit between physicians, and technologists. They are generally small in number, and uniquely skillful, as compared to other major workforces in a typical cancer hospital environment.
International organizations of Medical Physics (IOMP) and International Atomic Energy Agency (IAEA) have clearly defined the role of medical physicists in a radiation oncology department [1], which include essentials, dosimetry, treatment planning, radiation safety, and quality assurance (QA). In a pandemic situation, tasks related to treatment planning could be easily performed in a work from home (WFH) environment in most of the developed countries, however, in countries like India, including our hospital, could not implement seamless remote treatment planning, due to the lack of infrastructure, in terms of Citrix based server, personal equipment- such as high-end laptop/personal computer at home, or even high bandwidth internet connectivity. Even in certain scenarios, if these above issues could be overcome, major issues such as patient confidentiality, one-to-one physician-physicist interaction to arrive at an optimal plan among other things, remain at large due to lack of regulations and clarity. On the other hand, for tasks related to machine QA, patient-specific QA, dosimetry, radiation safety, the physicists must be present in the hospital physically.
Another major challenge is in brachytherapy services. India is the second-largest country with the incidence of cervical cancer [2], where brachytherapy plays a major role, was a continuous service, wherein physicists must be present physically not only for imaging but also for treatment planning, plan evaluation, and optimization. In addition, during the lockdown period, it was a major challenge to clear the Ir-192 source from the customs, which caused a major delay that resulted in wasting a crucial one-half-life of the isotope.
In certain scenarios, especially in small towns, the equipment breakdowns could not be serviced on time, due to lack of availability of transport or simply non-availability of the engineers, due to the infection, leading to major downtime. In addition, calibration of the dosimetric equipment also was disrupted due to the closure of the major dosimetry laboratories closing for the reasons cited above.
Gaps in the treatment delivery were a major challenge, faced by the medical physicist when patients were not able to travel to the hospital for their treatment. New protocols for handling gaps in delivery which were not familiar to many physicists. A lot of clinics still use the old Time-Dose-Fractionation (TDF) models to calculate the gap correction. Conventional fractionation using 180-200cGy/fraction, 5days a week, over 5-7 weeks is the commonest schedule in use in radiotherapy, using conventional techniques. With the increasing use of conformal radiotherapy and hypo-fractionated schedules with high-precision techniques, the role of the physicist in the day-to-day delivery of treatment has increased.
Presently, there are many advanced techniquesused to treat the patients, such as 3-dimensional conformal arc therapy (3D-CRT), intensity-modulated radiotherapy (IMRT), volumetric modulated arc therapy (VMAT), stereotactic body radiotherapy (SBRT), stereotactic radiotherapy (SRT), stereotactic radiosurgery (SRS) to reduce the incidence of radiation-induced sequelae. In all these treatment modalities the medical physicist plays an important role in patient simulation, treatment planning, treatmentdelivery, and verification.
As the physicist is involved in the entire process, there is a higher likelihood of exposure for the physicist also. This makes it important for the medical physicist who would otherwise not have come in direct contact with the patient, to take the same level of precautions as other members of the team.
Apart from the physics related challenges, other common challenges that include, family pressure – children being at home with schools/daycare centers closed, colleagues/physicists testing positive, quarantine period, hospitalization, loss of a family member, affects the mental health which results in sub-optimal efficiency in work. Hence, a reasonable work-life balance must be aimed to reduce the stress and anxiety associated with mental well-being.
Now, India is facing the second wave of Covid-19, which is highly affecting people’s lives. This wave is more dangerous for young as well as those under 16. In this present scenario, many other sectors are closed for a time being, however, the health sector workload is rising day by day. Many hospitals have converted into Covid-19 hospitals temporarily, still due to a high backlog of cancer patient treatment; the cancer treatment is continued and cannot be avoided. That’s why, in most hospitals, the treatment timing hours are expanding. Another important issue, which is created in the second wave, the patient is becoming Covid-19 positive in course of treatment and going to be isolated for 20 days approximately. That is escalating the workload of medical physicists, such as re-simulation, adaptive planning, gap correction, patient- specific quality assurance. Along with this, the Covid-19 positive risk factor is also high in this environment.
Suggested measures [3-7]
1. While most of the treatment prescription was hypo-fractionated, the physicists must adapt to the changes, both in terms of radiobiology and imaging protocols.
2. Medical Physicist must adopt the same level of infection prevention and control measures as the rest of the team while carrying out duties involving regular and close contact with the patient such as SRS, SBRT, Brachytherapy, especially, wearing-masks, gloves, caps, and personal protective equipment (PPE) kit, whenever necessary.
3. All the treatment documentation paperwork may be converted to paperless, to reduce the handling of infections due to fomites.
4. Medical Physicists must continue to perform all the patient-specific QA other than daily morning QA before handing over the treatment unit to the radiation therapist for treatment.
5. Every morning, before QA, the treatment couch, pendant, console unit, and common immobilization devices (such as a headrest, knee rest, etc) must be sanitized at regular intervals
6. All equipment and accessories in the treatment room should be sanitized appropriately.
7. Similarly, treatment planning systems (TPS) should be sanitized every morning, especially the keyboard, mouse, etc. Use of gloves must be discouraged unless there is physical contact with contaminated articles or patient secretions.
8. There should be a plan to create a reserve workforce, creating a timetable for attendance as necessary for optimal work, while following regulations at the same time.
9. Any staff with symptoms suggestive of infection or history of exposure should immediately report the same to the designated member/ team of the COVID Action group and isolate themselves until appropriate action/ testing has been carried out.
In conclusion, the pandemic shows no signs of abating and most countries in the West are experiencing their second wave. Given the circumstances, the three basic principles of infection prevention and control seem to be the new way of life. All members of the radiation oncology department including the medical physicist will have to stringently adopt and follow these practices at work and away from work.
References
- INTERNATIONAL ATOMIC ENERGY AGENCY, Roles and Responsibilities, and Education and Training Requirements for Clinically Qualified Medical Physicists, Human Health Series No. 25, IAEA, Vienna (2013) .
- Available from: https://www.uicc.org/news/global-cancer-data-globocan-2018, Global Cancer data: GLOBOCAN 2018 .
- Development and execution of a pandemic preparedness plan: Therapeutic medical physics and radiation dosimetry during the COVID-19 crisis Riegel AC, Chou H, Baker J, Antone J, Potters L, Cao Y. J Appl Clin Med Phys.2020;21(9):259-265.
- Revision in standard operating procedures of radiation oncology department and quality assurance schedule under COVID-19 pandemic Chaudhari Suresh, Sharma SunilDutt, Shrivastava ShyamKishore. Journal of Medical Physics.2020;45(2). CrossRef
- Managing Radiotherapy Practice during Coronavirus Disease 2019 Pandemic: Medical Physicist's Perspective Goswami Shachindra, Yadav Bhaveshwar, Sarma Gautam, Barthakur Mithu, Goswami Pranjal. Journal of Radiation and Cancer Research.2020;11(1). CrossRef
- COVID-19 pandemic planning: considerations for radiation oncology medical physics Whitaker May, Kron Tomas, Sobolewski Matthew, Dove Richard. Physical and Engineering Sciences in Medicine.2020;43(2). CrossRef
- Brachytherapy in cervical cancer radiotherapy during COVID-19 pandemic crisis: problems and prospects Miriyala Raviteja, Mahantshetty Umesh. Journal of Contemporary Brachytherapy.2020;12(3). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2021
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times