GIS to Explore the Geographical Mysteries of Oral Cancer: Geospatial Distribution of Patients Diagnosed with Oral Potentially Malignant Disorders at the University Dental Hospital Peradeniya
Download
Abstract
Background: Oral cancers which are often preceded by an oral potentially malignant disorder (OPMD) carries the highest mortality rate among all cancers in Sri Lanka. Dental Teaching Hospital, Peradeniya is one of the tertiary centres in Sri Lanka for treating OPMD with a high patient turnover.
Objectives: This study aimed to determine the geospatial distribution of OPMD patients who attended Dental Hospital, Peradeniya (DHP) using geocoding methods.
Materials and Methods: A retrospective study was done by obtaining data of 869 OPMD patients who visited DHP within the last 4 years to geo-code their addresses using GIS software.
Results: The majority of the sample consisted of oral lichen planus (OLP) (52.47%). 29% and 18.64% of the patients were diagnosed with leukoplakia and oral submucous fibrosis (OSF) respectively. Most of the OPMD patients (60.64%) who visited the clinic were from the Kandy district and surprisingly the majority of OPMD patients had been reported from non-estate areas. The second and third highest number of patients were respectively from Nuwaraeliya (11.28%) and Kegalle (7.48%). More than half (57.19%) of the patients were living within 20 km of the hospital.
Conclusion: The composition of patients with OPMDs visited the DHP had deviated from the national data. More than half of the sample residing within a reasonable travel distance to a specialist care centre.
Introduction
The term ‘oral potentially malignant disorders (OPMD), comprises a diverse group of disorders carrying an increased risk of malignant transformation. This terminology emerged at a World Health Organization (WHO) workshop in 2007 and was defined as ‘the risk of malignancy being present in a lesion or condition either at the time of the initial diagnosis or at a future date’ [1]. An array of disorders are considered as OPMDs including, oral leukoplakia (OL), erythroplakia, oral submucous fibrosis (OSF), oral lichen planus (OLP), discoid lupus erythematosus (DLE), actinic cheilitis and palatal keratosis associated with reverse smoking, chronic hyperplastic candidosis, epidermolysis bullosa and dyskeratosis congenital [2].
Oral cavity cancer is the 2nd most common cancer in Sri Lanka. It lies on top of the list of most common cancers among males and 8th among females [3]. The oral cavity cancers carry the highest mortality rate among all cancers in Sri Lanka [4]. This devastating disease is often preceded by an OPMD which has a global prevalence of 1-5% [5]. According to a large survey done in the Central Province, the prevalence of OPMDs among the Sri Lankan population is estimated at 4.2% [6]. According to the national oral health survey in Sri Lanka, oral leukoplakia and OSF being the commonest OPMDs reported a prevalence of 4.0 and 3.0 per 1000 respectively [7].
Management of oral cancer carries a significant burden on the health care systems in developing countries like Sri Lanka. Diagnosis of the cases at the stage of OPMD offers a significant cost benefit to the healthcare system and morbidity and mortality benefits to the patients [8,9]. The preventive strategies are in search of novel approaches for the early detection of oral cancer. Remarkable observations are seen with the recent approaches which extend to involve modern technology such as artificial intelligence, geographic information science etc [10].
Geographic Information Science (GIS) is defined as ‘the development and use of theories, methods, technologies, and data for understanding geographic process, relationships and patterns’ [11]. It is widely used in land management, urban planning, disaster prevention and mitigation, real estate development, commercial and other areas [12]. GIS has been used in public health care for epidemiologic studies, mapping healthcare resources, health system planning etc., for over the past few years [13]. Even though the potential application of GIS to health systems are enormous it has not yet been utilized in health research to its fullest capability. Referring to the incidence of cancer and mortality rates, GI Science is well recognized as a powerful tool and effective means of communicating and presenting health data. This is enabling visualization to attribute data beyond traditional graphs and charts. Hence, it allows researchers and clinicians to obtain a sound understanding of the spatial relationship of both risk and potential cofounders as well as social and demographic patterns and trends [14].
