Incidence of Microsatellite Instability, Mutational Burden, and Actionable Alterations in Genes of Patients with Metastatic Colorectal Carcinoma: A Study from a Tertiary Care Hospital in India
Download
Abstract
Background and objective: Tumor mutational burden (TMB) and microsatellite instability (MSI) are predictive clinical markers of responses to immunotherapy in a wide range of advanced cancers, including colorectal cancers. The data about TMB and MSI in Indian patients is scarce. Hence, assessed the incidence of MSI, TMB, and actionable alterations in genes of patients with metastatic colorectal carcinoma.
Methods: A single centre, observational, prospective study in newly diagnosed patients (n=60) with colorectal carcinoma were assessed for MSI incidence, mutational burden, and actionable alterations in genes.
Results: The TMB ranged between 5.08 and 2391 mutations per megabase, and 12 (20%) had low TMB, 12 (20%) intermediate TMB and 36 (60%) high TMB. The TMB was high in right-sided than left-sided cancer (100% vs. 47%). Three or more two, and one genomic alteration were observed in 26 (44%), 20 (33%), and (20%) patients, respectively. Gene fusion was absent in all 60 patients. Gene mutations were predominant in the left-sided than right-sided but statistically insignificant (p=0.7). APC, TP53, and BRCA2 gene mutations were evident in 46, 28, and 22 patients, respectively. Wild KRAS/NRAS gene alterations were evident in all metastatic cancers (n=22) presented at baseline. There was no significant correlation between the genomic alterations and age, sex, histology, or tumor differentiation.
Conclusion: This study highlights the importance of detecting genomic mutations at the earliest. Genomic mutations should form the basis for customizing and exploring newer targeted therapy against the most common genomic alteration like APC, TP53, and RAS mutations to improve outcomes.
Introduction
Colorectal cancer is a fatal disease with an insidious onset. When the disease is clinically apparent, most of the cases are beyond cure. Despite advances in surveillance as well as imaging modalities, most cancers exasperate attempts at early detection. Thus, treatment is often late, and the survival is dismal.
Globally, colorectal cancer was the third most common malignancy (after lung and breast) and the second most common cause of cancer death (after lung) in 2020 [1]. Colorectal cancer is one of India’s most rapidly increasing cancers, and the westernization of the lifestyle is the important attributable factor [2]. Age-adjusted incidence rates of colorectal cancer from Population-Based Cancer Registries under the National Cancer Registry Programme, India was 2%–19.9% in men and 1.7%–11.4% in women [3]. According to a recently presented data at the American Society of Clinical Oncology (ASCO), the incidence of colorectal cancer in India has increased by 20.6%, between 2004 and 2014, from 5.8% (in 2004-2005) to 6.9% (2012-2014) [2].
Colorectal cancer is one of the three most common gastrointestinal cancers [4]. Hence, it is important to develop effective means to counter this disease. Advances are being made in the early detection followed by multimodality treatment with a combination of radiotherapy, chemotherapy, and surgery to provide better care to patients with colorectal cancer. However, the prognosis is good in the early stages of the disease. Most cases of colorectal cancer in India are detected in the advanced and metastatic stages where the only modality of treatment is palliative chemotherapy. Moreover, the prognosis in such patients remains poor, and the mortality rate is high, specifically in the young Indian population where the disease is aggressive and metastatic at presentation.
Chemotherapy over the past two decades has been an unsatisfactory option for advanced colorectal cancers. This has been due to a lack of knowledge of various biomarkers and driver mutations that aggravate the disease. Several biomarkers and mutations have been identified as important targets for therapeutics. In recent times, the role of mutations in the RAS and the downstream RAF pathways have been identified and effectively targeted with anti-epidermal growth factor receptor (EGFR) and anti-vascular endothelial growth factor receptor (VEGF) agents along with conventional chemotherapy. Nevertheless, several mutations originating from an adenoma to carcinoma are undiscovered in colorectal cancer and have a strong genetic preponderance. Tumor Mutational Burden (TMB), quantifies the mutations per deoxyribonucleic acid (DNA) me abases (Mut/Mb) in tumor cells, has evolved as a new predictive clinical marker of immunotherapy in a wide range of advanced including colorectal cancers [5,6]. Microsatellite instability (MSI) is a consequence of DNA mismatch repair (MMR) deficiency [7,8]. Microsatellite instability is one of the possible predictive markers in metastatic tumors, including colorectal cancer [8,9]. TMB and MSI may also influence the response of tumors to new agents like immune checkpoint inhibitors [5,10].
The data about TMB and MSI in Indian patients is scarce; hence, we studied the TMB in various stages of colorectal cancer and correlated it with the disease profile. We also assessed the occurrence of various mutations in colon cancers, which could serve as important targets for future treatment. The incidence of DNA MMR and MSI which is the cornerstone of immunotherapy was studied.
Study objectives
To assess the incidence of MSI, mutational burden, and actionable alterations in genes of patients with metastatic colorectal carcinoma.
Materials and Methods
We conducted a single centre, observational, prospective study at the Department of Oncology, Malignant Diseases Treatment Centre (MDTC), Command Hospital Bangalore. The MDTC brings together the expertise within the hospital and provides comprehensive and coordinated cancer care along with departments of Medical Oncology, Surgical Oncology, Radiation Oncology, and Oncopathology. The MDTC centre caters to serving defence personnel and their families from all three arms of services (Army, Navy, and Air force) throughout the country.
Study population
Sixty newly diagnosed patients with metastatic colorectal carcinoma were assessed for MSI incidence, mutational burden, and actionable alterations in genes. All patients with metastatic colorectal cancer whose paraffin embedded blocks were available during the two-years of study were included. Patients with histopathological evidence of inadequate tumor, early colorectal cancer, and non-metastatic disease were excluded from the study.
Sample size
For sample size calculation, we assumed a minimum of 80% power and a 5% significance level (significant at 95% confidence level). If the true relative risk of failure for experimental subjects is 0.16, it is estimated that at least 30 experimental subjects are needed. The Type I error probability associated with the test is 0.05 (Formula 1).
Formula 1.
