Clinicopathological Profile, Treatment Response and Survival of Cervical Cancer Patients from a Tertiary Cancer Centre in North Karnataka
Download
Abstract
Background: North Karnataka consisting of large rural population doesnot have any report on carcinoma cervix clinical profile and treatment outcomes.
Objectives: analysing the clinicopathological profile and survival data from a tertiary cancer Centre in north Karnataka and comparing it with that of data published worldwide.
Methods: We analysed carcinoma cervix patients from our centre between Oct 2014 to Oct 2016. The clinicopathological, treatment-related parameters, outcomes were analysed.
Results: A total of 360/450 patients treated radically, 60% of the patients were between 40-60 years with the youngest being 22 years and the eldest 84 years. 33.3% of patients had Comorbidity, 85% patients had History of bleeding. 87%were from rural area, 44.8% were literate. 46.6% of patients had stage IIIB followed by II (27.8%), 3.8%had para-aortic node and 3.1% had pelvic nodes. 93.3% had SCC, 80% received chemoradiation, 13%received adjuvant Radiation/chemoradiation and 7% only surgery. Response data available for 320 patients (88.8%) among 320, 74.6% had complete response, Residual disease present in 14%, 3% patients had stable disease and progressive disease in 7%. At 18 months post-treatment, the survival data were available for only 244 (67.7%) patients, out of which 187 patients (67.7%) were alive. Overall 50% of the patients lost to follow up within 3 years of treatment completion. The 3-year survival for the patients who followed up until 3 years was 62.3% (111/178 patients). The stage-wise 3-year survival was 70.6% for stage I, 83.6% for II, 60% for IIIA, 49% for IIIB, 33.3% for IIIC2 (para-aortic nodal involvement) and 28.6% for stage IVA (P-0.001).
Conclusion: Awareness about carcinoma cervix in the rural population is still lacking and they are presenting at an advanced stage, which largely effects on survival of the patients.
Introduction
Carcinoma cervix is the most prevalent cancer and the fourth leading cause of cancer deaths among women worldwide. Estimated to have 570000 cases and almost 311000 penalties [1]. Close to 85% of cervical cancer occurring in growing nations. Cervical cancer is the most prevalent cancer among the Indian women had increased from 0.11 million in 2000 to 0.16 million in 2010 [2]. The proportion ranged from 15% to 55% of Female cancers From all parts of the country. Around 80% of cervical cancer presents at a locally advanced stage and accounts for 80000 deaths in India annually [3]. This is mostly due to Lack of screening in the second most populated country like India.
The standard treatment for the early stage (FIGO IA TO IB1) is radical radiotherapy or Radical surgery. Radical radiation therapy or chemoradiation is the treatment of choice for the Locally advanced stages (FIGO IIB, III and IVA) and an IB bulky disease. The 5- year Survival rates for carcinoma cervix are 95% and above in the case of stage IA, and it reduces to 20% in the case of stage IV [4].
The radiotherapy technique for the treatment of carcinoma cervix has been continuously undergoing evolution from 2D conventional technique to image-guided radiotherapy and from Low dose rate brachytherapy to image-guided brachytherapy. Even though the radiotherapy technique has been improving in the treatment of Carcinoma cervix like image Guided brachytherapy, which established to have superior survival results as evidenced by Retro EMBRACE study [5]. But the radiotherapy facilities are still lacking in developing countries. Which hinders the survival outcome and cancer-related death rate in developing nations. Carcinoma cervix is most commonly the disease that occurs in the rural population [6,7].
North Karnataka consists of the majority of the rural population compared to south Karnataka, according to the 2011 cences of India [8]. There are not a single report of carcinoma cervix from northern Karnataka and none of hospitals registered for hospital-based cancer registry under ICMR. Hence, we conducted a study to analyse the clinicopathological profile and a minimum of 3 yr. survival of carcinoma cervix patients registered in a tertiary cancer centre located in the northern Karnataka.
Objectives
To Assess the clinicopathological profile of the patients attending our centre.
To analyse response to the treatment.
To analyse the three-year survival of the patients and compare the results with published literature.
Materials and Methods
Carcinoma cervix patients registered at a tertiary cancer centre located in the north Karnataka, between October 2014 to October 2016, had retrieved, and patients who underwent treatment with radical intent had included for analysis. Medical records of 450 patients with carcinoma cervix presented during this period have been retrieved and analyzed for patient’s demographic data, tumor-related details, treatment outcomes. Survival data analyses using the follow-up records, telephonic calls and encouraging them for immediate follow up using the contact information provided by them.