GIS-based research in the field of oral health is scarce, not only in Sri Lanka but also around the globe [15-17]. The Oral Medicine Clinic of the University Dental Teaching Hospital, Peradeniya is the only dedicated oral medicine clinic in Sri Lanka. The unit is located central to the island (Kandy district) and is recognized for treating, teaching and research in oral cancer and OPMDs. The clinic receives patients not only from the proximities but from the various parts of the island with a significant annual turnover. The study was carried out with the purpose of mapping out the distribution of OPMD patients presented to the Dental Teaching Hospital, Peradeniya within the last 4 years. Further, the authors aimed at exploring the unearthed geospatial mysteries of oral potentially malignant disorders with the data.
Materials and Methods
This study is a cross-sectional descriptive study on the distribution of OPMD patients presented to the Oral Medicine Clinic, Dental Teaching Hospital, Peradeniya from the year 2017 to 2020.
Sources
The study population included patients with OPMDs, diagnosed clinically and confirmed histopathologically. The study sample included OL, OSF and OLP being the three most common OPMDs presented to the clinic [18]. The demographic data, essentially the accurate location of the patients were obtained from the electronic database of the Dental Teaching Hospital, Peradeniya. Patients with incomplete records and repeated records were carefully excluded.
Geocoding Approach
Geocoding of patients’ locations was done using Google Earth Pro (version 7.3.3.7786) software by assigning geographic coordinates to the physical addresses of the locations. All recorded data were transferred into QGIS (version 2.14.1) for ultimate analysis. Patients’ density (patients per square kilometre) in different divisional secretariat divisions (DSD) in the Central Province and different regions in Sri Lanka were mapped using the GIS software. A 20 km buffer was constructed around the DHP, the ‘reasonable distance to a specialist care centre’ adopted by Wijewardena et.al in 2018 [17]. The extracted datasets were transferred into Excel version 365 and further descriptive analysis.
Results
Locations of 869 patients presented to the Dental Teaching Hospital, Peradeniya with three OPMDs during 2017-2020 were geocoded for this research and the males outnumbered females with a percentage of 53%.
Demography
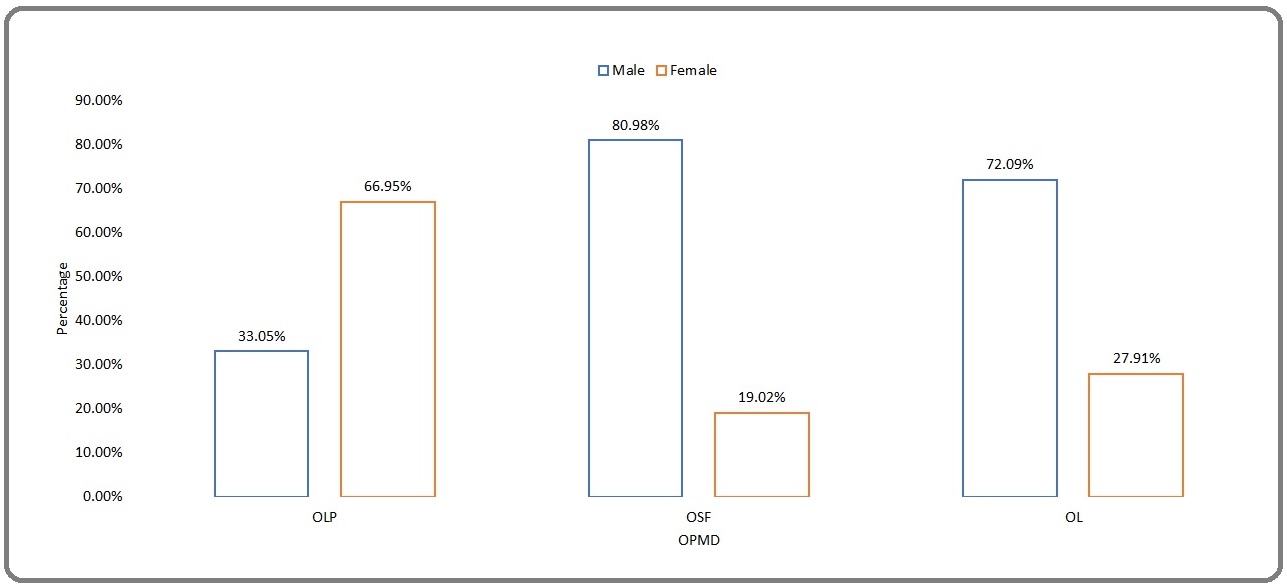
A major proportion of the sample consisted of OLP (52.47%) patients. Approximately 28.88% were diagnosed with OL and 18.64% of them had OSF. However, OLP was predominant among females while most of the OSF and leukoplakias were seen among males (Figure 1).
