Case Series of Rare Primary Intranasal Diffuse Large B-cell Lymphoma among Filipinos
Download
Abstract
Background: Diffuse Large B-cell Lymphoma (DLBCL) is the most common type of Non-Hodgkin Lymphoma (NHL) at the present time. However, it rarely presents in the intranasal cavity as the primary site. There is scarcity of local data on this disease, and the outcomes to the standard treatment are still unclear.
Objective: In this case series, we presented 2 patients with primary intranasal DLBCL that were treated with chemotherapy ± anti-CD20 antibody and radiotherapy.
Results: Both cases were in the early stage of disease. One patient was given systemic chemotherapy (CHOP) plus anti-CD20 antibody (Rituximab), and the other patient was only given chemotherapy (CHOP) due to financial constraints. The systemic treatment was followed by Involved-Field Radiotherapy (IFRT). Both patients demonstrated with an objective radiologic and clinical response to the treatment. The patients had no evidence of disease recurrence at 36 months.
Conclusion: The cases presented showed that primary intranasal DLBCL appears to have an objective and durable response to the treatment for DLBCL as prescribed by the guidelines. The findings in this study can be added to the pool of data to expand our comprehension of this disease process.
Introduction
Primary nasal Diffuse Large B-Cell Lymphoma (DLBCL) is an extremely rare disease. It is estimated to be at 0.2 to 2% of all cases of Non-Hodgkin Lymphomas (NHLs). Patients with nasal DLBCL were found to be older, predominantly males, present at an early stage of disease, with low incidence of B symptoms and elevation of lactate dehydrogenase (LDH), good performance status, and a low international prognostic index (IPI) score. The clinical behavior and treatment outcomes were determined with the use of a CHOP-based chemotherapy, with or without rituximab, and with or without involved-field radiotherapy (IFRT) which showed an overall response rate (ORR) of 76% in a median follow up of 37 months, and a 3-year progression-free survival (PFS) and overall survival (OS) of 44% and 52.8%, respectively. These outcomes are numerically inferior and conclude a poorer prognosis with a propensity for extranodal failure as compared to the typical DLBCL [1].
Case Series
We present two cases seen in our institution that had similar presenting symptoms. Metastatic work-up for both patients revealed no other sites of disease. Both patients received systemic chemotherapy, however, only one patient was able to receive Rituximab and subsequent radiotherapy due to financial constraints. Nevertheless, clinical benefit was seen in both cases.
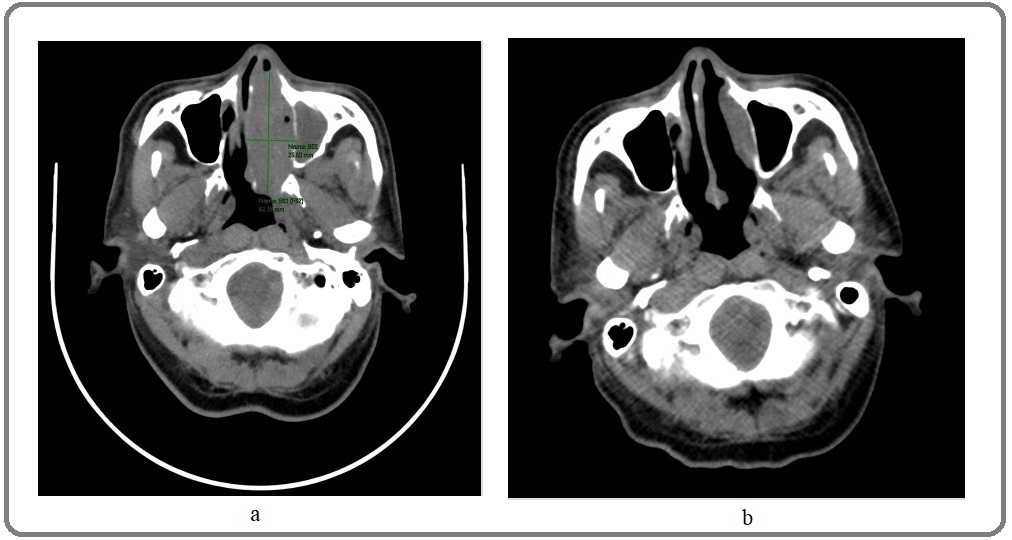
The first case is a 70-year old male who presented with anosmia. The patient experienced a 5-month history of intermittent nasal congestion, rhinorrhea, which subsequently led to anosmia and a nasal voice quality. There were no other signs and symptoms such as fever, chills, loss of appetite, and weight loss. The patient consulted an otolaryngolosist due to persistence of symptoms and an anterior rhinoscopy was done which showed a fleshy mass in the left nasal cavity, with bilateral whitish discharge, and normal findings in the right nasal cavity. A biopsy was done revealing a round cell tumor followed by immunohistochemical stainings (IHC) which turned out to be CD20 positive, P63 focally positive, ki67 >95% (high), and negative for cytokeratin, CD3, S100, chromogranin, and synaptophysin. The histopathologic finding was compatible with the diagnosis of High-grade Non-Hodgkin B-cell lymphoma (NHL) favoring Diffuse Large B-cell Lymphoma. An iodine-contrast computed tomography (CT) scan of the nasopharynx, chest, and whole abdomen and pelvis were done to determine the extent of the disease. The nasopharynx CT showed a heterogeneously enhancing soft tissue mass centered in the left nasal cavity measuring 6.2 x 2.4 x 4.7 cm and extends posteriorly to the choana (Figure 1a).
