CT and MRI Based Gross Tumor Volume Comparison in Pharyngeal and Laryngeal Carcinoma
Download
Abstract
Background: Different other imaging modalities help in accurate gross tumor volume delineation. Studies have shown conflicting results for intermodality GTV comparison. Since in our institute we routinely take planning CT and planning MRI for laryngeal and pharyngeal tumors treated with definitive radiotherapy, with this study we intent to compare the gross tumor volume (GTV) with these modalities in these tumors.
Materials & Methods: Study population included pharyngeal and laryngeal carcinoma patients treated. Planning CT and planning MRI images of these patients were retrieved. Gross tumor volume (GTV) was delineated by a Radiation Oncologist in both these image sets and GTVs were documented.
Results: Out of 87 patients analysed, the overall median GTV with planning CT and planning MRI were 20.4 cc & 18.2 cc respectively. Median GTV with planning CT & MRI for different sites like Nasopharynx, Oropharynx, Larynx and Hypopharynx were 32.85 & 27.75 cc, 22.1 & 20.9 cc, 8.25 & 10.35cc and 20.55 & 20.6 cc respectively with no statistically significant difference. Median GTVs with CT & MRI for different primary tumor stages like T2, T3, T4a, T4b were 14.3 & 14.3 cc, 20.45 & 19 cc, 16.55 & 27.45 cc and 50.75 & 52.4 cc respectively. Analysis showed 94.6 % correlation between GTVs with CT & MRI.
Conclusion: This study showed comparable median GTVs with planning CT & MRI for pharyngeal and laryngeal carcinomas. Subset analysis did not show any significant difference in GTVs with two modalities for different primary tumor site. As expected there was good correlation between GTVs of two modalities. Even though the results does not show significant intermodality variation for GTV delineation. With the results of this study we cannot question the use of multiple modalities for GTV delineation as subtle variation in GTV can result in differences in target volumes resulting in differences in toxicity profile.
Introduction
For conformal radiotherapy International Commission on Radiation Units and Measurements (ICRU) has defined different target volumes like gross tumor volume (GTV), clinical target volume (CTV) and planning target volume (PTV) [1]. In this era of conformal radiotherapy target volume delineation in head and neck cancers is a crucial step. Accurate target volume delineation is mandatory to avoid geographical misses leading to recurrences in view of steep dose gradients. Inaccuracy in tumor delineation is a well recognized error in radiotherapy treatment delivery. [2-4]. In conformal radiotherapy treatment delivery target volume delineation remains a very subjective step. GTV delineation is affected by the type of imaging modality utilised [5]. CT based imaging is most commonly used for defining PTV. Latest treatment planning software allows registration of different imaging modalities with simulation CT images [6, 7]. In laryngeal tumors GTV delineation in CT scan has resulted in significant intra and interobserver variations [8]. Magnetic resonance imaging (MRI) more accurate than CT scan in head and neck tumors to evaluate soft tissue extension and bone invasion. [9]. However there are conflicting results on the utility of multimodality imaging for GTV delineation in pharyngeal and laryngeal cancers [7, 10]. As an institutional practice we are doing planning MRI for pharyngeal and laryngeal carcinoma. Hence with this study we intended to assess the variation in GTV delineation with planning CT and MRI for pharyngeal and laryngeal carcinoma patients. We also aimed to assess the tumor site wise difference in variation in GTV delineation with CT and MRI.
Materials and Methods
This was a retrospective study conducted in Radiation Oncology Department in a tertiary cancer centre from India.
Inclusion Criteria
All pharyngeal and laryngeal carcinoma patients treated with Radical RT/ Chemoradiation during the period 1st January 2019 to 30th June 2019.
Exclusion Criteria
Patients in whom planning MRI images are not available and patients in whom conformal radiotherapy was not used.
Procedure
Case records of the selected patients was retrieved and the demographic details was documented. Planning CT and the co-registered MR images of already treated selected patients were retrieved. Radiation Oncologist delineated GTV in planning CT and planning MRI of each patient after a gap of at least one week, to avoid bias while contouring.
Image Acquisition
Planning CT
Planning CT images were acquired in Wipro GE OPTIMA 580W 16 slice machine. Patients were immobilized with neck rest and thermoplastic shell. Intravenous contrast were given while taking planning CT. 2.5 mm slice thickness CT images of neck and thorax region were acquired.
Planning MRI
MRI images were acquired on 1.5 Tesla Signa HDtX machine. Patient were immobilized in same position and with the same thermoplastic mould which were used for planning CT. Axial T2 weighted (TR-6460,TE 112), FOV 26 × 26, Matrix 320 × 192, NEX-4 and axial STIR (TR-6940,TE- 49.8,T1-140), FOV-26 × 26, Matrix 320 × 160, NEX-2 sequences were acquired.