Figure 1. Gender Distribution of OLP, OSF and OL.
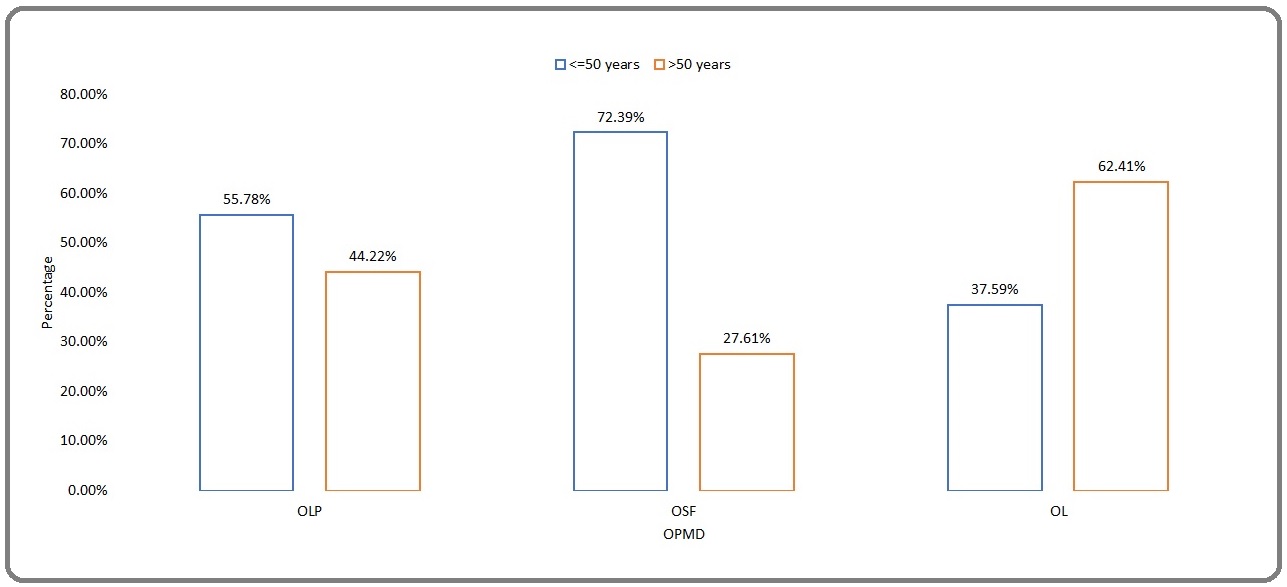
Although OL was the predominant OPMD seen among patients over 50 years, OLPs and OSFs dominated in the group below 50 years (Figure 2).
Figure 2. Age Distribution of OLP, OSF and OL.
Geography
At the outset majority of the patients presented to the clinic (76.17%) were living in the Central province.
The Kandy district, Nuwara Eliya district and Matale district are the districts of the Central province. District- based analysis revealed that most of the OPMD patients (60.64%) presented to the clinic were residents of the Kandy district while the second being the Nuwara Eliya district with a proportion of 11.28%. Surprisingly the 3rd highest number of patients were reported from Kegalle (7.48%) district belongs to adjacent Sabaragamuwa province (Figure 3).
Figure 3. Distribution of the OPMD Patients Attended the Clinic among Districts in Sri Lanka.