Figure 1. a, Axial View Nasopharynx CT-Scan (Pre-RCHOP); b, Axial View Nasopharynx CT-Scan (Post-RCHOP).
The chest and abdomen CT were all negative for metastasis.
The final diagnosis was primary sinonasal DLBCL stage I with an IPI score of 1. The patient received 3 cycles of treatment with CHOP and Rituximab (RCHOP21) regimen (Rituximab 375mg/m2 IV day 1, Cyclophosphamide 750mg/m2 day 1 IV, Doxorubicin 50mg/m2 day 1 IV, Vincristine 1.4mg/m2 day 1 IV; maximum of 2mg, and Prednisone 100mg/day PO day 1-5). A post-treatment evaluation with FDG PET/CT with IV contrast (Figure 2) was done which showed a significant regression in size of the intranasal mass to 4.2 x 1.1 x 1.5 cm and no undue FDG uptake (Figure 1b).
Figure 2. Post-RCHOP PET/CT with IV Contrast.
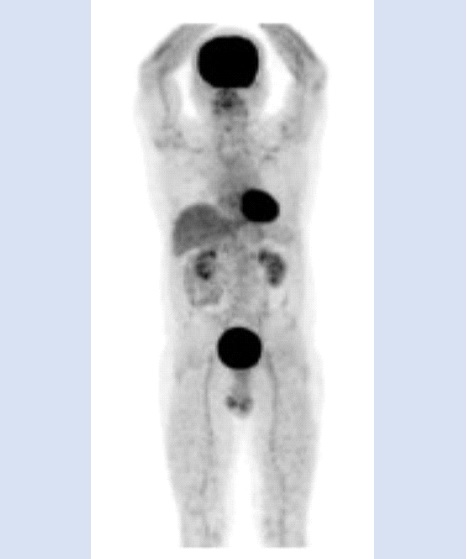
The rest of the findings did not show any hypermetabolic lesion suggestive of active malignant disease. The previous symptoms of anosmia and change of voice quality have markedly improved together with his general performance status, and there were no significant adverse reactions to date. The patient then received involved-field radiotherapy (IFRT) in the left nasal cavity with a total tumor dose of 4,000 cGy in 20 fractions. Three years post-treatment, the patient’s subjective complaints were all resolved and the surveillance imaging did not show any evidence of disease recurrence.
The second case is a 53-year-old female who presented with a 6-month history of colds and nasal congestion and was initially managed with nasal sprays and decongestant. There was a small non-tender fleshy mass measuring approximately 0.5 x 0.5 cm which gradually enlarged causing anosmia. Paranasal CT-Scan showed a mildly enhancing soft tissue mass in the LEFT nasal cavity measuring 2.7 x 1.9 x 5.9 cm (Figure 3).
Figure 3. Axial, Sagittal, Coronal Views Paranasal CT-Scan Pre-treatment (LEFT) and Upon Initial Consult (RIGHT).
