Predictors of Knowledge of Human Papillomavirus Infection and Its Related Diseases: A Study of Women in a Nigerian Tertiary Institution
Download
Abstract
Background: The burden of HPV infection and its diseases is very high in Sub-Saharan Africa and unfortunately many vulnerable women in this region have little or no knowledge about the infection and its diseases. Bearing in mind the vital role knowledge plays in disease prevention and control, our study aimed to assess women’s knowledge about relevant aspects of human papillomavirus (HPV) infection & its related diseases and to predict the factors that influence their knowledge.
Material and methods: A cross-sectional study conducted among 500 women attending a tertiary health institution in Nigeria using a self-administered structured questionnaire to assess knowledge about HPV infection, its related diseases and associated risk factors. Knowledge scores were derived, participants were categorized into having either good or poor knowledge and factors associated with good knowledge were assessed. Data was analyzed was using Statistical Package for Social Sciences version 23.0.
Results: The knowledge of HPV infection & its diseases was poor with only 26.3% (123/468) of participants having good level of knowledge. Worse still, only 21.4% believed that they were at risk of acquiring the infection. Tertiary education (AOR=2.40, CI=1.30-4.44, P=0.005), low parity (AOR=4.22, CI=1.40-12.66, P=0.011), and having electronic media (AOR=6.06, CI=2.86-12.9, P<0.001), print media (AOR=4.00, CI=1.21-13.16, P=0.023), healthcare professionals (HCP) (AOR=6.30, CI=3.56-11.11, P<0.001) and organized program (AOR=13.16, CI=5.08-34.48, P<0.001) as primary sources of information significantly predicted good knowledge of HPV infection & its related diseases.
Conclusion: Knowledge of HPV infection and its related diseases is very low among Nigerian women in our study. Tertiary education, low parity and having electronic media, print media, HCP and organized health programs as primary sources of information significantly predicted of good knowledge. Health education through these information channels may help to bridge the gap in knowledge and improve public knowledge about HPV and its related diseases.
Introduction
Human papillomavirus (HPV) is the most common sexually transmitted infection worldwide [1,2] and it is most prevalent in the early reproductive years [1,3]. The global prevalence of HPV infection in women with normal cervical cytology has been reported as 11 – 12%, with Sub-Saharan Africa recording the highest prevalence rate of 24% [4,5]. The prevalence of the infection rises exponentially to greater than 90% in the presence of high grade precancerous lesions or invasive cervical cancer (CC) [2,4]. A significant proportion of sexually active women acquire the infection at one point or the other in their lifetime [6]. However, 70-90% of the infections are asymptomatic and are usually cleared from the body within one to two years [3,6]. Only persistent infections result into HPV related disease, among which cancer is a common sequelae [5]. Six types of cancers are known to be associated with HPV infection and these include cervical, penile, vulvar, vaginal, anal and oropharyngeal cancers [4]. Approximately all cases of CC, 88% of anal cancers, 78% of vaginal cancers, 15–48% of vulvar cancer, 51% of penile cancers and 13-60% of oropharyngeal cancers are caused by high risk HPV (HrHPV) [3,7]. Among these, CC is the most prevalent, accounting for 84% of all the HPV related malignancy [5]. Though, CC is the fourth most common cancer and cause of cancer death in women worldwide, it is the most frequently diagnosed genital cancer and cause of mortality in Sub-Saharan African women [8]. In Nigeria, it is the second most common female cancer and cause of female cancer mortality after breast cancer, accounting for 12,075 new cases and 7,968 deaths in 2020 respectively [9].
HPV is classified based on its potential to cause malignancy into HrHPV or oncogenic HPV and low risk HPV (LrHPV) or non-oncogenic HPV [3,10]. HrHPV is the cause of HPV related cancers while LrHPV are responsible for common anogenital warts such as vulvar, penile and perineal warts. Approximately 90% of all anogenital warts are believed to be caused by HPV 6 and 11 [5]. HrHPV 16 & 18 are the predominant causes of HPV related malignancies. These two serotypes account for 71% of all CC cases [11], 85% of oropharyngeal cancers and 87% of anal cancers [6]. Others are serotypes 45, 31, 33, 39, 51 52, 56, 58, 66, & 68 [3,12]. Several factors have been shown to increase the risk of HPV acquisition and persistence among women. These factors include presence of HIV infection, co-infection with other sexually transmitted infections like Chlamydia trachomatis, gonorrhea and herpes simplex, tobacco smoking, long-term oral contraceptives use, immune-compromise, high parity and early age at pregnancy [5,8,10,13]. Persistent HrHPV infection and its associated diseases are preventable. HPV vaccination, HPV DNA testing, conventional Pap test, liquid-based cytology and visual inspection with acetic acid are recommended methods of prevention among women [3,6,13].