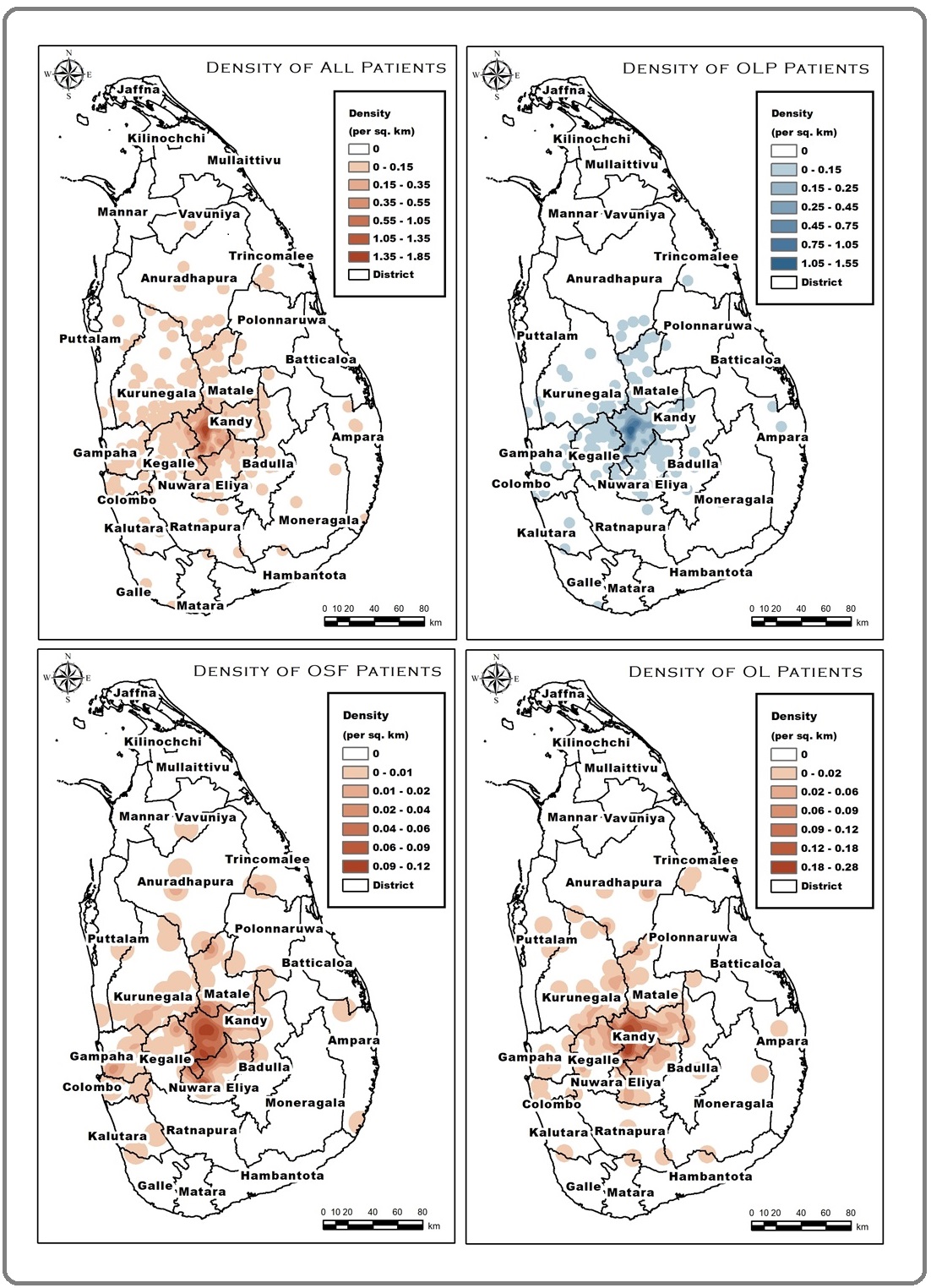
The geographic distribution of OLP, OSF and OL among districts are elaborated in Table 1 and Figure 3.