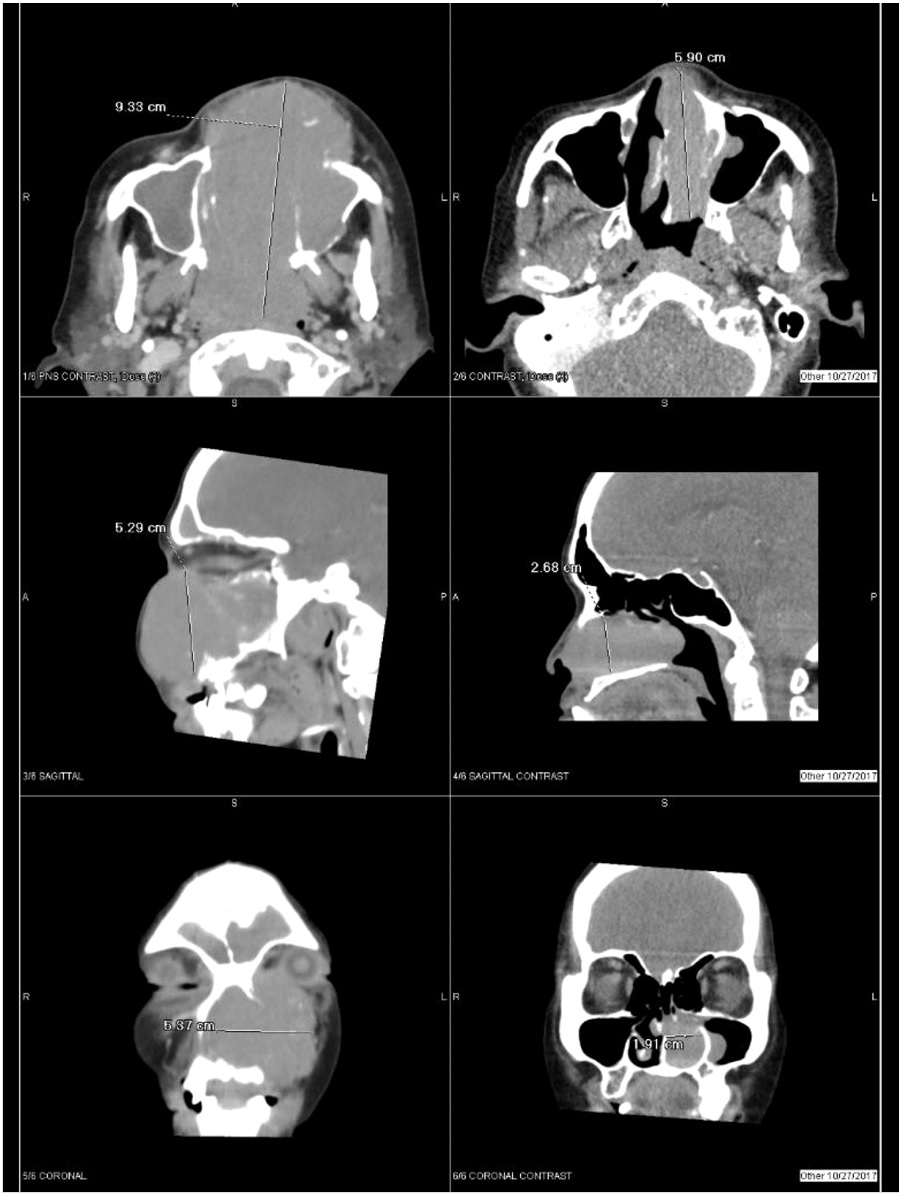
It appeared to fill up the middle and inferior meati and the left osteomeatal unit was obstructed. A rounded soft tissue focus was detected along the medial wall of the left maxillary sinus possible part of the aforementioned left nasal cavity mass. There was left ward bulging of the lateral wall of the left nasal cavity due to the mass. Initial biopsy result showed round cell neoplasm and IHCs done (CD20 positive, CK negative, and CD 3 negative) were consistent with a High grade, B-cell Non-Hodgkin Lymphoma favoring diffuse large B cell lymphoma. She was advised to complete metastatic work-up however was lost to follow up for 5 months. She decided to seek consult when the rapidly enhancing lesion on the left intranasal cavity started to cause facial deformity (Figure 3,4), pain and fullness, headache, increased lacrimation on the left eye, anosmia and nasal congestion. Whole abdominal scan and Chest CT scan showed no other evidence of disease.