Statistical analysis
Descriptive statistics like frequencies, percentages, median with interquartile range were used wherever appropriate. Mann-Whitney test was used for median comparison of GTVs. Pearson correlation test was used to find out the correlation between GTVs. Blant Altmann plot was used to plot mean GTV and average difference between GTVs.
Results
Total of 87 patient details were analysed. Median age of the patients were 62 years (Range 19-78). Majority were male patients 82 (94%). Among the study patients, the most common primary site was Oropharynx (52%) and site wise distribution of patients is shown in Table 1.
| Primary site | Frequency | Percent |
| Nasopharnyx | 4 | 4.6 |
| Oropharnyx | 45 | 51.7 |
| Larynx | 24 | 27.6 |
| Hypopharnyx | 14 | 16.1 |
| Total | 87 | 100 |
Patients were distributed among different tumor (T) as per TNM staging. The most common T stage was T3 (55%). Number of patients in different T stages like T1, T2,T3 and T4 were 1, 24, 48 and 14 respectively.
Median GTV in planning CT was 20.40 cc and it ranged from 1.1 to 85.8 cc. Median GTV in planning MRI was 18.20 and it ranged from 1.9-108.7 cc. Table 2 shows median GTVs in planning CT & MRI. Median comparison with Mann Whitney test did not show any statistically significant difference.
| Median GTV | Inter Quartile range (IQR) | No. of patients | P value | |
| Planning CTGTV | 20.4 | 8.90-30.30 | 87 | |
| Planning MRGTV | 18.2 | 9.30-29.60 | 87 | 0.544 |
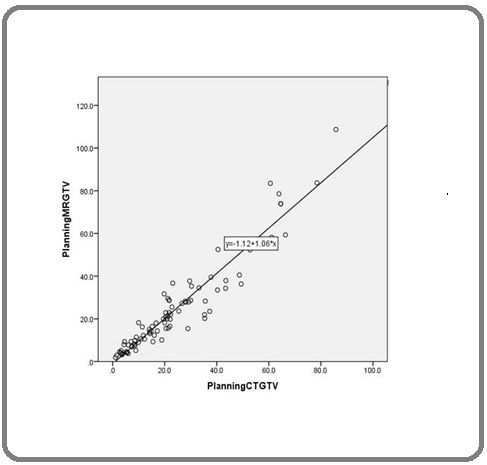
Pearson correlation showed a strong correlation between Planning CT & planning MRI GTVs. 94.9% correlation was observed which was statistically significant (p < 0.01) and the scatter plot of the same is shown in Figure 1.
Figure 1. Scatter Plot Showing Correlation between Gross Tumor Volumes (GTVs) among Pharyngeal and Laryngeal Carcinoma Patients.
Primary sitewise GTVs in planning CT & MRI were analysed. Table 3 shows median GTVs in each site and median comparison between GTVs.
| Primarysite | Median | IQR | N | p value | |
| Nasopharnyx | Planning CT GTV | 32.85 | 24.08-45.38 | 4 | |
| Planning MR GTV | 27.75 | 17.42-39.20 | 4 | 0.49 | |
| Oropharnyx | Planning CT GTV | 22.1 | 11.85-41.95 | 45 | |
| Planning MR GTV | 20.9 | 10.30- 37.80 | 45 | 0.59 | |
| Larynx | Planning CT GTV | 8.25 | 3.38-21.58 | 24 | |
| Planning MR GTV | 10.35 | 4.13-24.85 | 24 | 0.44 | |
| Hypopharnyx | Planning CT GTV | 20.55 | 14.65-21.85 | 14 | |
| Planning MR GTV | 20.6 | 14.18-28.63 | 14 | 0.8 |
Pearson correlation between GTVs in each site is shown in Table 4, with all sites showing statistically significant correlation, except for Nasopharynx.
| Primary site | r value | P value |
| Orophaynx | 95.30 % | < 0.01 |
| Nasopharynx | 73 % | 0.27 |
| Larynx | 97.70 % | <0.01 |
| Hypopharynx | 80 % | <0.01 |
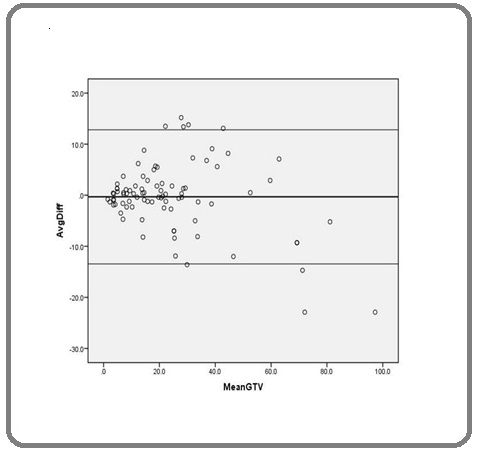
Bland Altman Plot showing that as mean GTV volume increases there is increase in difference between planning CT & MRI GTVs is shown in Figure 2.