| OPMD | OSF | OLP | OL | |||||||||
| District | No. of Pts | % | District | No. of Pts | % | District | No. of Pts | % | District | No. of Pts | % | |
| 1 | KAN | 527 | 60.64 | KAN | 77 | 47.53 | KAN | 309 | 67.76 | KAN | 141 | 56.18 |
| 2 | NUW | 98 | 11.27 | NUW | 31 | 19.14 | NUW | 41 | 8.99 | NUW | 26 | 10.36 |
| 3 | KEG | 65 | 7.48 | KUR | 12 | 7.41 | KEG | 36 | 7.89 | KEG | 25 | 9.96 |
| 4 | KUR | 50 | 5.75 | MAT | 9 | 5.56 | KUR | 19 | 4.17 | KUR | 19 | 7.57 |
| 5 | MAT | 37 | 4.26 | GAM | 7 | 4.32 | MAT | 19 | 4.17 | MAT | 9 | 3.59 |
KAN, Kandy; NUW, Nuwaraeliya; KEG, Kegalle; KUR, Kurunegala; MAT, Matale; GAM, Gampaha
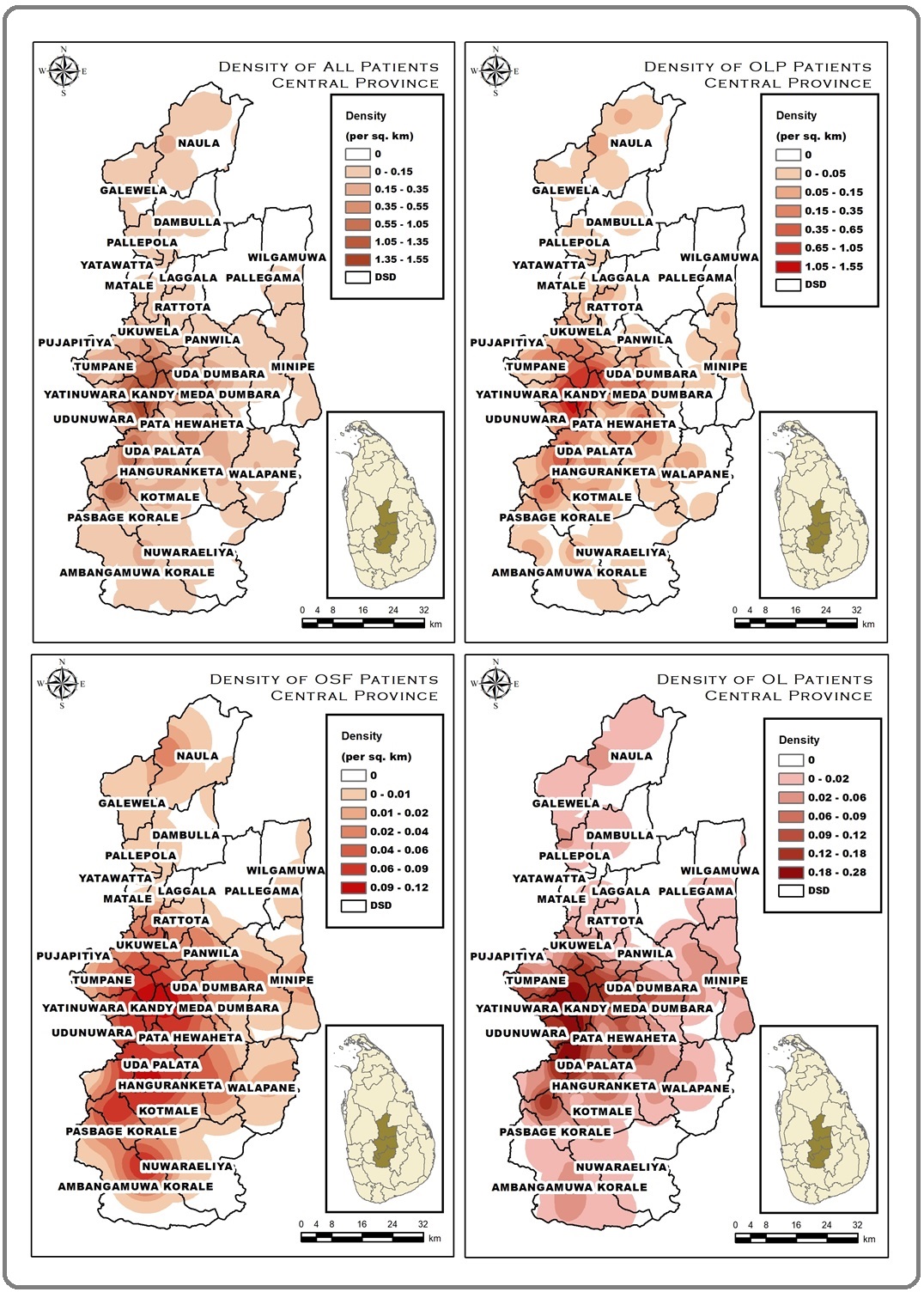
The ‘divisional secretarial divisions’ represent the lower administration unit to the districts in the administrative hierarchy of Sri Lanka. The Yatinuwara Divisional Secretariat Division (DSD) of Kandy district reported the highest number of OPMD patients (7.83%) in the Central Province. Gangawata Korale (7.13%) and Udunuwara (5.75%) DSDs reported the 2nd and 3rd highest. Table 2 illustrates the DSDs with the highest frequency of patients in each OPMD (Figure 4, Table 2).
Figure 4. Distribution of the OPMD Patients who Attended the Clinic among DSDs in Central Province.
| OPMD | OSF | OLP | OL | |||||||||
| DSD | No. of Pts | % | DSD | No. of Pts | % | DSD | No. of Pts | % | DSD | No. of Pts | % | |
| 1 | YAT | 68 | 7.83 | AMB/KOT | 10 | 6.17 | GAN | 44 | 9.65 | YAT | 20 | 7.97 |
| 2 | GAN | 62 | 7.13 | GAN | 8 | 4.94 | YAT | 43 | 9.43 | UDU | 12 | 4.78 |
| 3 | UDU | 50 | 5.75 | UDA | 7 | 4.32 | UDU | 34 | 7.46 | UDA | 11 | 4.38 |
YAT, Yatinuwara; GAN, Gangawatakorale; UDU, Udunuwara; AMB, Ambagamuwa; KOT, Kothmale; UDA, Udapalatha