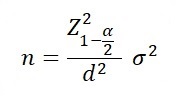
α = 5% (i.e. Confidence level = 95%)
d = 5%
Standard deviation (σ)
Precision required =d
Probability of type I error
Data collection techniques and tools
Formalin-fixed and paraffin embedded samples obtained from biopsy specimens of patients with advanced/ metastatic colorectal carcinoma was evaluated for MSI, TMB, and actionable alterations in genes. The genetic alterations were evaluated using Next-generation sequencing (NGS). Comprehensive genomic profiling was done using NGS to identify all 4 types of genomic alterations (namely insertion/deletions, base substitutions, copy number alterations and rearrangements) across all genes known to be drivers of solid tumors. Simultaneous sequencing of the coding region of 315 cancer-related genes plus introns from 28 genes often rearranged or altered in cancer using NGS technique was also performed. The epidemiological and clinicopathological profile of the disease was correlated with the TMB, MSI status, and other detected mutations to study any trend.
A low TMB was defined as <5 Mut/Mb, intermediate TMB as 5 to<20 Mut/Mb, high TMB as 20 to <50 Mut/ Mb and very high TMB as >50 Mut/Mb. The scoring and classification of high, intermediate, and low TMB were based on in-house validation, supported by a clinical study on colorectal cancer patients assessed for TMB score and its correlation with response to immune checkpoint inhibitors.
Results
Baseline demography
From July 2018 to July 2020 (2 years), 60 patients with advanced /metastatic colorectal cancer, who met the inclusion criteria, were prospectively enrolled in the study. There were 34 males and 26 females in the study (M: F=1.3:1).
The mean age of the enrolled patients was 59.68 years (45–74 years). Most patients were in the age group of 51–60 years. All patients at the time of enrolment presented with altered bowel habits (100%), associated with weight loss (50%) and bleeding per rectum (75%). Anemia was seen in 30%. Five patients presented with obstruction at presentation, and 3 (10%) presented with tenesmus.
The most common location of the tumor was in the left-side of the colon (distal 1/3 of the transverse colon to the anorectum; n=42 [70%]). Among them, 22 were in the sigmoid colon, 16 in the rectum and six in the transverse colon near the splenic flexure. Eighteen (30%) patients had right-sided colon cancer (ileocecal junction to proximal 2/3 of the transverse colon). The common subsite was caecum (n=8) and ascending colon (n=8). Anemia and weight loss with altered bowel habits were common in right-sided lesions, while bleeding per rectum and altered bowel habits were common in the left-sided lesions.
Among 60 patients, 56 (93%) patients had adenocarcinoma histology, while one each had mucinous and signet cell carcinoma. After clinical, pathological, and radiological staging with contrast-enhanced (CECT)/ positron emission tomography (PET)-CT scan, 20 (33%) patients had stage II, 18 (30%) stage III, and 22(37%) patients were metastatic at presentation. During treatment or follow-up, 10 patients in stage II and 12 patients in stage III metastasized (Table 1).
| Variable | Sub Variables | N = 60 | % |
| Sex | Male | 34 | 57 |
| Female | 26 | 43 | |
| Age | <51 years | 6 | 10 |
| 51–60 years | 34 | 57 | |
| 61–70 years | 12 | 20 | |
| 71–80 years | 6 | 10 | |
| >80 years | 2 | 3 | |
| Side of colon | Right side | 18 | 30 |
| Left side | 42 | 70 | |
| Colon subsite involved | Caecum | 8 | 13 |
| Ascending colon | 10 | 17 | |
| Transverse colon | 4 | 7 | |
| Descending colon | 2 | 3 | |
| Sigmoid colon | 22 | 33 | |
| Rectum | 14 | 23 | |
| Stage | II | 18 | 30 |
| III | 20 | 33 | |
| IV | 22 | 37 | |
| Histology | Adenocarcinoma | 56 | 93 |
| Others | 4 | 7 | |
| Tumor differentiation | Moderately differentiated | 42 | 70 |
| Well-differentiated | 6 | 10 | |
| Poorly differentiated | 12 | 20 |
Tumour mutation burden profile
The TMB in 60 samples ranged between 5.08 and 2391 Mut/Mb, and 12 (20%) had low TMB, 12 (20%) intermediate TMB, while 36 (60%) high TMB. All samples (n=12) with low TMB were found in the sigmoid colon (left-sided), while all 12 samples with intermediate TMB were found in the rectum (range 5.92 to 8.93 Mut/Mb). Twenty (47%) samples of left-sided colon cancers had a high TMB with a maximum number in the descending colon and rectosigmoid (max 2391 Mut/ Mb). All samples [18 (100%) of right-sided colon cancers (caecum, ascending colon, and proximal transverse colon) had high TMB in the range of 33.96–2044 Mut/ Mb (p<0.01).
The TMB profile is presented in Table 2.
| Tumor mutation burden (TMB) | |||
| Variable | Low TMB | Intermediate TMB | High TMB |
| Number | 12 (20%) | 12 (20%) | 36 (60%) |
| Left-sided | 12 | 12 | 18 |
| Transverse colon | 0 | 0 | 4 |
| Sigmoid colon | 0 | 12 | 10 |
| Rectum | 12 | 0 | 4 |
| Right-sided | 0 | 0 | 18 |
| Caecum | 0 | 0 | 10 |
| Ascending Colon | 0 | 0 | 8 |
| Females | 6 | 6 | 14 |
| Males | 6 | 6 | 22 |
Tumor mutation burden was maximum in the caecum, specifically in the presence of BRAF mutation. Liver, abdominal and lymph node metastasis was common in our patients. Tumor mutation burden was significantly high (p<0.01) in all patients with liver metastasis stage IV disease, with all patients having a TMB above 2000 Mut/Mb. Tumor mutation burden (50 Mut/Mb) was intermediate in patients with abdominal and lymph node metastasis. The TMB was significantly higher in men than in women. Fourteen of the 26 (53%) samples from women had high TMB, whereas 22 out of 34 (64.7%) had high TMB. Tumor mutation burden was higher in women aged less than 60 years and in men aged 60 years and above (p<0.01), specifically in left-sided tumors. There was no other significant correlation between TMB and early-stage histology, or tumor differentiation.