Despite the high prevalence of HPV infection and its disease burden in our environment [2,4,5,8,9], there is still a significant knowledge gap about the infection and its associated diseases among the populace [14-18]. Knowledge is a critical determinant of acceptability and success of public health strategy and intervention [19]. As Nigeria prepares to join the League of Nations in reducing the burden of HPV associated diseases especially CC through implementation of population based HPV vaccination and other preventive strategies, it is imperative to evaluate the knowledge of her vulnerable populace about HPV infection and the diseases it causes. This study aimed to assess women’s knowledge about HPV infection and its related diseases, and to determine the factors that predict such knowledge. This will provide baseline evidence for appropriate public health interventions geared towards reduction of the burden of HPV related diseases especially CC disease in our environment.
Materials and Methods
Study design and setting
This was a cross-sectional descriptive study conducted among women attending Lagos University Teaching Hospital (LUTH), Lagos, Nigeria. LUTH is the largest tertiary hospital in Lagos, Nigeria and the main referral center for many public and private hospitals in Lagos and its environs.
Study population and recruitment of study participants
The study was conducted among women attending outpatient clinics at LUTH. Four outpatient clinics were randomly selected by ballot method out of the eight major outpatient clinics in the hospital. The selected clinics were medical outpatient clinic, surgical outpatient clinic, gynaecological outpatient clinic and community health outpatient clinic. Appropriate sample size was determine using the formula (n = Z2 p (1 − p)/d2) [20] with an absolute error margin of 5% (d = 0.05), type 1 error of 5% (Z = 1.96), and proportion of women with knowledge of HPV (p) of 67.1% [21]. The calculated minimum sample size was 339 and after adjusting for a non-response rate of 20%, the final sample size was 407.
Women attending the selected outpatient clinics who are 18 years and above and who gave informed consent were recruited into the study. Those unwilling to participate in the study and with personal history of HPV related diseases such as genital warts, cervical, vulvar or vaginal cancer were excluded from the study. Women who meet the eligibility criteria were enrolled into the study. The study participants were equally distributed across the four selected clinics with equal number of women recruited from each clinic. Participants were recruited consecutively until the allotted sample size was obtained.
Instrument of survey and data collection
A structured questionnaire was designed and used to obtained information from the study participants. Information on socio-demographic characteristics, reproductive characteristics, awareness and general knowledge of HPV infection was obtained. Information on knowledge of HPV associated diseases, risk factors for HPV infections and its related diseases was also obtained. The socio-demographic characteristics elicited included age, tribe, occupation, religion; educational and marital status. Information on total number of deliveries was also obtained. Women with less than 5 deliveries were regarded as having low parity while women with 5 or more deliveries were regarded as having high parity. Knowledge of HPV infection was assessed by asking the participants if they have heard of HPV before, if HPV can cause infection in women, how common HPV infection was in women and if HPV can cause infection in men. Questions such as “are sexually active women at risk of having HPV infection?”, “are you at risk of having HPV infection?”, “can HPV infection can cause problem?” and on mode of acquisition of HPV were also asked to assess their knowledge of HPV infection. Primary sources of information about HPV and its related diseases were also inquired about by asking “how did you get to know about HPV and its diseases?” Furthermore, knowledge about diseases associated with HPV infection was assessed by asking respondents if they were aware of any disease caused by HPV infection, the type of diseases caused by HPV and what genital warts (GW) and CC are. They were also asked about the part of the female genital tract that is most frequently affected by GW and the type of female cancer that is most commonly associated with HPV infection. Finally, knowledge about risk factors for HPV infection and its diseases was assessed by asking the participants to identify the factors that increase the risk of acquisition and persistence of HPV infection. These included having multiple sexual partners, having partners with multiple sexual partners, early age at first sexual intercourse and engaging in homosexuality. Others included presence of other STI like chlamydia, smoking, HIV/AIDS and immune suppression.