More than half (57.19%) of the OPMD patients presented to the Oral Medicine Clinic of the Dental Teaching Hospital, Peradeniya were living within the 20 km buffer zone of the hospital which is the ‘reasonable distance to a specialist care centre’.
Discussion
Sri Lanka is a country with a heavy burden of oral cancer with the large number of cases being reported every day. Diagnostic delay in Oral cancer is recognized as the paramount determinant in morbidity and mortality. The devastating morbidities of oral cancer can be prevented if these cases are identified at an OPMD stage [19].
The finding of the current study illustrates that the highest number of OLP patients were females although OSF and OL were common among males. Further, OL was predominant among people older than 50 years while OSF and OLP were more prevalent in people aged 50 or less. These findings lie in consensus with the results of a clinicopathological audit done by Pieris et al., 2014 on patients who attended the University Dental Hospital, Peradeniya between 2000 and 2014. The study highlights that the mean ages for OL, OLP and OSF to be 57.06, 47.63 and 44.01 respectively [18]. Pieris et al., 2014, further reported OLP/OLL (57.3%) as the commonest OPMD followed by keratosis/hyperkeratosis with or without dysplasia (22.58%) and OSF (20.12%) presented to the University Dental Hospital, Peradeniya [18]. The findings of the current study revealed a similar frequency of presentation with OLP being the commonest, followed by OL and OSF respectively. These findings indicate that there is no significant variation in the patterns of patients presenting over the years.