Figure 4. Facial Deformity (pre-treatment).

Patient was advised to undergo treatment with RCHOP21 regimen (Rituximab 375mg/m2 IV day 1, Cyclophosphamide 750mg/m2 day 1 IV, Doxorubicin 50mg/m2 day 1 IV, Vincristine 1.4mg/m2 day 1 IV; maximum of 2mg, and Prednisone 100mg/day PO day 1-5). However, the patient was only able to complete 6 cycles of CHOP regimen and was unable to afford Rituximab treatment. To date, the intranasal mass had already resolved (Figure 5), ECOG Performance Score is 0 and quality of life was significantly improved.
Figure 5. Axial View Paranasal CT-Scan (post-treatment).
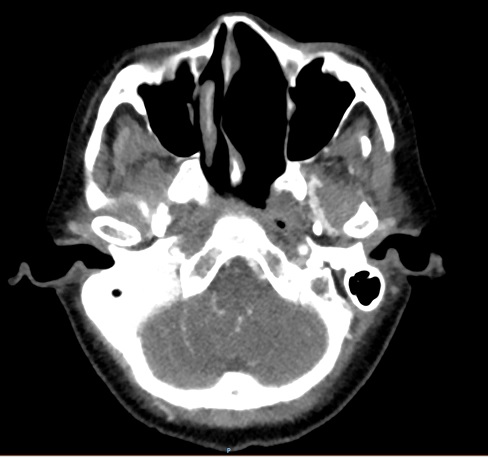
The latest evaluation CT Scan of the neck and paranasal sinuses (1 year post-treatment) showed regression in the degree of mucosal thickening in frontal, maxillary, sphenoid and ethmoid sinuses with minimal residuals in both maxillary and ethmoid sinuses. No discrete enhancing mass lesion seen in the paranasal sinuses and nasal cavity. The chest and whole abdominal CT scans were also negative for active lesions.
Discussion
Diffuse Large B Cell-Lymphoma is the most commonly occurring type of Non-Hodkin Lymphoma [2]. However, this may rarely be found primarily in extranodal sites. Primary nasal lymphoma is a rare disease and the diagnosis may sometimes be delayed due to nonspecific and relatively mild symptoms. Histopathologic examination with immunohistochemical stainings are needed to confirm the diagnosis Primary nasal cavity and paranasal sinus lymphoma demonstrates aggressive behavior and often relapses [3]. However due to the rarity of this disease, treatment has been extrapolated from diffuse large B-cell lymphoma which involved the lymph nodes. Chemotherapy is the primary treatment for nasal DLBCL followed by IFRT [1]. In a study of Yoo-Kang Kwak et al., final local control rate after radiotherapy was 94% [4]. However, another study showed that there is no significant difference in survival between chemotherapy with or without rituximab or chemotherapy plus radiotherapy and chemotherapy alone [1].
The incidence of this disease precludes large-scale studies to ascertain the most appropriate treatment and the prognostic or predictive factors for patients afflicted. These patients would need long term follow up and close monitoring as primary nasal lymphoma is aggressive and has high rates of relapse.
References
- Clinical behavior and treatment outcome of primary nasal diffuse large B-cell lymphoma Nn Lu, Yx Li, Wh Wang, J Jin, Yw Song, Lq Zhou, Sl Wang, Yp Liu, Xf Liu, Zh Yu. Cancer.2012;118(6). CrossRef
- Primary nasal diffuse large B-cell lymphoma with synchronous pulmonary involvement: A case report Hao Shuhong, Sun Yan, Hu Chunmei, Zhi Yunhui, Xiao Han, Li Yarong. Medicine.2019;98(17). CrossRef
- The value of [(18)F]fluorodeoxyglucose positron emission tomography/computed tomography in extranodal natural killer/T-cell lymphoma D Karantanis, Rm Subramaniam, Pj Peller, Vj Lowe, Jm Durski, Da Collins, E Georgiou, Sm Ansell, Ga Wiseman. Clinical lymphoma & myeloma.2008;8(2). CrossRef
- Treatment outcome of diffuse large B-cell lymphoma involving the head and neck: Two-institutional study for the significance of radiotherapy after R-CHOP chemotherapy Yk Kwak, Bo Choi, Sh Kim, Jh Lee, Dg Kang, Jh Lee. Medicine.2017;96(25). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times