Data were analyzed using statistical software, SPSS Inc. Release 2009. PASW Statistics for windows version 18.0, Chicago. The P-value of <0.05 was considered for statistical significance. Variables like age, stage, histology, grade of tumor and comorbidity, were summarized using percentage, mean and standard deviation. 3 years overall survival and stage-wise survival assessed using the Kaplan Meier curve.
The evaluation of patients for diagnosis and staging included clinical examinations, histopathology reports, chest X-rays, ultrasound of abdomen and pelvis, cystoscopy, and proctosigmoidoscopy.patients had staged according to recent Figo staging (2018) .
Standard recommendations are followed as treatment policies at our institute by involving multimodality treatment. The stage Ia1 up to stage Ib1 were treated with radical hysterectomy and pelvic Lymph node dissection, stage Ib2 and IIa patients received adjuvant radiation with or without chemotherapy, depending on Peter’s major criteria, stage III and IVA received concurrent chemoradiation Either with 3 DCRT or IMRT technique to a dose of 45-50 Gy along with concurrent weekly cisplatin 40 mg/m2 or carboplatin AUC 2 chemotherapy followed by HDR brachytherapy to a dose 7Gy in 3 fractions or 6.5 Gy in 4 fractions.
Response to treatment assessed after 6 weeks with combined clinical examination and imaging which includes CT scan abdomen and pelvis or MRI scan. The response documented using RECIST criteria as complete response, partial response, stable disease and progressive disease. A patient who followed up a minimum of 3 years included in survival analysis.
Results
Patients demography and tumor characters (Table 1)
A total of 450 carcinoma cervix patients registered during this period out of which 360 Patients offered radical radiation; 65 patients received palliative treatment. Most common age A group of patients is between 40 to 60 years (60%), with the youngest being 22 years and the eldest was 84 years. 33.3% of patients were associated with Comorbidity, 85% of patients had History of vaginal bleeding, 70% had a history of white discharge per vagina and 32% had h/o Backache. 391 patients among 450 patients, 391 patients (87%) belonged to the rural area and only 202 (44.8%) patients were literate. 30 patients (6.66%) were having associated with HIV infection. The majority of patients had (167 pts, 46.6%) stage IIIB disease followed by stage II (100 patients, 27.8%), stage IIIA (27 patients, 7.5%), stage I (24 patients, 6.6%), stage IVA (17 patients, 4.6%), stage IIIC2 (14 patients, 3.8%) and stage IIIC1 (11 patients, 3.1%). 336 patients (93.3%) had squamous cell histology, 18 (5%) patients had adenocarcinoma histology and 1.7% patient had other histological types which include Adeno-squamous, sarcoma and Nero endocrine varieties. 10 % of patients had high-grade histology, 20% had intermediate grade and 70% of patients had low-grade histology.
| Age Group | Frequency | Percentage |
| <30 | 8 | 2.2 |
| 31-40 | 69 | 19.1 |
| 41-50 | 113 | 31.3 |
| 51-60 | 101 | 28.05 |
| 61-70 | 57 | 15.8 |
| >70 | 12 | 3.3 |
| Comorbidity | ||
| Yes | 120 | 33.33 |
| No | 240 | 66.67 |
| Residency | ||
| Urban | 46 | 12.77 |
| Rural | 314 | 87.2 |
| Stage Wise Distribution | ||
| I | 24 | 6.6 |
| II | 100 | 27.8 |
| IIIA | 27 | 7.5 |
| IIIB | 167 | 46.6 |
| IIIC1 | 11 | 3.1 |
| IIIC2 | 14 | 3.8 |
| IVA | 17 | 4.6 |
| Histology | ||
| SCC | 336 | 93.3 |
| Adeno | 18 | 5 |
| Other | 6 | 1.7 |
Treatment outcomes (Table 2)
Out of 360 patients treated with radical radiation 288 patients (80%) received concurrent chemoradiation followed by HDR brachytherapy, 47 patients (13%) received adjuvant Radiation/chemoradiation and 25 patients (7%) received surgery alone.
| Modality | Frequency | Percentage |
| Post OP RT | 47 | 13 |
| Upfront CTRT | 288 | 80 |
| Surgery Alone | 25 | 7 |
| Treatment Outcome | ||
| Known | 320 | 88.8 |
| Unknown | 40 | 22.8 |
| Response after Treatment | ||
| CR | 239 | 74.6 |
| RD | 45 | 14 |
| SD | 11 | 3 |
| PD | 25 | 7 |
| Survival at 1 Year | ||
| Survival Known | 244 | 67.7 |
| Surviving | 187 | 76.6 |
| Dead | 57 | 23.3 |
| Survival Data at 1.5 Years | ||
| Survival Known | 178 | 50 |
| Surviving | 111 | 62.3 |
| Dead | 67 | 32 |
Abbrevations, Cr, Complete Response; Rd, Residual Disease; Sd, Stable Disease; Pd, Progressive Disease
The median overall treatment time (OTT) was 61 days with 198 patients (55%) completing the treatment within 55 days (Figure 1).