However, the National Oral Health Survey in Sri Lanka 2015-2016 elicited a contrasting presentation of these values. The report of the national oral health survey is recognized as the standard representation of population oral health status in Sri Lanka. According to the survey, OL (43%) was the most common OPMD in Sri Lanka followed by OSF (32.26%) and OLP (24.73%) [7]. This disparity observed may be due to the differences in referral patterns to the only academic Oral Medicine Unit in Sri Lanka. Most of these cases presented to the institution were referrals from primary or secondary oral health care facilities. Self-referrals were minimal. Therefore, patterns observed in the population is not represented in the current sample.
According to Warnakulasuriya et al., 1984, the prevalence of OPMD in Sri Lanka is calculated as 4.2% [6]. In a similar study, Ariyawardana et al., 2007 reported the prevalence of OPMD among tea estate workers in the Central Province to be 6% [20]. To further support the evidence of the higher prevalence of OPMDs among the estate population, Amarasinghe et al 2018 reported 11.3% among estate workers in Sabaragamuwa province [21]. The tea estate labourers were a well-recognized community for the frequent involvement of risk habits such as betel chewing, smoking and alcohol during their daily routine. To worsen the situation poverty and lack of awareness synergizes their suitability to the high-risk group to develop oral cancer [20]. The Central Province has the highest estate density with the majority being a tea. Surprisingly, the data enumerates that more OPMD patients have been reported from areas with low estate density such as Yatinuwara (7.83%), Udunuwara (5.75%) and Gangawatakorale (7.13%) than areas with high estate density such as Kothmale (3.45%) and Nuwara Eliya (0.92%). This may be due to the fact that most of the estate workers living in a poor socio-economic background, education level and lacks the awareness of OPMDs delay seeking medical advice until the lesions become obvious cancers with symptoms. Further, they may attend hospitals closer to their residence and be referred elsewhere outside the province.
Another important observation of the study was the low frequency of patients presented from the Matale district. Although Kegalle district belongs to the Sabaragamuwa province, more OPMD patients were presented from Kegalle than Matale. This may be partly attributed to the low population density seen in the Matale district compared to the other adjacent districts. Besides A1 highway (one most populated roads in Sri Lanka) spans across Kegalle district towards Kandy district where the University Dental Hospital Peradeniya is also located. More transport options are available to the patients from Kegalle than the patients from Matale.
A study done by Wijewardena et al. in 2018 concluded that about 75% of the population in the Central Province are living within 20 km from a specialized Oral and Maxillofacial Surgery Clinic [17]. The present study has found that 57.19% of the OPMD patients that presented to the Dental Teaching Hospital, Peradeniya were living within a 20 km buffer from the hospital. Approximately 42.81% of patients presented due to a lack of specialized clinics in other regions or can be due to the facilities and availability of specialized staff for diagnosis and managing of oral cancer. This highlights the importance of considering geographical aspects in health resource planning rather than allocating resources on a district or provincial base.
The study embarks upon GIS in oral cancer and OPMD management and is an eye-opener for the novel approaches based on geography in the prevention of oral cancer.
Acknowledgements
Thanks to Mahes Salgado, the Coordinator of the ELTU, Faculty of Medicine, and former head ELTU for editorial assistance.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for- profit sectors.
References
- Oral potentially malignant disorders: Revisited Ray J. J oral Maxillofac Pathol.2017;21(3):326-327. CrossRef
- Oral potentially malignant disorders: risk of progression to malignancy Speight PM, Khurram SA, Kujan O. Oral Surg Oral Med Oral Pathol Oral Radiol [Internet].2018;125(6):612-627. CrossRef
- National Cancer Control Programme Sri Lanka. National Cancer Incidence and Mortality Data Sri Lanka : 2015. 17th ed. Colombo 2021.
- A comparison of health state utility values associated with oral potentially malignant disorders and oral cancer in Sri Lanka assessed using the EQ-5D-3 L and the EORTC-8D Kularatna S, Whitty JA, Johnson NW, Jayasinghe R, Scuffham PA. Health Qual Life Outcomes [Internet].2016;14(1):1-10. CrossRef
- Natural history of potentially malignant oral lesions and conditions: An overview of the literature Napier SS, Speight PM. J Oral Pathol Med.2008;37(1):1-10. CrossRef
- Utilization of primary health care workers for early detection of oral cancer and precancer cases in Sri Lanka Warnakulasuriya KAAS, Ekanayake ANI, Sivayoham S. Bull World Health Organ.1984;62(2):243-250.
