Phenotypic Appraisal of Collision Tumors of Thyroid – Initial Experience of a Rare Entity at a Cancer Centre in South India
Download
Abstract
Introduction: Collision tumours (CT) of the thyroid refer to the coexistence of two or more independent, histologically distinct malignant tumours. Though the presence of multifocal differentiated thyroid carcinomas is common, it is extremely rare for the thyroid to harbour more than one type of malignancy simultaneously.
Methods: An extensive literature search of PubMed databases identified very few cases indicating the tumour rarity. To the best of our knowledge, this is the first documentation of a case series including various combinations of CT in the thyroid. Our main aim is to explore the phenotypic characteristics of CT in the thyroid with an aim of revealing unique features associated with this rare entity.
Results: Of a total of 138 thyroid cancers treated during the eight-year period, five (3.62%) were diagnosed as CT. All were females with a median age of 50 years. Papillary Thyroid Carcinoma (PTC) was the major component (80%) in collision with medullary (MC), follicular, and hurthle cell carcinomas. Both cases with papillary microcarcinoma showed vascular emboli and patients with a combination of MC and PTC had nodal metastasis. 80% of patients had a survival of more than 2.5 years and are alive without disease at present. Our study showed features like female predominance and PTC as the most common component with good overall survival. Metastatic and survival rates were consistent with matched singleton pathology.
Conclusion: Insight into the genomic and proteomic pathways of this entity is the need of the hour.
Introduction
Thyroid carcinoma, the most common endocrine malignancy worldwide, accounts for 1–5% of all carcinomas in females and less than 2% in males [1,2]. In the last few decades, thyroid carcinoma incidence has continuously and sharply increased worldwide [1,2]. Thyroid neoplasms are broadly classified as follicular cell differentiated and C cell/ parafollicular cell differentiated. Follicular cell differentiated carcinomas include well differentiated carcinomas like papillary carcinoma and follicular carcinoma, undifferentiated/ anaplastic thyroid carcinoma and poorly differentiated / insular thyroid carcinomas which is intermediate between the two. Medullary thyroid carcinoma is a C cell differentiated neoplasm. Majority of these differentiated thyroid carcinomas are composed of a single cell population.
Our area of interest is the “collision tumor” which is defined as simultaneous occurrence of two distinct neoplasms derived from different cells of origin and is a recognized, albeit rare, entity [3,4]. Collision tumors at any site are histologically distinct and morphologically independent malignant tumors that coexist geographically [5]. Collision tumors of thyroid represent the presence of two intimately associated but histomorphologically different malignant neoplasms in thyroid gland [6]. Although differentiated malignancies of the thyroid with multifocality are no longer considered a rare event, it is extremely uncommon for the gland to harbor more than one histologic type of malignancy at the same time [7]. The usual patterns of this dual pathology include combinations of papillary with medullary carcinoma or papillary with squamous cell carcinoma [5, 6].
We undertook an extensive literature search of the PubMed data bases from 1985- the year collision tumor of thyroid was first described [5]. Till date only 36 cases of collision tumors identified in 30 different publications. All these were case reports and to the best of our knowledge, this is the first documentation of a case series including various combinations of collision tumors in Thyroid gland. In this study we explore the phenotypic characteristics of this rare tumor with an aim of revealing the unique features associated with this entity in our population.
Materials and Methods
This study was based on a retrospective review of all patients with histopathological diagnosis of collision tumors of thyroid gland treated at our centre during the period spanning from Jan 2012 – Dec 2019 (8 years). Demographic and treatment data was obtained from the patients’ medical records archived at the department of Carcinoma Registry. Principal focus during analysis of each patient’s record was placed on- a) clinical presenting symptoms b) investigations c) treatment d) follow up details. Haematoxylin and Eosin stained histopathology slides were analyzed for histomorphological characteristics and aid of Immunohistochemistry (IHC) was sought whenever needed.
Results
Of a total number of 138 thyroid carcinoma cases diagnosed during the study period, five (3.6%) presented as collision tumors. All five patients were females with median age of 48 years (range 40 to 60). None of the patients recalled history of irradiation or contributed to occupational/ family history. The most common presenting complaint was swelling in the midline/ front of neck within a duration ranging from 1 month to 2 years. The patients’ clinical and pathological characteristics are described in Table 1.