Figure 1. Graph Showing Response to the Treatment. Abbrevations, Cr, Complete Response; Rd, Residual Disease; Sd, Stable Disease; Pd, Progressive Disease.
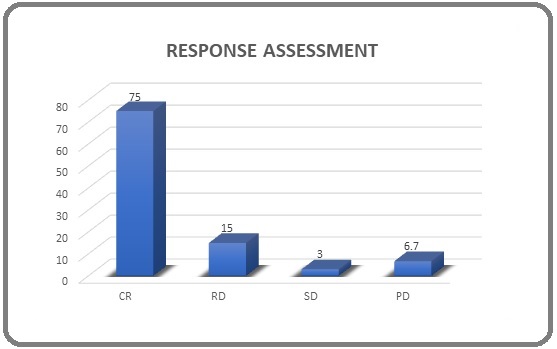
Response assessment data after treatment was available for 320 patients (88.8%), and the complete response after treatment showed by the 239 (74.6%) patients, residual disease present in 45 (14%) patients, stable disease showed by 11 patients (3%) patients and progressive disease in 25 patients (7%), except for complete response other patients were subjected to further management according to standard management guidelines.
Survival outcomes (Figure 2)
An assessment of 3-year survival done for the patients whose follow up was known at least 3 years following completion of treatment due to the large number of missing patients (50%) from the total cohort of the study. At one and half years post-treatment, the survival data were available for only 244 (67.7%) patients, out of which 187 patients (67.7%) were surviving and 57 (23.3%) were dead. The median survival of the study population was 43.5 months.
Figure 2. Kaplan-Meier Curve Representing 3 Year Over All Survival.
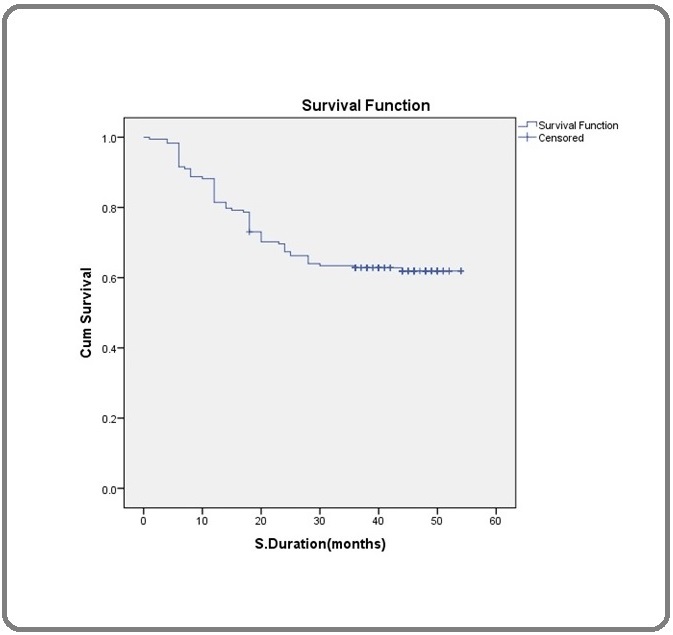
Overall, 50% of the patients lost in the follow up within 3 years of treatment completion. The 3-year survival for the patients who followed up till 3years was 62.3% (111/178 patients). For the overall study cohort if we consider missing patients are due to disease-related event, then it would be 30.8% or if we consider missing patients did not have the event due to disease then it would be 81.3% (Table 3)(Figure 3).
| Survival | ||||
| Stage | Alive | Dead | Total | Survival% |
| I | 12 | 5 | 17 | 70.6 |
| II | 51 | 10 | 61 | 83.6 |
| IIIA | 3 | 2 | 5 | 60 |
| IIIB | 42 | 43 | 85 | 49.4 |
| IIIC2 | 1 | 2 | 3 | 33.3 |
| IVA | 2 | 5 | 7 | 28.6 |
| Total | 111 | 67 | 178 | 62.4 |
Figure 3. Kapalan Meier Curve Representing Stgaewise Survival (P=0.001).