Genomic alteration (mutation) profile
Overall genomic alteration profile of the patients is shown in Table 3.
| Variables | Subset | Total (n=60) | Percent % |
| Number of genomic alterations | 3 or more | 26 | 44 |
| 2 | 20 | 33 | |
| 1 | 12 | 30 | |
| Nil | 2 | 3 | |
| Genomic alteration (mutations) | APC | 46 | 77 |
| TP53 | 28 | 47 | |
| BRCA 2 | 22 | 37 | |
| ERBB 2 | 6 | 10 | |
| BRAF | 4 | 7 | |
| PIK3CA | 4 | 7 | |
| CTNNB1 | 4 | 7 | |
| MET | 2 | 3 | |
| KRAS | 10 | 17 | |
| NRAS | 4 | 7 | |
| Her2nu | 6 | 10 | |
| Gene Fusion | NIL | NIL | Nil |
The mutation analysis revealed that 26 patients (44%) had three or more genomic alterations while 20 patients (33%) had two genomic alterations and 12 (20%) had one alteration. Gene fusion was absent in all 60 patients. APC gene was observed in 46 patients, TP53 in 28 patients, and BRCA2 in 22 patients. These mutations were more common in the left-sided than right- sided but not statistically significant (p=0.7). Among other genomic alterations, ERBB2 and BRAF were seen in six and four patients with right-sided colon cancer, respectively, whereas PIK3A was exclusively observed in four left-sided lesions, all statistically significant (p<0.01). CTNNB1 mutation was evident in transverse colon disease in four patients. The KRAS and NRAS genomic alteration were present in ten and four patients with a nonmetastatic right-sided lesion, respectively (p<0.01). Upfront, all 22 metastatic patients had wild KRAS/NRAS irrespective of the site. MET mutation was seen in two patients. Apart from RAS and PIK3CA oncogenes, the rest were Tumor Suppressor Genes (TSG). There was no significant correlation between the genomic alterations and age, sex, histology, or tumor differentiation.
Mismatch repair status profile
Mismatch repair status and distribution in the study population are depicted in Tables 4 and 5.
| Variables | Subset | Total (n=60) | Percent |
| MMR (MSI) | Proficient (MSI low / stable) | 32 | 53 |
| Deficient (MSI High) | 28 | 47 | |
| MMR deficient (n=14) | Left-sided (n =42) | 14 | 30 |
| Right-sided (n=18) | 14 | 77 | |
| Non-metastatic (n=38) | 22 | 57 | |
| Metastatic (n=22) | 6 | 27 |
MMR, mismatch repair; MSI, microsatellite instability.
| Subset | Left side (n=42) | Right side (n=18) | |
| MSI | MLH1 | 8 | 8 |
| MSH2 | 2 | 6 | |
| MSH6 | 2 | 6 | |
| PMS2 | 10 | 8 |
MSI, microsatellite instability.
The MSI assessment, including MLH1, MSH2, MSH6, and PMS2 revealed that 32 patients (53%) were MMR proficient while 28 (47%) patients were MMR deficient. The MMR deficient tumor was evident in 14 patients, each of right- sided (77%) and left-sided CRC (30%), and this was statistically significant (p<0.01). The MSH2 and PMS2 was predominantly observed in the right-sided lesion (3:1). Eighty percent of MMR deficiency was significantly seen in patients above 60 years, (p<0.01). Mismatch repair-deficient tumors were predominantly nonmetastatic (n=22), 12 were stage II and 10 were stage III, whereas six had metastatic disease. No other statistically significant correlation was seen with histology or differentiation.
Several variants of uncertain significance (VUS) detected in the study population were DBR2, STK11, MRE11A, CARD11, CHEK2, AKT1, SLX4, RET, PALB2, SMO, PMS2, RB1, FGFR4, ROS1, ATR, MRE11A and FBXW7.
Discussion
In our study, colorectal cancer was widely prevalent in men. The average age of patients was 57.8 years. The most common type of colorectal cancer was left-sided (70%). In a large retrospective study (n=800) conducted in Tata Memorial Hospital, Mumbai, the average age of patients was 47.2 years (range 11 years–85 years), and the cancer was predominantly seen in men (65%) [11]. Similar to our study, left-sided tumor (80.2%) was predominant in the large retrospective study. In our study, sigmoid (33%) was the predominant sight of cancer followed by rectum (22%), whereas in the retrospective study, rectum (42%) was the common primary site of the tumor followed by rectosigmoid (21%) [11]. The tumor pathology found in our study was similar to that reported in the large retrospective study, with most of the cancer being moderately differentiated followed by well-differentiated and poorly differentiated cancer pathology.
In our study, nearly two-thirds of the patients had metastatic cancer at the time of enrolment, and nearly one-third each had stage I and II disease. Cancer metastasized in more than 50% of the patients with stage II and III cancer. The left-sided lesion presented early with obstruction, altered bowel habits, and bleeding per rectum, specifically if the subsite is the rectum. The right-sided lesion usually presents late with advanced diseases, like anemia or peritoneal/liver metastasis [12].
Right-sided and left-sided cancer are diverse clinical presentations largely due to variances in tumorigenesis and progression [13-15]. Unlike the west, the disease occurs earlier in Indians regarding age, is more aggressive and the response to treatment is poor. Therefore, the biology of the disease is more likely to be different, and like all cancers, it is critical to understand the various mutations that drive the disease [16]. With the use of immunotherapy as a potent tool in various cancers it has become critical to understand the TMB, MSI and other mutations, which serve as prognostic markers to use immunotherapy effectively.
The TMB is emerging as a quantitative biomarker for predicting the sensitiveness of checkpoint inhibitors in different tumor types. Tumors with higher levels of TMB might also express neoantigens, which can generate a strong antitumor immune response and thereby improve the response to immunotherapy [17,18]. Mutation frequency can be accurately analysed on tumor tissue samples by next-generation sequencing (NGS) [19,20]. Comprehensive panel-based genomic profiling is available instead of whole-exome sequencing for accurately measuring TMB [21-23]. Clinical evidence suggests the potential benefits of TMB as a diagnostic marker in terms of accuracy, sensitivity, and reproducibility [24,25]. Most importantly, quantitative assessment of TMB helps in treatment decisions [5,26]. As clinical evidence has shown that tumors with higher TMB might respond better to checkpoint inhibitors, it is critical to identify these patients and optimize therapy with novel agents.
In our study, NGS platform-based multi-gene analysis and sequences identified variants associated with multiple genes with diagnostic, prognostic, and therapeutic implications in colorectal cancer types. The NGS tumor somatic panel can investigate and screen somatic mutations in 170 cancer-related genes for tumorigenesis, prognostication and predictive value for chemotherapy, and targeted therapy drugs in different tumor types [27-29].