| Histological details | CASE 1 | CASE 2 | CASE 3 | CASE 4 | CASE 5 | |||||
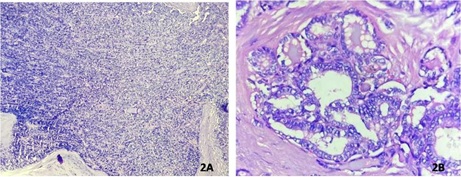
| Histological type | Follicular carcinoma + Papillary microcarcinoma (Image-2a& 2b) | Hurthle cell carcinoma + Follicular variant of papillary carcinoma | Medullary carcinoma + Papillary carcinoma (Image-1a& 1b) | Medullary carcinoma + Papillary microcarcinoma | Follicular carcinoma, widely invasive+ Medullary carcinoma | |||||
| Tumor size (cm) | 3.5x3 | 0.6x0.5 | 5.8x4.9 | 1.8x1.7 | 2.6x2.5 | 1.5x1.1 | 2x2 | 0.5x0.5 | 5.5x4.5 | 2x2 |
| Tumor site | Right lobe- Lower pole | Left lobe- Upper pole | Right lobe- Upper pole | Left lobe- Lower pole | Right lobe- Lower pole | Right lobe- Upper pole | Right lobe- lower pole | Left lobe- Lower pole | Left lobe Lower pole | Left lobe Upper pole |
| Background | Nil | follicular adenoma | Multi Nodular Goitre | Multi Nodular Goitre | Lymphocytic thyroiditis | Nil | Lymphocytic thyroiditis | Nil | Nil | Lymphocytic thyroiditis |
| Predominant pattern | Follicles | Papillary | Trabeculae, nests, sheets | Follicles, papillary | Nest, trabecule, solid | Papillary, follicular | Nest, sheets, islands | Papillary, follicular | Follicles | Nests, sheets |
| Lympho Vascular Emboli | Present | Nil | Present | Nil | Nil | Nil | Present | Nil | Present | Nil |
| Capsular invasion | Present | Nil | Present | nil | Nil | Nil | Nil | Nil | Present | Nil |
| Peri- neural Invasion | Nil | Nil | Nil | Nil | Nil | Nil | Seen in spinal accessory nerve | Nil | Nil | Nil |
| Extra Thyroidal Extension | Nil | Nil | Nil | Nil | Nil | Present | Nil | Nil | Nil | |
| Pathological stage | pT2No | pT1aN 0 | pT2 No | pT1aN0 | pT2N1a | pT1a | pT2 N1b | pT1a | pT3N0 | pT1 N1a |
| Lymph Node involvement | Nil | Nil | 2/8 LN shows metastatic deposits of medullary carcinoma in right level IIA | 11/27 LN shows metastatic deposits of medullary carcinoma in right level II,III | Nil | |||||
| ENE | Nil | Nil | Present | Present | Nil | |||||
| Prognostic stage | Stage I | Stage I | Stage I | Stage I | Stage II | |||||
| Treatment | Total thyroidectomy + Radioiodine Ablation | Total thyroidectomy + Radioiodine Ablation | Total thyroidectomy + Radioiodine Ablation | Total thyroidectomy + Radioiodine Ablation | Total thyroidectomy + Radioiodine Ablation | |||||
| Overall Survival | 34 | 29 | 43 | 46 | 6 | |||||
| (months) | ||||||||||
| Disease Free Survival | 33 | 29 | 40 | 44 | 2 | |||||
| (months) |
Preoperative Fine Needle Aspiration Cytology was done in all cases. Medullary Carcinoma was diagnosed by FNAC in all cases. Two different lesions were diagnosed in two cases in which the lesions were in separate lobes and measured more than 1cm in maximum dimension.
Lesions occurred in separate lobes in 60% cases. No definite predilection for lobe noted. Papillary Carcinoma formed the most common histologic component (n=4) Histological variants included classic type (n=1), follicular variant (n=1) and papillary microcarcinoma (n=2) . Most common observed in our study is Medullary and papillary carcinoma (Figure 1a and 1b) is the most common tumor combination observed (40%). Lymphovascularemboli were present in two cases of follicular carcinoma and one case each of Medullary and Hurthle cell carcinoma. Perineural invasion and ExtraThyroid Extension seen in one case diagnosed as Medullary carcinoma. Nodal metastasis was seen in two cases- both were from Medullary carcinoma with Extranodal extension in one of the cases. All cases had undergone Total thyroidectomy and Radio iodine ablation. At present 80 % cases are alive without disease while one person succumbed to death.
Discussion
The criteria for multiple primary tumors was first established by Bilroth in 1879 and later simplified by Warren and Gates [8,9]. To call an entity as collision tumor, three conditions must be met: (1) each tumor must demonstrate a definite picture of malignancy, (2) each tumor must be distinct, and (3) the possibility that one was a metastatic lesion from the othermust be excluded. While collision tumor refers to coexistence of two or more independent tumors that are histologically distinct, it must be differentiated from mixed and composite tumors of thyroid which show parafollicular and follicular derived cellular elements. Mixed tumor is a single tumor with a common cell of origin, i.e.; tumor cells show expression of both thyroglobulin and calcitonin. Composite tumor on the other hand is a single tumor, with two discrete cellular populations – thyroglobulin positive and calcitonin positive [7,10].