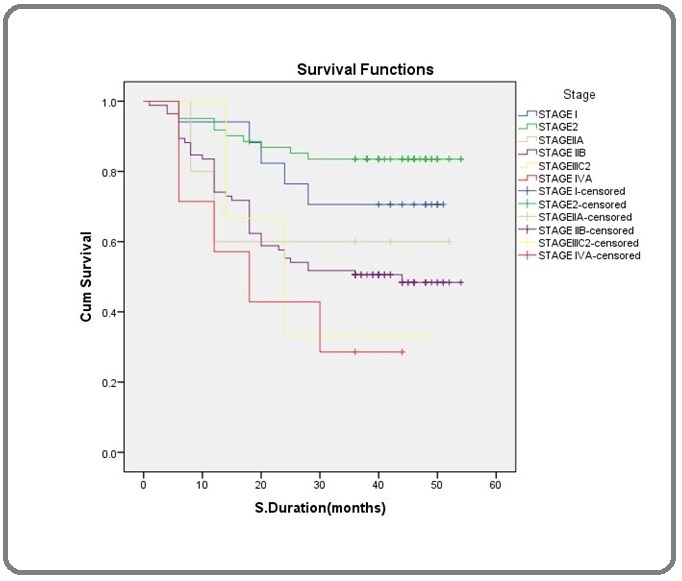
The stage weighs 3-year survival was 70.6% for stage I, 83.6% for stage II, 60% for stage IIIA, 49% for stage IIIB, 33.3% for stage IIIC2 (para-aortic nodal involvement) and 28.6% for stage IVA, which showed statistically significant (p=0.001).
Discussion
Here we analysed clinicopathological profile, response assessment and 3-year survival of carcinoma cervix in a tertiary cancer centre located at north Karnataka which has most of the carcinoma cervix from rural area (87%) unlike study from a tertiary cancer centre from south Karnataka which has 54.7% of carcinoma cervix from rural background [9] and we found that despite efforts to emphasis on the early detection and Screening of carcinoma cervix, awareness is still lacking in rural population and is evident From the fact that the patients in our study presented with advanced stage and only 7% were Candidate for surgery alone compared to the western population where 40% of patient were Candidates for surgery [10].
The median age at presentation in our study population almost Matches western data but in our study most common histological type is squamous cell Carcinoma, which was 93.3% compared to 70% in western data [11]. Although the new case of Carcinoma cervix is decreasing in urban population but in rural area cervical carcinoma Prevalence remains higher [7]. The main reason behind this is because of lack of awareness, Screening programs, neglected attitude towards early symptoms of carcinoma cervix, lack of hygiene, vaccination and access to treatment facilities. Recently Retro EMBRACE study has showed an improved local control by using image-guided brachytherapy and delivering increased dose to the high-risk target volume showed local control of 91% and 3 year OS of 74% [5].
Response to the treatment in our study according to RESIST criteria was 75% patient showed complete response, 15% showed partial response, 3% showed stable disease and 6.7% of patients showed progressive disease which was inferior to the above mentioned study and shows that importance of image guidance and dose escalation to the high-risk volume, but our study is in par with other study assessed the 5-year disease-free survival [12]. In a SEER data analysis of advanced carcinoma cervix treated with chemoradiation the 5-year overall survival was 54% [13] and a similar 54% survival also reported in the National Cancer Database [10], our study showed 3-year overall survival of 62.4%, which is comparable to these studies.The survival in carcinoma varies according to the stage, and stage is the single most predictor of survival in carcinoma cervix. The 5-year age-standardized survival in India was 46%, ranging from 34 to 60% [14]. In our study nearly 70.6% patient of stage I showed 3-year survival but 83.6% of stage II patients showed 3-year survival this was mostly because of the majority of stage II patients underwent concurrent chemoradiation compared to stage I patients whounderwent radical surgery alone which was showing the importance of concurrent chemoradiation but again stage IIIB patients showed 49.4%, patient with para-aortic node showed only 33.3% survival. The survival in our study was significantly correlating with the stage of the disease.
The overall treatment is an important prognostic factor in carcinoma cervix. Our study showed a median overall treatment time of 61 days which almost comparable with other published data [15]. The uniqueness of our study is it had assessed the treatment response after treatment Completion, stage-matched survival and implication of nodal status on survival which many other studies could not do, however, in our study about half of the patient were missing within 3 year of follow up the poor follow up in our study may be because of lack of awareness and concern about the disease among the rural population. Our data results were showing carcinoma cervix patients from rural areas are presenting at advanced stage resulting in reduced survival and treatment outcome due to lack of awareness, screening programs and treatment facilities.
In conclusion, awareness about carcinoma cervix in the rural population is still lacking. The treatment response and survival in carcinoma cervix largely depend on the stage of the disease which emphasis on early detection and treatment of the patients and the survival in our study matches the similar studies published internationally.