In our study, a higher proportion of patients had a high-TMB (60%). Tumor mutational burden in most of our patients was high (80 to 3000Mut/MB), symbolizing that the mutation in colorectal cancer is aggressive in Indian. Jiao et al. confirmed that TMB varies among different ethnic populations, specifically the Chinese and Caucasian populations and that the TMB-associated mechanism varies between different cancers [30]. Hence, a poor response to chemotherapy and early relapses could be related to the TMB profile. In our study, the TMB was high in all patients with right-sided cancer, whereas TMB was high in 47% of left-sided tumors. Further, TMB was the highest in the proximal colon with the maximum burden in the caecum followed by the ascending colon and descending colon. The TMB decreased distally as the majority of the sigmoid /rectal tumors had low/intermediate tumor burden. Left-sided cancer is less immunogenic, whereas righted-sided cancer is highly immunogenic, and hence right-sided tumor respond to immunotherapies [12]. This explains the phenomena that the left-sided tumors are relatively less aggressive, more responsive to therapy and do not relapse as compared to the right-sided lesion [12]. Moreover, a mutated BRAF commonly seen in the right-sided tumor is a poor prognostic marker and requires a specific target agent [31,32].
In our study, TMB showed gender- and age-related differences. The TMB was significantly higher in men than in women. In our study, colorectal cancer was prevalent at a younger age in women, and 54% of them had a high TMB. Tumor mutation burden was high in women aged less than 60 years, whereas it was high in men aged more than 60 years. This gender difference in the occurrence of colorectal cancer could be attributed to the hormonal differences, presence of a genetic modifier, or an X-linked gene which may have a protective effect against developing colorectal cancer [33,34]. Further evidence is substantiated by the presence of the mutated genes (VUS), like STK11, CHEK2, AKT1, PALB2 and BRCA, in the breast cancer and colorectal [35]. We also found mutated genes STK11, CHEK2, AKT1, PALB2, and BRCA in our samples of colorectal cancer. However, this is an area for further research and therapeutics.
We did not find any other significant correlation between TMB and early stage of disease, histology or tumor differentiation. We also did not find any significant correlation between the genomic alterations and age, sex, histology or tumor.
Liver metastasis was associated with a very high TMB (> 2000 Mut/Mb) compared to abdominal or lymph node metastasis in our study. Although TMB burden is predictive of immunotherapy response [36], there is a lack of data correlating TMB and liver metastasis. Hence, early or nonmetastatic CRC should be closely monitored for liver metastasis if TMB is high.
In our study, the genomic mutations of three or more were evident in a higher proportion of patients (44%). Two and one genomic mutations were seen in 33% and 20% of patients, respectively. Gene mutations were predominant in the left-sided than right-sided but statistically insignificant (p=0.7). Further, among the genomic alteration, the commonest was the APC gene seen in 23 patients, followed by TP53 in 14 patients and BRCA2 in 11 patients. Wild KRAS/NRAS gene alterations were evident in all metastatic cancers.
Knowing specific mutations would enable physicians to customize the available therapies. According to the adenoma-carcinoma hypothesis, APC is the earliest in the sequence of mutations that occurs in tumorigenesis of colorectal cancer [37]. The TP53 gene encodes the p53 protein, also known as a guardian of the genome, plays a critical role in supporting DNA repair. In several cancers, the p53 pathway is inhibited [38]. Anti-EGFR therapies have been promising in treating colorectal cancer with mutations in TSG (APC, TP53, KRAS, and BRAF [39]. BRCA2 was more common than BRCA1 in our study, and hence patients may respond well to platinum therapy. The use of poly(ADP-ribose) polymerase (PARP), inhibitors (synthetic lethality approach) is also being investigated in several cancers, including colorectal cancer [40]. We detected BRAF mutation in the right-sided colon and PIK3CA mutation left-sided colon cancer in few patients. Novel agents like dabrafenib/ trametinib and alpliseb are used in melanoma and breast cancer respectively [41-44]. These agents might be the options that can be explored in patients with BRAF and PIK3CA mutations; however, these drugs are not yet approved in colorectal cancer. ERBB 2 or Her2nu mutation was detected in six patients, all of whom were left-sided. Her2nu targeted therapy along with chemotherapy is an approved option in metastatic colorectal cancer [45]. RAS mutation was seen in the right-sided lesion, and therefore, the cancer was more aggressive than left-sided lesions where RAS was wild. This type would respond to anti- EGFR and chemotherapy.
Mutational heterogeneity is linked to tumor immunogenicity as mutations can augment neoantigen burden, which is also critical for better response to immunotherapy [46]. Tumors such as malignant melanoma having significant somatic mutations have had a positive responses to immune checkpoint inhibitors [46]. The efficacy of various immunotherapy was assessed in patients with high MSI-H/MMR deficiency colorectal cancer were in the KEYNOTE-177, -158, -028, -016, and KEYNOTE-164 (pembrolizumab); NICHE and Checkmate 142 (Nivolumab ± Ipilimumab); GARNET (Dostarlimab) [47-56]. The results from these data have been promising and suggests a strong association between MSI status and immunogenicity in colorectal cancer, as MSI could be linked to improved prognosis compared to microsatellite-stable cancer. In our study, there was no significant difference in the prevalence of tumor MMR proficiency and deficiency (53% vs. 47%). MSH2 and PMS2 were predominantly seen in the right-sided lesion. These tumors were invariably associated with a high TMB in our study. These tumors are likely to respond to immunotherapy agents due to increased tumor-infiltrating lymphocytes, T cell, and TMB [57]. The role of immunotherapy is established in metastatic CRC but not in nonmetastatic disease thirty-seven percent of nonmetastatic CRC (stage II and III) in our study had high MSI (MMR deficient), which is similar to the reported data worldwide (National Comprehensive Cancer Network® (NCCN®)/European Society for Medical Oncology [ESMO]). These tumors are deemed aggressive, recur either locally, or have distant metastasis despite attaining a complete response post- primary treatment. The use of immunotherapy as a part of the adjuvant chemotherapy or maintenance therapy protocol in these subsets need to be researched. The occurrence of different VUS provides a whole lot more genomic alteration, which may become driver mutation after therapy for the sensitive (drug-able) mutation. This is significant as resistant clones may bear these mutations once the initial therapy has eradicated the sensitive clones and lead to drug resistance and recurrence/ relapse. There is a large overlap of genetic alteration in other malignancies where the targeted therapy is already established, and the same can be extrapolated in colorectal cancer. Further studies are warranted to explore targeted therapies in overlapping genomic alterations. In conclusions, colorectal cancer is a heterogeneous disease with different disease biology. The genetic makeup differs for right-sided and left-sided colon cancer. They have different epidemiology, clinicopathological profile and respond differently to a treatment. Tumor mutation burden is an important marker of the aggressiveness of the disease, response to therapy, and recurrence. It is an important marker for the response to checkpoint inhibitors/ immunotherapy. We presented the genomic mutations in colorectal cancers in Indian patients. Tumor mutation burden is maximum in the right-sided lesions (caecum) and gradually decreases towards the left-sided with least in the rectum. High tumor burden is associated with metastasis to the liver, and hence such patients should be closely monitored even after complete response. Targeted therapy against the most common genomic alteration like APC, TP53, and RAS mutations must be established to improve outcomes. Therapy for other mutations like BRCA, MET, PIK3CA, BRAF, ERBB2 mutations should be extrapolated from other malignancies to improve treatment options and response rates. Microsatellite instability-high (MMR deficient) tumors are closely related to high TMB, and these tumors show a good response to immunotherapy in a metastatic setting. Our study highlights the importance of detecting genomic mutations sooner and suggests that genomic mutations should form the basis for customizing and exploring newer targeted therapy against the most common genomic alteration like APC, TP53, and RAS mutations to improve outcomes. Thus, the future of oncology practice colorectal cancer is based on the identification of genetic mutation and customized, targeted therapies progressing from an era of chemotherapy to immunotherapy and biologicals.