Several hypotheses have been suggested as mechanisms for collision tumors. The simplest is that the two primary tumors occurred in continuity by a chance/ accidental ‘‘meeting.’’ Two different tumors may develop contiguously because the region is altered by the same carcinogenic stimuli. Another hypothesis is that of “neoplastic coercion” the presence of the first tumor alters the microenvironment, making the development of the second adjacent tumor more likely. The third theory “pluripotent precursor cell” theory put forward by Lax et al proposed that they arise from a single pluripotent precursor cell suggests a common stem cell of origin for the two tumors [7][11-13].
Our case series showed the presence of papillary thyroid carcinoma in majority of cases in collision with Medullary (n=2; Figure 1) following by Follicular cell (n=1; Figure 2), and Hurthle cell carcinomas (n=1).
Figure 1. Collision Tumor of Thyroid with a) Medullary Carcinoma b) Papillary Carcinoma. Haematoxylin and Eosin stain. 40 x magnifications.
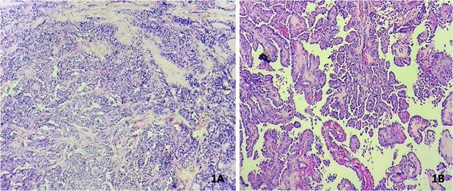
Figure 2. Collision Tumor of Thyroid with a) Follicular Carcinoma b) Papillary Microcarcinoma. Haematoxylin and Eosin stain. 40 x magnifications.
A single case of medullary carcinoma with follicular carcinoma was also present. Literature review suggests that, most common collision tumors of the thyroid are that of medullary and papillary carcinomas which was true in our case. These are also the most common singleton tumors of the thyroid. The next most common combination as per literature review was Squamous cell carcinoma (SCC) and papillary carcinomas, all of which had metastasized at presentation [6]. But none of our cases had SCC. A population-based study has placed the incidence of differentiated thyroid carcinoma and medullary carcinoma coexistence at 12.3% of all medullary carcinomas. This coincidence was found to be increasing in collision tumors [14].
Specific case reports have alluded to risk factors for the development of collision tumors of the thyroid. Darwish et al suggests that lymphocytic infiltration, present in some forms of thyroiditis, may predispose a patient to the condition [15]. This was quite acceptable because three (60%) of our cases had a lymphocytic thyroiditis background. Furthermore, in the case of medullary and papillary collision, the risk is thought to be increased by multiple endocrine neoplastic syndromes. Ultimately, there is simply not enough data, evidence, or understanding to support or exclude any one hypothesis [15,16].
When compared to similar studies, we could understand those collision tumors are more common in females at an age range of 28-84, with an increasing incidence during middle age. This goes in concordance with our study.
Another striking feature is the absence of known risk factors associated with the neoplasms. None of the patients had an exposure to ionizing radiation, familial history or iodine insufficiency. In our study, both cases with papillary microcarcinoma showed LymphoVascular Invasion and patients with a combination of medullary and papillary carcinoma showed lymph node metastasis with extranodal extension. Yet, none of these cases showed recurrence. Only case that showed recurrence was a widely invasive follicular carcinoma with medullary carcinoma and unfortunately that was the only patient who succumbed to death emphasizing the significance of angioinvasion.
On literature review, little information about the survival details are found, owing to rarity of the disease, It is seen that half of the collision tumors did not mention the survival, another half were alive at the time of study and only very few patients died. This highlights the fact that even though collision tumors behave more aggressively than singleton tumors, looking at the body of information, we find that metastatic and survival rates are consistent with matched singleton pathology and no unusual difference in the prognosis of patient was appreciated [17]. We could not find any case reports of collision tumors mentioning the survival outcome.
The treatment of collision tumors poses a unique challenge. As practiced across all oncology, treatment should be developed in a multidisciplinary framework with a patient centered approach. Intrinsically, the most aggressive singleton tumor identified should inform treatment. In the vast majority of cases found in the literature, the authors adopted multimodal treatment with surgery and adjuvant therapy, which was how themultidisciplinary board meeting of our tertiary carcinoma centre also decided to take forward with all the cases [18].
In conclusion, collision tumors of the thyroid are extremely rare. They present both a diagnostic and treatment challenge. There has been limited research into their etiology and patient management. Here, we present a series of this rare entity and would like to ponder upon the genetic and proteomic pathways associated with.