Knowledge score was calculated for knowledge on HPV infection, HPV related diseases and risk factors for HPV and its diseases by using a scoring system adapted from a similar study [22]. Every question answered correctly was score one point while a wrongly or inappropriately answered question was scored zero. The total maximum score for knowledge on HPV infection was eight while the minimum was zero. A score of ≥4 was adjudged good while a score of <4 was adjudged poor. The total maximum score for knowledge about HPV associated diseases was twelve while the minimum was zero. A score of ≥6 was adjudged good while a score of <6 was adjudged poor. The total maximum score for knowledge of risk factors for HPV infection and associated diseases was eight while the minimum was zero. A score of ≥4 was adjudged good while a score of <4 was adjudged poor. These scores were added together to derive the cumulative score for knowledge of HPV and its associated diseases. The maximum score was twenty- eight and the least score was zero. A score of ≥14 was adjudged good while a score of <14 was adjudged poor. Five hundred (500) questionnaires were self- administered to the study participants after an initial pilot study. The pilot study was carried out at the general outpatient clinic department in LUTH among a convenient sample of 20 women who attended the clinic and who had given consent to participate in the pilot study. The questionnaire was tested for the appropriateness of its content and clarity of its instructions. The outcome of the pilot study was used to revise the final study questionnaire as appropriate and the data from the pilot study was not included in the final study data. The study questionnaires were administered to 125 consecutive participants in each of the selected clinics; all the respondents were encouraged to fill the questionnaires completely and these were retrieved immediately after completion.
Data analysis
Participants’ data was anonymized and entered into Excel spreadsheet and data cleaning and validation was done. Data was analyzed using Statistical Package for Social Sciences (SPSS) version 23.0, IBM Corp., Armonk, NY, USA. Descriptive statistics were computed for all relevant data and presented in frequencies and percentages using tables or charts. Normally distributed continuous variables were expressed as mean ± standard deviation (SD) while non-normally distributed continuous variables were expressed as median and interquartile range (IQR). Knowledge variables were dichotomized into “good” and “poor” based on the cut off criteria stipulated above. Bivariate analysis was done using Student’s t-test (or Mann Whitney U test) and Pearson’s Chi- square test to compare continuous variables and categorical variables respectively. Fischer’s exact test was used in place of Pearson’s Chi- square test when the expected cell value was less than 5. Univariable regression analysis was done and crude odd ratios derived. Multivariable regression analysis was conducted using stepwise backward elimination technique after including variables with univariable P-value < 0.2. The level of statistical significance was set at a P-value < 0.05 and confidence interval at 95%.
Ethical consideration
Ethical approval was obtained from the Human Research and Ethical committee of LUTH before conducting the study (ADM/DCST/HREC/APP/2280). Informed consent was obtained from the participants prior to their participation in the study and the study was carried out in accordance with the Declaration of Helsinki (1964).
Results
Out of 500 questionnaires that were administered, only 493 were retrieved (98.6%), while 468 (93.6%) were appropriately filled and used for analysis. The mean age of the respondents was 35.5±10.1 years (range 18–83 years) with majority [311/468 (66.5%)] within the age group of 21–40 years. Most of the respondents were married [328/468 (70.1%)] with tertiary education [317/468 (67.7%)] and skilled occupation [244/468 (52.1%)] (Table 1).
| Variable | Frequency (n = 468) | Percentage (%) |
| Age (in years) | ||
| < 21 | 29 | 6.2 |
| 21 – 30 | 120 | 25.7 |
| 31 – 40 | 191 | 40.8 |
| 41 – 50 | 98 | 20.9 |
| 51 – 60 | 21 | 4.5 |
| > 60 | 9 | 1.9 |
| Mean age = 35.5+10.1 years | ||
| Marital status | ||
| Married | 328 | 70.1 |
| Single | 111 | 23.7 |
| Others* | 29 | 6.2 |
| Highest level of education | ||
| No formal education | 16 | 3.4 |
| Primary | 12 | 2.6 |
| Secondary | 123 | 26.3 |
| Tertiary | 317 | 67.7 |
| Occupational status | ||
| Professional | 18 | 3.8 |
| Skilled | 244 | 52.1 |
| Semi-skilled | 129 | 27.6 |
| Unskilled | 5 | 1.1 |
| Unemployed | 72 | 15.4 |
| Religion | ||
| Christianity | 392 | 83.8 |
| Islam | 72 | 15.4 |
| Traditional | 4 | 0.8 |
| Tribe | ||
| Yoruba | 262 | 56 |
| Igbo | 141 | 30.1 |
| Hausa | 9 | 1.9 |
| Others# | 56 | 12 |
| Parity | ||
| 0 | 176 | 37.6 |
| 1 – 4 | 232 | 49.6 |
| >4 | 60 | 12.8 |
* Divorced, separated, cohabiting; # Tiv, Ijaw, Urhobo, Fulani, Edo, Egun
Table 2 shows the distribution of participants’ knowledge of HPV infection and its related diseases. Regarding knowledge about HPV, less than half of the respondents [229/648 (48.9%)] have heard about HPV. Though respondents believed that HPV infection occurs more in women [226/468 (48.3%)] than in men [139/468 (29.7%)], only 5.3% (25/468) and 32.9% (154/468) believed that the infection is common and sexually active women were at risk of acquiring the infection respectively. Less than a quarter of respondents [100/468 (21.4%)] believed that they were at risk of HPV infection. With regards to knowledge of HPV related diseases, only 42.7% (200/468) knew of any disease caused by HPV infection while barely 18.2% (85/468) knew that HPV could cause both cancer and non-cancer related diseases. Though 51.1% (239/468) of the respondents knew what CC is, only 29.5% (138/468) knew that it is associated with HPV infection. Likewise 43.8% (205/468) of respondents knew what GW are but only 28.0% (131/468) knew that it is related to HPV infection.