Recommendations
All early, locally advanced, and metastatic colorectal cancer cases should undergo NGS testing for TMB and MSI.
Treatment protocol as per the latest guidelines should be followed with the incorporation of treatment agents as per the genetic alteration profile Screening of family members of patients with high MSI, BRCA, CHEK2, ATM, and other gene mutations for other cancers is recommended.
In high TMB and MSI high tumors, immunotherapy should be considered an option in the treatment protocol.
Acknowledgments
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work, and have given final approval for the version to be published. The authors thank Dr. Punit Srivastava of Mediception Science Pvt. Ltd (www.mediception.com) for providing medical writing support during the preparation of this manuscript.
References
- IARC. Colorectal Cancer. Globocan 2020.; 2020:2 https://gco.iarc.fr/today/data/factsheets/cancers/10_8_9-Colorectum-fact-sheet.pdf..
- Trends in colorectal cancer incidence in India. Mathew Thomas Vinay, Baby Basil, Wang Kevin, Lei Feitong, Chen Quan, Huang Bin, Mathew Aju. Journal of Clinical Oncology.2020;38(15_suppl). CrossRef
- ICMR-NCDIR. Report of National Cancer Registry Programme (ICMR-NCDIR).; 2020:282. Accessed October 10, 2021 https://ncdirindia.org/All_Reports/Report_2020/resources/NCRP_2020_2012_16.pdf..
- Wild C, Weiderpass E, Stewart B, World Health Organization. WORLD CANCER REPORT: Cancer Research for Cancer Development. IARC; 2020. .
- Tumor Mutational Burden as a Predictive Biomarker for Response to Immune Checkpoint Inhibitors: A Review of Current Evidence Klempner Samuel J., Fabrizio David, Bane Shalmali, Reinhart Marcia, Peoples Tim, Ali Siraj M., Sokol Ethan S., Frampton Garrett, Schrock Alexa B., Anhorn Rachel, Reddy Prasanth. The Oncologist.2020;25(1). CrossRef
- The Tumor Microenvironment in the Response to Immune Checkpoint Blockade Therapies Petitprez Florent, Meylan Maxime, Reyniès Aurélien, Sautès-Fridman Catherine, Fridman Wolf H.. Frontiers in Immunology.2020;11. CrossRef
- Molecular and Computational Methods for the Detection of Microsatellite Instability in Cancer Baudrin Laura G., Deleuze Jean-François, How-Kit Alexandre. Frontiers in Oncology.2018;8. CrossRef
- Classification and characterization of microsatellite instability across 18 cancer types Hause Ronald J., Pritchard Colin C., Shendure Jay, Salipante Stephen J.. Nature Medicine.2016;22(11). CrossRef
- Microsatellite instability in colorectal cancer: overview of its clinical significance and novel perspectives Battaglin Francesca, Naseem Madiha, Lenz Heinz-Josef, Salem Mohamed E.. Clinical Advances in Hematology & Oncology: H&O.2018;16(11).
- Tumor Mutational Burden as a Predictor of Immunotherapy Response: Is More Always Better? Strickler John H., Hanks Brent A., Khasraw Mustafa. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research.2021;27(5). CrossRef
- Colorectal Cancer in India: An Audit from a Tertiary Center in a Low Prevalence Area Patil Prachi S., Saklani Avanish, Gambhire Pravir, Mehta Shaesta, Engineer Reena, De'Souza Ashwin, Chopra Supriya, Bal Munita. Indian Journal of Surgical Oncology.2017;8(4). CrossRef
- Difference Between Left-Sided and Right-Sided Colorectal Cancer: A Focused Review of Literature Baran Burcin, Mert Ozupek Nazli, Yerli Tetik Nihal, Acar Emine, Bekcioglu Omer, Baskin Yasemin. Gastroenterology Research.2018;11(4). CrossRef
- Right- and left-sided colon cancer - clinical and pathological differences of the disease entity in one organ Mik Michal, Berut Maciej, Dziki Lukasz, Trzcinski Radzislaw, Dziki Adam. Archives of medical science: AMS.2017;13(1). CrossRef
- Right and left-sided colon cancers - specificity of molecular mechanisms in tumorigenesis and progression Mukund Kavitha, Syulyukina Natalia, Ramamoorthy Sonia, Subramaniam Shankar. BMC cancer.2020;20(1). CrossRef
- Left and right sided large bowel cancer Richman Susan, Adlard Julian. BMJ : British Medical Journal.2002;324(7343).