Acknowledgements
The authors acknowledge Dr Sajith Babu, Consultant Head and Neck Surgeon Multispeciality Hospital, MIMS Kannur for valuable insights.
References
- Carcinoma Incidence in Five Continents. IX Curado MP, Edwards B, Shin HR, Storm H, Ferlay J, Heanue M, Boyle P. IARC Scientific Publications.2007;160.
- International patterns and trends in thyroid cancer incidence, 1973-2002 Ba Kilfoy, T Zheng, Tr Holford, X Han, Mh Ward, A Sjodin, Y Zhang, Y Bai, C Zhu, Gl Guo, N Rothman, Y Zhang. Cancer causes & control : CCC.2009;20(5). CrossRef
- Carcinoma of the Thyroid With a Mixed Medullary, Papillary, Follicular, and Undifferentiated Pattern Parker Lawrence N., Kollin Jozef, Wu Sing-Yung, Rypins Eric B., Juler George L.. Archives of Internal Medicine.1985;145(8). CrossRef
- A rare case of collision tumor of thyroid gland: simultaneous occurrence of calcitonin negative medullary thyroid carcinoma and papillary thyroid carcinoma Saharan Savita, Solanki Ranjana, Saharan Deepak. International Journal of Otorhinolaryngology and Head and Neck Surgery.2019;5(6). CrossRef
- Collision tumors of the thyroid: Review of literature and report of a case of papillary–Follicular collision tumor Thomas Vijy Paul, George Rahul. Thyroid Research and Practice.2018;15(2). CrossRef
- Collision tumor of the thyroid gland: primary squamous cell and papillary thyroid carcinoma M Warman, N Lipschitz, S Ikher, D Halperin. ISRN otolaryngology.2011;2011. CrossRef
- Combined tall cell carcinoma and Hürthle cell carcinoma (collision tumor) of the thyroid Baloch Z. W., Mandel S., LiVolsi V. A.. Archives of Pathology & Laboratory Medicine.2001;125(4). CrossRef
- Collision tumor of the thyroid: a case report of metastatic liposarcoma plus papillary thyroid carcinoma M Brandwein-Gensler, M Urken, B Wang. Head & neck.2004;26(7). CrossRef
- Multiple primary malignant tumors Warren S, Gates O. Am J Carcinoma.1932;16:1358-1414.
- Collision tumor of the thyroid: follicular variant of papillary carcinoma and squamous carcinoma Rr Walvekar, Sv Kane, Ak D'Cruz. World journal of surgical oncology.2006;4. CrossRef
- Combined "Mixed Medullary-Follicular" and "Papillary" Carcinoma of the Thyroid with Lymph Node Metastasis Shimizu Michio, Hirokawa Mitsuyoshi, LiVolsi Virginia A., Mizukami Yuji, Harada Tanekazu, Itoh Tomoo, Manabe Toshiaki. Endocrine Pathology.2000;11(4). CrossRef
- Concurrent medullary and papillary carcinomas of thyroid with lymph node metastases. A collision phenomenon Pastolero G. C., Coire C. I., Asa S. L.. The American Journal of Surgical Pathology.1996;20(2). CrossRef
- Mixed medullary-follicular carcinoma and papillary carcinoma of the same thyroid Wu C. J., Chen H. L., Song Y. M., Sheu W. H., Chen S. H.. Internal Medicine (Tokyo, Japan).1998;37(11). CrossRef
- Simultaneous medullary and differentiated thyroid cancer: a population-level analysis of an increasingly common entity Wong Risa L., Kazaure Hadiza S., Roman Sanziana A., Sosa Julie A.. Annals of Surgical Oncology.2012;19(8). CrossRef
- Simultaneous medullary carcinoma, occult papillary carcinoma and lymphocytic thyroiditis Darwish A, Satir AA, Hameed T, Malik S, Aqel N. Malays J Pathol.1995;17(2):103-7. PubMed
- Simultaneous Occurrence of Medullary Carcinoma and Papillary Microcarcinoma of Thyroid in a Patient with Men 2A Syndrome. Report of a Case Giacomelli Laura, Guerriero Gabriella, Falvo Laura, Altomare Vittorio, Chiesa Carlo, Ferri Simone, Stio Francesco. Tumori Journal.2007;93(1). CrossRef
- Collision tumors of the thyroid: A case report and review of the literature Ryan Neil, Walkden Graham, Lazic Darko, Tierney Paul. Head & Neck.2015;37(10). CrossRef
- Concurrent occurrence of medullary thyroid carcinoma and papillary thyroid carcinoma in the same thyroid should be considered as coincidental Wg Kim, G Gong, Ey Kim, Ty Kim, Sj Hong, Wb Kim, Yk Shong. Clinical endocrinology.2010;72(2). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times