| Variables | Frequency (n = 468) | Percentage (%) |
| Knowledge of Human Papilloma Virus infection | ||
| Awareness of HPV | ||
| Yes | 229 | 48.9 |
| No | 239 | 51.1 |
| Can HPV infection occur in women? | ||
| Yes | 226 | 48.3 |
| No | 107 | 22.9 |
| Don’t know | 135 | 28.8 |
| Can HPV infection occur in men? | ||
| Yes | 139 | 29.7 |
| No | 22 | 4.7 |
| Don’t know | 307 | 65.6 |
| Can HPV infection cause problem? | ||
| Yes, it always cause problem | 152 | 32.5 |
| Yes, sometimes it does | 63 | 13.5 |
| No, it never cause problem | 61 | 13 |
| Don’t know | 192 | 41 |
| How is HPV infection acquired? | ||
| Sexual intercourse | 226 | 48.3 |
| Exposure to contaminated blood | 25 | 5.3 |
| Consuming contaminated food | 4 | 0.9 |
| Inhaling contaminated air | 13 | 2.8 |
| Don’t know | 200 | 42.7 |
| How common is HPV infection among women? | ||
| Very rare | 74 | 15.8 |
| Not common | 72 | 15.4 |
| Common | 71 | 15.2 |
| Very common | 25 | 5.3 |
| Don’t know | 226 | 48.3 |
| Are sexually active women at risk of infection? | ||
| Yes | 154 | 32.9 |
| No | 43 | 9.2 |
| Don’t know | 271 | 57.9 |
| Are you at risk of HPV infection? | ||
| Yes | 100 | 21.4 |
| No | 176 | 37.6 |
| I don’t know | 192 | 41 |
| Knowledge of HPV related diseases | ||
| Knowledge of a disease caused by HPV | ||
| Yes | 200 | 42.7 |
| No | 29 | 6.2 |
| Don’t know | 239 | 51.1 |
| What types of disease does HPV causes? | ||
| Only cancer related diseases | 73 | 15.6 |
| Only non-cancer related diseases | 42 | 9 |
| Both non-cancer and cancer related diseases | 85 | 18.2 |
| Don’t know | 268 | 57.2 |
| Diseases known to be associated with HPV* | ||
| Cervical cancer | 138 | 29.5 |
| Genital warts | 131 | 28 |
| Pre-cancerous lesions in the genital areas | 111 | 23.7 |
| Vaginal cancer | 104 | 22.2 |
| Vulva cancer | 74 | 15.8 |
| Anal warts | 67 | 14.3 |
| Type of cancer thought to be most commonly associated with HPV infection | ||
| Cervical cancer | 121 | 25.9 |
| Vaginal cancer | 66 | 14.1 |
| Vulva cancer | 13 | 2.8 |
| Don’t know | 268 | 57.2 |
| Knew that cervical cancer affects the mouth of the womb | ||
| Yes | 239 | 51.1 |
| No | 39 | 8.3 |
| Don’t know | 190 | 40.6 |
| Knew that genital warts are abnormal fleshy growth in private parts | ||
| Yes | 205 | 43.8 |
| No | 13 | 2.8 |
| Don’t know | 250 | 53.4 |
| Part of the female private part most commonly affected by warts | ||
| Vulva | 138 | 29.5 |
| Vaginal | 52 | 11.1 |