- Annual Report to the Nation on the Status of Cancer, Featuring Cancer in Men and Women Age 20-49 Years Ward Elizabeth M., Sherman Recinda L., Henley S. Jane, Jemal Ahmedin, Siegel David A., Feuer Eric J., Firth Albert U., Kohler Betsy A., Scott Susan, Ma Jiemin, Anderson Robert N., Benard Vicki, Cronin Kathleen A.. Journal of the National Cancer Institute.2019;111(12). CrossRef
- Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer Rizvi Naiyer A., Hellmann Matthew D., Snyder Alexandra, Kvistborg Pia, Makarov Vladimir, Havel Jonathan J., Lee William, Yuan Jianda, Wong Phillip, Ho Teresa S., Miller Martin L., Rekhtman Natasha, Moreira Andre L., Ibrahim Fawzia, Bruggeman Cameron, Gasmi Billel, Zappasodi Roberta, Maeda Yuka, Sander Chris, Garon Edward B., Merghoub Taha, Wolchok Jedd D., Schumacher Ton N., Chan Timothy A.. Science (New York, N.Y.).2015;348(6230). CrossRef
- Beyond Tumor Mutation Burden: Tumor Neoantigen Burden as a Biomarker for Immunotherapy and Other Types of Therapy Wang Peipei, Chen Yueyun, Wang Chun. Frontiers in Oncology.2021;11. CrossRef
- Tumour mutational burden, microsatellite instability, and actionable alterations in metastatic colorectal cancer: Next-generation sequencing results of TRIBE2 study Antoniotti Carlotta, Korn W. Michael, Marmorino Federica, Rossini Daniele, Lonardi Sara, Masi Gianluca, Randon Giovanni, Conca Veronica, Boccaccino Alessandra, Tomasello Gianluca, Passardi Alessandro, Swensen Jeff, Ugolini Clara, Oberley Matthew, Tamburini Emiliano, Casagrande Mariaelena, Domenyuk Valeriy, Fontanini Gabriella, Giordano Mirella, Abraham Jim, Spetzler David, Falcone Alfredo, Lenz Heinz-Josef, Cremolini Chiara. European Journal of Cancer (Oxford, England: 1990).2021;155. CrossRef
- A next-generation sequencing-based strategy combining microsatellite instability and tumor mutation burden for comprehensive molecular diagnosis of advanced colorectal cancer Xiao Jian, Li Wenyun, Huang Yan, Huang Mengli, Li Shanshan, Zhai Xiaohui, Zhao Jing, Gao Chan, Xie Wenzhuan, Qin Hao, Cai Shangli, Bai Yuezong, Lan Ping, Zou Yifeng. BMC cancer.2021;21(1). CrossRef
- Tumor mutational burden quantification from targeted gene panels: major advancements and challenges Fancello Laura, Gandini Sara, Pelicci Pier Giuseppe, Mazzarella Luca. Journal for Immunotherapy of Cancer.2019;7(1). CrossRef
- Analysis of tumor mutational burden: correlation of five large gene panels with whole exome sequencing Heydt Carina, Rehker Jan, Pappesch Roberto, Buhl Theresa, Ball Markus, Siebolts Udo, Haak Anja, Lohneis Philipp, Büttner Reinhard, Hillmer Axel M., Merkelbach-Bruse Sabine. Scientific Reports.2020;10(1). CrossRef
- Harmonization and Standardization of Panel-Based Tumor Mutational Burden Measurement: Real-World Results and Recommendations of the Quality in Pathology Study Stenzinger Albrecht, Endris Volker, Budczies Jan, Merkelbach-Bruse Sabine, Kazdal Daniel, Dietmaier Wolfgang, Pfarr Nicole, Siebolts Udo, Hummel Michael, Herold Sylvia, Andreas Johanna, Zoche Martin, Tögel Lars, Rempel Eugen, Maas Jörg, Merino Diana, Stewart Mark, Zaoui Karim, Schlesner Matthias, Glimm Hanno, Fröhling Stefan, Allen Jeff, Horst David, Baretton Gustavo, Wickenhauser Claudia, Tiemann Markus, Evert Matthias, Moch Holger, Kirchner Thomas, Büttner Reinhard, Schirmacher Peter, Jung Andreas, Haller Florian, Weichert Wilko, Dietel Manfred. Journal of Thoracic Oncology: Official Publication of the International Association for the Study of Lung Cancer.2020;15(7). CrossRef
- Analytic validation of tumor mutational burden as a companion diagnostic for combination immunotherapy in non-small cell lung cancer Fabrizio D. A., Milbury C., Yip W.-K., Ramamurthy L., Bai X., Pattani V., Maness P., Cowen A., Fedorchak K., Ma P., Frampton G. M., Connelly C., Li Y.. Annals of Oncology.2018;29. CrossRef
- Review of Immunogenomics and the Role of Tumor Mutational Burden as a Biomarker for Immunotherapy Response Ros Javier, Baraibar Iosune, Vivancos Ana, Rodon Jordi. Journal of Immunotherapy and Precision Oncology.2019;2(4). CrossRef
- Implementing TMB measurement in clinical practice: considerations on assay requirements Büttner Reinhard, Longshore John W., López-Ríos Fernando, Merkelbach-Bruse Sabine, Normanno Nicola, Rouleau Etienne, Penault-Llorca Frédérique. ESMO open.2019;4(1). CrossRef
- Tumor mutational burden assessed by targeted NGS predicts clinical benefit from immune checkpoint inhibitors in non-small cell lung cancer Alborelli Ilaria, Leonards Katharina, Rothschild Sacha I., Leuenberger Laura P., Savic Prince Spasenija, Mertz Kirsten D., Poechtrager Severin, Buess Martin, Zippelius Alfred, Läubli Heinz, Haegele Jasmin, Tolnay Markus, Bubendorf Lukas, Quagliata Luca, Jermann Philip. The Journal of Pathology.2020;250(1). CrossRef
- Comprehensive cancer-gene panels can be used to estimate mutational load and predict clinical benefit to PD-1 blockade in clinical practice Campesato Luís Felipe, Barroso-Sousa Romualdo, Jimenez Leandro, Correa Bruna R., Sabbaga Jorge, Hoff Paulo M., Reis Luiz F. L., Galante Pedro Alexandre F., Camargo Anamaria A.. Oncotarget.2015;6(33). CrossRef
- Novel algorithmic approach predicts tumor mutation load and correlates with immunotherapy clinical outcomes using a defined gene mutation set Roszik Jason, Haydu Lauren E., Hess Kenneth R., Oba Junna, Joon Aron Y., Siroy Alan E., Karpinets Tatiana V., Stingo Francesco C., Baladandayuthapani Veera, Tetzlaff Michael T., Wargo Jennifer A., Chen Ken, Forget Marie-Andrée, Haymaker Cara L., Chen Jie Qing, Meric-Bernstam Funda, Eterovic Agda K., Shaw Kenna R., Mills Gordon B., Gershenwald Jeffrey E., Radvanyi Laszlo G., Hwu Patrick, Futreal P. Andrew, Gibbons Don L., Lazar Alexander J., Bernatchez Chantale, Davies Michael A., Woodman Scott E.. BMC medicine.2016;14(1). CrossRef
- Tumor mutation burden in Chinese cancer patients and the underlying driving pathways of high tumor mutation burden across different cancer types Jiao Xiao-Dong, Zhang Xiao-Chun, Qin Bao-Dong, Liu Dong, Liu Liang, Ni Jian-Jiao, Ning Zhou-Yu, Chen Ling-Xiang, Zhu Liang-Jun, Qin Song-Bing, Ying Shen-Peng, Chen Xue-Qin, Li Ai-Jun, Hou Ting, Han-Zhang Han, Ye Junyi, Zheng Jingjing, Chuai Shannon, Zang Yuan-Sheng. Annals of Translational Medicine.2020;8(14). CrossRef
- BRAF V600E mutation in colorectal cancer is associated with right-sided tumours and iron deficiency anaemia Sideris Michail, Adams Katie, Moorhead Jane, Diaz-Cano Salvador, Bjarnason Ingvar, Papagrigoriadis Savvas. Anticancer Research.2015;35(4).