Figure 2. Bland Altman Plot Showing the Mean GTV and Average Differences among Pharyngeal and Laryngeal Carcinoma Patients.
Analysis was done to check whether there was difference in GTVs in planning CT and planning MRI in different T stage of tumor. There was no statistically significant difference in GTVs in different T stages of tumor and the same is shown in Table 5.
| T stage | No. of patients | Median Planning CT GTV | Median Planning MRI GTV | P value |
| T2 | 23 | 14.3 | 14.3 | 0.62 |
| T3 | 48 | 20.45 | 19 | 0.54 |
| T4a | 4 | 16.55 | 27.45 | 0.69 |
| T4b | 10 | 50.75 | 52.4 | 1 |
Discussion
Median age of patients in our study was 62 years. Out of the total 87 patients, 82 (94%) were males. In our study around 45 (51.7%) of patients had oropharyngeal primary. Among the rest of the patients, 24 (27.6%) had laryngeal, 14 (16.1%) had hypopharyngeal and 4 (5.1%) had nasopharyngeal primary tumors. In study by Bird et al all 11 patients had Oropharyngeal primary [11]. In study by Daisne et al 13 out of 29 (45%) had laryngeal, 10 had oropharyngeal and 6 had hypopharyngeal primary disease [7]. In study by Anderson et al 9 out of 14 (64%) patients had oropharyngeal primary disease [5].
In our study 62 (71%) patients had T3 or above tumor stages of disease. In our study 56 (64.3%) patients had node positive disease. But in this study we have looked at only the GTV of primary tumor and we have not seen the GTV of gross node.Various similar studies also studied volumes of primary tumor [7, 10, 11].
In this study median GTV with planning CT & MRI were 20.44 cc & 18.2 cc respectively. In our study sitewise GTVs with planning CT & MRI for different sites, Oropharynx (22.10 & 20.90) cc, Larynx (8.25 & 10.35) cc, Hypopharynx (20.55 & 20.6) cc and Nasopharynx (32.85 & 27.75) cc respectively. In study by Geet et al GTVs in planning CT by different observers ranged from 31.1 to 34.7 cc and with MRI it ranged from 29.4 to 31.5 cc for laryngeal tumors and for pharyngeal tumors it was 18.1 to 21.9 cc with CT and 19.3 to 21.8 cc with MRI respectively. This study did not show difference in volumes with CT and MRI [10]. Study by Daisne et al showed an average GTV for oropharyngeal with planning CT and MRI of 32.1 cc & 27.9 cc and for laryngophryngeal primaries of 21.4 cc & 21.4 cc respectively. This study also did not demonstrate any difference in volumes with two modalities. In study by Bird et al mean GTVs for oropharyngeal tumors with CT & MRI were 11.9 & 12.7 cc and was documented as statistically significant [11]. Our study did not show any significant difference with CT & MRI GTVs as a whole and also on sitewise subset analysis. Our study also did not show any significant difference in GTVs with two modalities as T (tumor) stage advanced. But as the mean GTV increased there was a trend towards difference in GTVs with two modalities.
As expected correlation analysis showed excellent positive correlation with GTVs of CT & MRI. For nasopharyngeal site primary the correlation value was less compared to other sites, possible reason could be lesser number of nasopharyngeal patients.
Study by Bird et al looked at intermodality and interobserver variation in target delineation in Oropharyngeal cancers with CT,MRI and PET CT. In this study GTVs were drawn by 5 physicians, including 2 radiologist and 3 radiation Oncologist [11]. Daisne et al studied target volumes in laryngopharyngeal tumors with different modalities such as CT, MRI and PET CT scan [7]. But in our centre as an institutional policy planning MRI is taken apart from CT simulation to aid in GTV delineation in Laryngopharyngeal tumors. In our centre PET CTis not regularly done for these patients. Hence with this study we investigated intermodality variation with CT & MRI only. In our study tumor volumes were drawn by a single radiation oncologist and we have not investigated interobserver variability.
PET CT was not used in our study as compared to similar studies. Our study did not investigate the interobserver variability. These are limitations of our study. But similar studies were done with less number of patients compared to our study and this adds to the strength of our study. In future we are planning for studies investigating interobserver, multiple modality variability in GTV delineation.