References
- Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries F Bray, J Ferlay, I Soerjomataram, Rl Siegel, La Torre, A Jemal. CA: a cancer journal for clinicians.2018;68(6). CrossRef
- An overview of cancer survival in developing countries Sankaranarayanan R, Black RJ, Swaminathan R, Parkin DM. IARC Sci Publ [Internet].1998 [cited 2019 Sep 29];(145):135-73. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10194635.
- Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008 J Ferlay, Hr Shin, F Bray, D Forman, C Mathers, Dm Parkin. International journal of cancer.2010;127(12). CrossRef
- icmr cervix [cited 2019 Sep 29]; Available from: https://www.icmr.nic.in/sites/default/files/reports/Cervix Cancer.pdf..
- Image-guided Adaptive Brachytherapy for Cervix Cancer - A Story of Successful Collaboration within the GEC-ESTRO GYN Network and the EMBRACE Studies Lt Tan, K Tanderup, P Hoskin, R Cooper, R Pötter. Clinical oncology (Royal College of Radiologists (Great Britain)).2018;30(7). CrossRef
- Cancer Statistics India Against Cancer [Internet]. [cited 2020 Jan 6]. Available from: http://cancerindia.org.in/cancer-statistics/..
- Cervical cancer screening in rural India: Status & current concepts Srivastava Anand Narain, Misra Jata Shankar, Srivastava Shruti, Das Bhudav C., Gupta Shilpi. The Indian Journal of Medical Research.2018;148(6). CrossRef
- (No Title) [Internet]. [cited 2020 Jan 6]. Available from: http://censusindia.gov.in/2011census/dchb/2918_PART_A_DCHB_BANGALORE.pdf..
- Feasibility of Concurrent Chemoradiation in Cervical Cancer Patients From Rural Background Harjani Ritika R., Janaki Manur G., Somashekhar Mohankumar, Ponni Arul, Alva Ram C., Koushik Kirthi, Kannan Ram Abhinav, Sathyamurthy Arvind. Clinical Ovarian and Other Gynecologic Cancer.2014;7(1). CrossRef
- Are we appropriately selecting therapy for patients with cervical cancer? Longitudinal patterns-of-care analysis for stage IB-IIB cervical cancer Ja Carlson, C Rusthoven, Pe DeWitt, Sa Davidson, Te Schefter, Cm Fisher. International journal of radiation oncology, biology, physics.2014;90(4). CrossRef
- Cancers of the uterine cervix in Port Harcourt, Rivers State--a 13-year clinico-pathological review Uzoigwe SA, Seleye-Fubara D. Niger J Med [Internet]. [cited 2019 Sep 29].;13(2):110-3.
- Locally advanced cervical cancer: A study of 5-year outcomes S Chopra, M Gupta, A Mathew, U Mahantshetty, R Engineer, G Lavanya, S Gupta, J Ghosh, M Thakur, K Deodhar, S Menon, B Rekhi, J Bajpai, S Gulia, A Maheshwari, R Kerkar, Ts Shylasree, Sk Shrivastava. Indian journal of cancer.2018;55(1). CrossRef
- Trends in the utilization of brachytherapy in cervical cancer in the United States Han Kathy, Milosevic Michael, Fyles Anthony, Pintilie Melania, Viswanathan Akila N.. International Journal of Radiation Oncology, Biology, Physics.2013;87(1). CrossRef
- Cancer survival in Africa, Asia, and Central America: a population-based study Sankaranarayanan Rengaswamy, Swaminathan Rajaraman, Brenner Hermann, Chen Kexin, Chia Kee Seng, Chen Jian Guo, Law Stephen C. K., Ahn Yoon-Ok, Xiang Yong Bing, Yeole Balakrishna B., Shin Hai Rim, Shanta Viswanathan, Woo Ze Hong, Martin Nimit, Sumitsawan Yupa, Sriplung Hutcha, Barboza Adolfo Ortiz, Eser Sultan, Nene Bhagwan M., Suwanrungruang Krittika, Jayalekshmi Padmavathiamma, Dikshit Rajesh, Wabinga Henry, Esteban Divina B., Laudico Adriano, Bhurgri Yasmin, Bah Ebrima, Al-Hamdan Nasser. The Lancet. Oncology.2010;11(2). CrossRef
- Radical radiotherapy treatment (EBRT + HDR-ICRT) of carcinoma of the uterine cervix: outcome in patients treated at a rural center in India Jain Vandana S., Singh Kailash K., Shrivastava Rajeev, Saumsundaram K. V., Sarje Mukund B., Jain Shailendra M.. Journal of Cancer Research and Therapeutics.2007;3(4). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times