- Clinicopathological and protein characterization of BRAF- and K-RAS-mutated colorectal cancer and implications for prognosis Zlobec Inti, Bihl Michel P., Schwarb Heike, Terracciano Luigi, Lugli Alessandro. International Journal of Cancer.2010;127(2). CrossRef
- Mismatch repair genes hMLH1 and hMSH2 and colorectal cancer: a HuGE review Mitchell R. J., Farrington S. M., Dunlop M. G., Campbell H.. American Journal of Epidemiology.2002;156(10). CrossRef
- Familial Breast and Bowel Cancer: Does It Exist? Scott Rodney J, Ashton Katie A. Hereditary Cancer in Clinical Practice.2004;2(1). CrossRef
- The genomic landscapes of human breast and colorectal cancers Wood Laura D., Parsons D. Williams, Jones Siân, Lin Jimmy, Sjöblom Tobias, Leary Rebecca J., Shen Dong, Boca Simina M., Barber Thomas, Ptak Janine, Silliman Natalie, Szabo Steve, Dezso Zoltan, Ustyanksky Vadim, Nikolskaya Tatiana, Nikolsky Yuri, Karchin Rachel, Wilson Paul A., Kaminker Joshua S., Zhang Zemin, Croshaw Randal, Willis Joseph, Dawson Dawn, Shipitsin Michail, Willson James K. V., Sukumar Saraswati, Polyak Kornelia, Park Ben Ho, Pethiyagoda Charit L., Pant P. V. Krishna, Ballinger Dennis G., Sparks Andrew B., Hartigan James, Smith Douglas R., Suh Erick, Papadopoulos Nickolas, Buckhaults Phillip, Markowitz Sanford D., Parmigiani Giovanni, Kinzler Kenneth W., Velculescu Victor E., Vogelstein Bert. Science (New York, N.Y.).2007;318(5853). CrossRef
- Burden of Proof: Evaluating the Efficacy of Tumor Mutational Burden (TMB) in Predicting Response to Immune Checkpoint Inhibitors Newman James, Seetharamu Nagashree, Saif Muhammad Wasif. Cancer Medicine Journal.2020;3(Suppl 2).
- Guanylyl cyclase C in colorectal cancer: susceptibility gene and potential therapeutic target Lin Jieru E, Li Peng, Pitari Giovanni M, Schulz Stephanie, Waldman Scott A. Future oncology (London, England).2009;5(4). CrossRef
- Exploring the multiple roles of guardian of the genome: P53 Feroz Wasim, Sheikh Arwah Mohammad Ali. Egyptian Journal of Medical Human Genetics.2020;21(1). CrossRef
- The Role of p53 Dysfunction in Colorectal Cancer and Its Implication for Therapy Michel Maurice, Kaps Leonard, Maderer Annett, Galle Peter R., Moehler Markus. Cancers.2021;13(10). CrossRef
- The potential for poly (ADP-ribose) polymerase inhibitors in cancer therapy Javle M., Curtin N. J.. Therapeutic Advances in Medical Oncology.2011;3(6). CrossRef
- Alpelisib for PIK3CA-Mutated, Hormone Receptor-Positive Advanced Breast Cancer André Fabrice, Ciruelos Eva, Rubovszky Gabor, Campone Mario, Loibl Sibylle, Rugo Hope S., Iwata Hiroji, Conte Pierfranco, Mayer Ingrid A., Kaufman Bella, Yamashita Toshinari, Lu Yen-Shen, Inoue Kenichi, Takahashi Masato, Pápai Zsuzsanna, Longin Anne-Sophie, Mills David, Wilke Celine, Hirawat Samit, Juric Dejan. The New England Journal of Medicine.2019;380(20). CrossRef
- Alpelisib plus fulvestrant in PIK3CA-mutated, hormone receptor-positive advanced breast cancer after a CDK4/6 inhibitor (BYLieve): one cohort of a phase 2, multicentre, open-label, non-comparative study Rugo Hope S., Lerebours Florence, Ciruelos Eva, Drullinsky Pamela, Ruiz-Borrego Manuel, Neven Patrick, Park Yeon Hee, Prat Aleix, Bachelot Thomas, Juric Dejan, Turner Nicholas, Sophos Nickolas, Zarate Juan Pablo, Arce Christina, Shen Yu-Ming, Turner Stuart, Kanakamedala Hemanth, Hsu Wei-Chun, Chia Stephen. The Lancet. Oncology.2021;22(4). CrossRef
- Patient-reported outcomes in patients with resected, high-risk melanoma with BRAFV600E or BRAFV600K mutations treated with adjuvant dabrafenib plus trametinib (COMBI-AD): a randomised, placebo-controlled, phase 3 trial Schadendorf Dirk, Hauschild Axel, Santinami Mario, Atkinson Victoria, Mandalà Mario, Chiarion-Sileni Vanna, Larkin James, Nyakas Marta, Dutriaux Caroline, Haydon Andrew, Robert Caroline, Mortier Laurent, Lesimple Thierry, Plummer Ruth, Schachter Jacob, Dasgupta Kohinoor, Manson Stephanie, Koruth Roy, Mookerjee Bijoyesh, Kefford Richard, Dummer Reinhard, Kirkwood John M., Long Georgina V.. The Lancet. Oncology.2019;20(5). CrossRef
- Combination dabrafenib and trametinib in the management of advanced melanoma with BRAFV600 mutations Spain Lavinia, Julve Maximilian, Larkin James. Expert Opinion on Pharmacotherapy.2016;17(7). CrossRef
- Comprehensive review of targeted therapy for colorectal cancer Xie Yuan-Hong, Chen Ying-Xuan, Fang Jing-Yuan. Signal Transduction and Targeted Therapy.2020;5(1). CrossRef