In conclusion, this study showed comparable median GTVs with planning CT & MRI of 20.4 & 18.2 cc respectively. Subset analysis did not show any significant difference in GTVs with two modalities for different primary tumor site. As expected there was good correlation between GTVs of two modalities in this study. Eventhough the results does not show significant intermodality variation for GTV delineation, the difference in GTVs were bigger for larger tumors. With the results of this we cannot question the use of multiple modalities for GTV delineation as subtle variation in GTV can result in differences in target volumes resulting differences in toxicity profile. Future studies should be undertaken including other modalities like PET CT and also look for intermodality and interobserver variation in GTV.
Acknowledgements
The authors acknowledge Dr Mohandoss for analyzing the data and reviewing the manuscript. The authors also acknowledge the other staffs of radiation oncology at the center.
References
- Report 62 Landberg T., Chavaudra J., Dobbs J., Gerard J. -P., Hanks G., Horiot J. -C., Johansson K. -A., Möller T., Purdy J., Suntharalingam N., Svensson H.. Journal of the ICRU.1999;os32(1). CrossRef
- Delineating neck targets for intensity- modulated radiation therapy of head and neck cancer. What we learned from marginal recurrences? David Merav Ben, Eisbruch Avraham. Frontiers of Radiation Therapy and Oncology.2007;40. CrossRef
- Recurrences near base of skull after IMRT for head-and-neck cancer: implications for target delineation in high neck and for parotid gland sparing Eisbruch Avraham, Marsh Lon H., Dawson Laura A., Bradford Carol R., Teknos Theodoros N., Chepeha Douglas B., Worden Francis P., Urba Susan, Lin Alexander, Schipper Matthew J., Wolf Gregory T.. International Journal of Radiation Oncology, Biology, Physics.2004;59(1). CrossRef
- Patterns of failure and toxicity after intensity-modulated radiotherapy for head and neck cancer Schoenfeld Gordon O., Amdur Robert J., Morris Christopher G., Li Jonathan G., Hinerman Russell W., Mendenhall William M.. International Journal of Radiation Oncology, Biology, Physics.2008;71(2). CrossRef
- Interobserver and intermodality variability in GTV delineation on simulation CT, FDG-PET, and MR Images of Head and Neck Cancer Anderson CM, Sun W, Buatti JM, Maley JE, Policeni B, Mott SL, et al . Jacobs J Radiat Oncol 2014;1:006..
- Target volume delineation in oropharyngeal cancer: impact of PET, MRI, and physical examination Thiagarajan Anuradha, Caria Nicola, Schöder Heiko, Iyer N. Gopalakrishna, Wolden Suzanne, Wong Richard J., Sherman Eric, Fury Matthew G., Lee Nancy. International Journal of Radiation Oncology, Biology, Physics.2012;83(1). CrossRef
- Tumor Volume in Pharyngolaryngeal Squamous Cell Carcinoma: Comparison at CT, MR Imaging, and FDG PET and Validation with Surgical Specimen Daisne Jean-François, Duprez Thierry, Weynand Birgit, Lonneux Max, Hamoir Marc, Reychler Hervé, Grégoire Vincent. Radiology.2004;233(1). CrossRef
- Laryngeal tumor volume measurements determined with CT: A study on intra- and interobserver variability Hermans Robert, Feron Michel, Bellon Erwin, Dupont Patrick, Van den Bogaert Walter, Baert Albert L.. International Journal of Radiation Oncology*Biology*Physics.1998;40(3). CrossRef
- Tumours of the oropharynx and oral cavity: Perineural spread and bone invasion Maroldi R, Battaglia G, Farina D, Maculotti P, Chiesa A. J Belge Radiol.1999;82:294-300.
- Inter-observer variability in the delineation of pharyngo-laryngeal tumor, parotid glands and cervical spinal cord: comparison between CT-scan and MRI Geets Xavier, Daisne Jean-François, Arcangeli Stephano, Coche Emmanuel, De Poel Marian, Duprez Thierry, Nardella Grazia, Grégoire Vincent. Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2005;77(1). CrossRef
- Multimodality imaging with CT, MR and FDG-PET for radiotherapy target volume delineation in oropharyngeal squamous cell carcinoma Bird David, Scarsbrook Andrew F., Sykes Jonathan, Ramasamy Satiavani, Subesinghe Manil, Carey Brendan, Wilson Daniel J., Roberts Neil, McDermott Gary, Karakaya Ebru, Bayman Evrim, Sen Mehmet, Speight Richard, Prestwich Robin J.D.. BMC Cancer.2015;15(1). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times