| Cervix | 15 | 3.2 |
| Don’t know | 263 | 56.2 |
| Knowledge of risk factors associated with HPV infection and diseases* | ||
| Risk factors | ||
| Having multiple sexual partners | 229 | 48.9 |
| Having partners with multiple sexual partners | 224 | 47.9 |
| Presence of other STIs | 193 | 41.2 |
| Engaging in unsafe sexual practices | 184 | 39.3 |
| like homosexuality | 182 | 38.9 |
| Immune suppression | 173 | 37 |
| Early age at first sexual intercourse HIV/AIDS | 158 | 33.6 |
| Smoking | 99 | 21.2 |
* Multiple responses observed
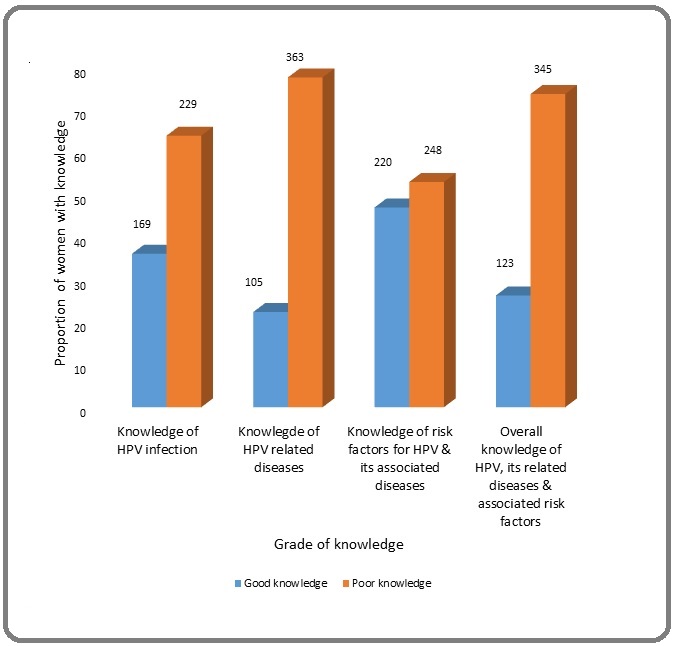
The most commonly identified risk factors for HPV infection and related diseases were having multiple sexual partners [229/468 (48.9%)], having partners with multiple sexual partners [224/468 (47.9%)], and presence of other STIs [193/468 (41.2%)]. The knowledge level of the participants were below average with a larger proportion of women having poor level of knowledge on different aspects of HPV and its associated diseases. The mean score for knowledge of HPV infection and HPV related diseases were 2.5±2.2 (range 0-8) and 3.5±3.3 (range 0-12) respectively while the mean score for knowledge of risk factors for HPV infection and its diseases was 3.2±2.6 (range 0-8). Only 36.1% (169/468), 22.4% (105/468) and 47.0% (220/468) of women had good knowledge of HPV infection, HPV related diseases, and risks factors for HPV and its diseases respectively. Participants were more knowledgeable about risk factors for HPV and its diseases than the infection itself or the diseases it causes. In total, the overall knowledge of HPV infection and its related diseases was low with a mean score of 9.2±7.3 (range 0-28). Approximately one quarter [123/468 (26.3%)] of women had overall good level of knowledge of HPV and its diseases (Figure 1).
Figure 1. Level of Knowledge of HPV Infection, Its Related Diseases and Associated Risk Factors.
The most common primary source of information about HPV and its associated diseases was healthcare professionals (HCP) [164/468 (35.0%)], followed by electronic media [55/468 (11.8%)] and organized programs such like health awareness programs and workshops [28/468 (6.0%)]. Religious bodies contributed the least information on HPV and its diseases while more than half [239/468 (51.1%)] had no source of information (Figure 2).
Figure 2. Sources of Information & Knowledge about HPV Infection and Its Related Diseases.