- Ministry of Health Nutrition and Indigenous Medicine. National Oral Health Survey Sri Lanka 2015-2016 [Internet]. 2018. 1–134 p Available from: http://www.moh.gov.lk..
- Economic burden of managing oral cancer patients in Sri Lanka: A cross-sectional hospital-based costing study Amarasinghe H, Jayasinghe RD, Dharmagunawardene D, Attygalla M, Scuffham PA, Johnson N, et al . BMJ Open.2019;9(7). CrossRef
- Economic cost of managing patients with oral potentially malignant disorders in Sri Lanka Amarasinghe H, Jayasinghe RD, Dharmagunawardene D, Attygalla M, Kumara DR, Kularatna S, et al . Community Dent Oral Epidemiol.2021;:1-6. CrossRef
- Automated Detection and Classification of Oral Lesions Using Deep Learning for Early Detection of Oral Cancer Welikala RA, Remagnino P, Lim JH, Chan CS, Rajendran S, Kallarakkal TG, et al . IEEE Access.2020;8:132677-132693.
- University Consortium for Geographic Information Science (UCGIS). UCGIS bylaws [Internet]. 2016th ed. Washington, DC; 2016 [cited 2018 Feb 5] Available from: http://www.ucgis.org/assets/docs/ucgis_bylaws_ march2016.pdf..
- Research on the Application of Geographic Information System in Tourism Management. Wei W. Procedia Environ Sci [Internet].2012;12(Icese 2011):1104-1109. CrossRef
- A public health care information system using GIS and GPS: A case study of shiggaon Hanjagi A, Srihari P, Rayamane AS. Lect Notes Geoinf Cartogr.2007;199039:243-255.
- GIScience and cancer: State of the art and trends for cancer surveillance and epidemiology Sahar L, Foster SL, Sherman RL, Henry KA, Goldberg DW, Stinchcomb DG, et al . Cancer.2019;125(15):2544-2560.
- School dental service in Sri Lanka: Geo-spatial analysis of access to oral health care Ranasinghe N, Kruger E, Tennant M. Int J Paediatr Dent.2018;28(5):490-496. CrossRef
- The heterogeneous nature of water well fluoride levels in Sri Lanka: An opportunity to mitigate the dental fluorosis Ranasinghe N, Kruger E, Chandrajith R, Tennant M. Community Dent Oral Epidemiol.2019;47(3):236-242. CrossRef
- The distribution of dental health specialist locations in Sri Lanka Wijewardena B. Community Dental Health.2018;(35). CrossRef
- Clinico-Pathological Audit Of 1904 Oral Potentially Malignant Disorder (OPMD) Patients Who Attended The University Dental Hospital, Peradeniya Peiris PM, Jayasinghe LAH, Wijeratne Y.M.T.Y., Rambukwellle I.W.Y.K.C., Bowala DNK,, Sitheeque M.A.M., Jayasinghe RD. In 2014..
- Screening programmes for the early detection and prevention of oral cancer Brocklehurst P, Kujan O, O’Malley LA. Cochrane Database Syst Rev.2013;2013(11).
- Prevalence of oral cancer and pre-cancer and associated risk factors among tea estate workers in the central Sri Lanka Ariyawardana A, Sitheeque MAM, Ranasinghe AW, Perera I, Tilakaratne WM, Amaratunga EAPD, et al . J Oral Pathol Med.2007;36(10):581-587. CrossRef
- High Prevalence of Lifestyle Factors Attributable for Oral Cancer, and of Oral Potentially Malignant Disorders in Rural Sri Lanka Amarasinghe A A H K, Usgodaararachchi U S, Johnson N W, Warnakulasuriya S. Asian Pacific Journal of Cancer Prevention.2018;19(9). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times