- Microsatellite instability as a predictive factor for immunotherapy in malignant melanoma Kubecek Ondrej, Trojanova Petronela, Molnarova Veronika, Kopecky Jindrich. Medical Hypotheses.2016;93. CrossRef
- Pembrolizumab in Microsatellite-Instability–High Advanced Colorectal Cancer André Thierry, Shiu Kai-Keen, Kim Tae Won, Jensen Benny Vittrup, Jensen Lars Henrik, Punt Cornelis, Smith Denis, Garcia-Carbonero Rocio, Benavides Manuel, Gibbs Peter, Fouchardiere Christelle, Rivera Fernando, Elez Elena, Bendell Johanna, Le Dung T., Yoshino Takayuki, Van Cutsem Eric, Yang Ping, Farooqui Mohammed Z.H., Marinello Patricia, Diaz Luis A.. New England Journal of Medicine.2020;383(23). CrossRef
- Antitumor activity of dostarlimab in patients with mismatch repair-deficient/microsatellite instability–high tumors: A combined analysis of two cohorts in the GARNET study. Berton Dominique, Banerjee Susana N., Curigliano Giuseppe, Cresta Sara, Arkenau Hendrik-Tobias, Abdeddaim Cyril, Kristeleit Rebecca Sophie, Redondo Andrés, Leath Charles A., Antón Torres Antonio, Guo Wei, Im Ellie, Andre Thierry. Journal of Clinical Oncology.2021;39(15_suppl). CrossRef
- Efficacy of pembrolizumab in phase 2 KEYNOTE-164 and KEYNOTE-158 studies of microsatellite instability high cancers Diaz L., Marabelle A., Kim T. W., Geva R., Cutsem E. Van, André T., Ascierto P. A., Maio M., Delord J.-P., Gottfried M., Guimbaud R., Jaeger D., Elez E., Yoshino T., Joe A., Lam B., Ding J., Pruitt S., Kang S. P., Le D. T.. Annals of Oncology.2017;28. CrossRef
- Nivolumab plus ipilimumab in metastatic colorectal cancer Gourd Elizabeth. The Lancet Oncology.2018;19(3). CrossRef
- Programmed death-1 blockade in mismatch repair deficient colorectal cancer. Le Dung T., Uram Jennifer N., Wang Hao, Bartlett Bjarne, Kemberling Holly, Eyring Aleksandra, Azad Nilofer Saba, Laheru Dan, Donehower Ross C., Crocenzi Todd S., Goldberg Richard M., Fisher George A., Lee James J., Greten Tim F., Koshiji Minori, Kang SoonMo Peter, Anders Robert A, Eshleman James R., Vogelstein Bert, Diaz Luis A.. Journal of Clinical Oncology.2016;34(15_suppl). CrossRef
- Association of tumour mutational burden with outcomes in patients with advanced solid tumours treated with pembrolizumab: prospective biomarker analysis of the multicohort, open-label, phase 2 KEYNOTE-158 study Marabelle Aurélien, Fakih Marwan, Lopez Juanita, Shah Manisha, Shapira-Frommer Ronnie, Nakagawa Kazuhiko, Chung Hyun Cheol, Kindler Hedy L., Lopez-Martin Jose A., Miller Wilson H., Italiano Antoine, Kao Steven, Piha-Paul Sarina A., Delord Jean-Pierre, McWilliams Robert R., Fabrizio David A., Aurora-Garg Deepti, Xu Lei, Jin Fan, Norwood Kevin, Bang Yung-Jue. The Lancet. Oncology.2020;21(10). CrossRef
- Safety and antitumor activity of the anti-PD-1 antibody pembrolizumab in patients with advanced colorectal carcinoma O'Neil Bert H., Wallmark John M., Lorente David, Elez Elena, Raimbourg Judith, Gomez-Roca Carlos, Ejadi Samuel, Piha-Paul Sarina A., Stein Mark N., Abdul Razak Albiruni R., Dotti Katia, Santoro Armando, Cohen Roger B., Gould Marlena, Saraf Sanatan, Stein Karen, Han Sae-Won. PloS One.2017;12(12). CrossRef
- Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): an open-label, multicentre, phase 2 study Overman Michael J., McDermott Ray, Leach Joseph L., Lonardi Sara, Lenz Heinz-Josef, Morse Michael A., Desai Jayesh, Hill Andrew, Axelson Michael, Moss Rebecca A., Goldberg Monica V., Cao Z. Alexander, Ledeine Jean-Marie, Maglinte Gregory A., Kopetz Scott, André Thierry. The Lancet. Oncology.2017;18(9). CrossRef
- KEYNOTE-177: Phase III randomized study of pembrolizumab versus chemotherapy for microsatellite instability-high advanced colorectal cancer. Shiu Kai-Keen, Andre Thierry, Kim Tae Won, Jensen Benny Vittrup, Jensen Lars Henrik, Punt Cornelis J. A., Smith Denis Michel, Garcia-Carbonero Rocio, Benavides Manuel, Gibbs Peter, De La Fouchardiere Christelle, Rivera Fernando, Elez Elena, Bendell Johanna C., Le Dung T, Yoshino Takayuki, Yang Ping, Farooqui Mohammed Zulfiqar Husain, Marinello Patricia, Diaz Luis A.. Journal of Clinical Oncology.2021;39(3_suppl). CrossRef
- Neoadjuvant immunotherapy shows promise Sidaway Peter. Nature Reviews. Clinical Oncology.2020;17(7). CrossRef
- Biomarkers for immune therapy in colorectal cancer: mismatch-repair deficiency and others Bupathi Manojkumar, Wu Christina. Journal of Gastrointestinal Oncology.2016;7(5). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times