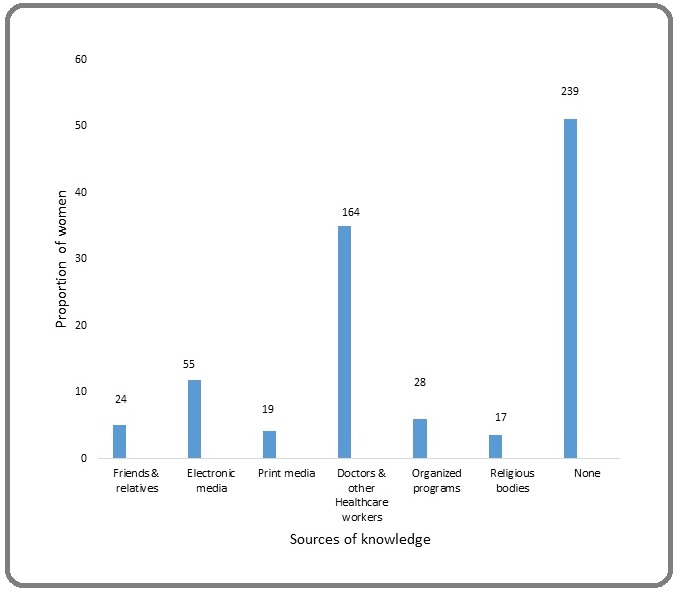
Table 3 shows the factors that influenced the overall knowledge of HPV infection and its associated diseases. Level of education, occupational status and parity were significantly associated with level of knowledge about HPV & its diseases (P <0.001, 0.033 & 0.001). Women with good knowledge of HPV infection and its related diseases had significantly better level of education, higher occupational status and lower parity compared to women with poor knowledge.
| Variable | Level of knowledge (n = 468) | P value | |
| Good (%) | Poor (%) | ||
| n = 123 | n = 345 | ||
| Age (in years) | 0.085 ¥ | ||
| < 21 | 11 (8.9) | 6.2 (5.2) | |
| 21 – 30 | 40 (32.5) | 80 (23.2) | |
| 31 – 40 | 48 (39.0) | 143 (41.4) | |
| 41 – 50 | 20 (16.3) | 78 (22.6) | |
| 51 – 60 | 3 (2.4) | 18 (5.2) | |
| > 60 | 1 (0.8) | 8 (2.3) | |
| Marital status | 0.166 £ | ||
| Married | 80 (65.0) | 248 (71.9) | |
| Single | 36 (29.3) | 75 (21.7) | |
| Others | 7 (5.7) | 22 (6.4) | |
| Highest level of education | <0.001 ¥ | ||
| No formal education | 2 (1.6) | 14 (4.1) | |
| Primary | 1 (0.8) | 11 (3.2) | |
| Secondary | 15 (12.2) | 108 (31.3) | |
| Tertiary | 105 (85.4) | 212 (61.4) | |
| Occupational status | 0.033 ¥ | ||
| Professional | 7 (5.7) | 11 (3.2) | |
| Skilled | 74 (60.2) | 170 (49.3) | |
| Semi-skilled | 21 (17.1) | 108 (31.3) | |
| Unskilled | 1 (0.8) | 4 (1.2) | |
| Unemployed | 20 (16.3) | 52 (15.1) | |
| Religion | 0.581 ¥ | ||
| Christianity | 104 (84.6) | 288 (83.5) | |
| Islam | 19 (15.4) | 53 (15.4) | |
| Traditional | 0 (0.0) | 4 (1.2) | |
| Tribe | 0.656 ¥ | ||
| Yoruba | 72 (58.5) | 190 (55.1) | |
| Igbo | 32 (26.0) | 109 (31.6) | |
| Hausa | 2 (1.6) | 7 (2.0) | |
| Others# | 17 (13.8) | 39 (11.3) | |
| Parity | 0.001 ¥ | ||
| 0 | 55 (44.7) | 121 (35.1) | |
| 1 – 4 | 64 (52.0) | 168 (48.7) | |
| >4 | 4 (3.3) | 56 (16.2) | |
| Source of knowledge Friends/relatives | |||
| Yes | 8 (6.5) | 16 (4.6) | 0.420 £ |
| No | 115 (93.5) | 329 (95.4) | |
| Electronic media | 0.001 £ | ||
| Yes | 25 (20.3) | 30 (8.7) | |
| No | 98 (79.7) | 315 (91.3) | |
| Print media | <0.011 £ | ||
| Yes | 10 (8.1) | 9 (2.6) | |
| No | 113 (91.9) | 336 (97.4) | |
| Doctors & Healthcare workers | <0.001 £ | ||
| Yes | 64 (52.0) | 100 (29.0) | |
| No | 59 (48.0) | 245 (71.0) | |
| Organized programs | <0.001 £ | ||
| Yes | 18 (14.6) | 10 (2.9) | |
| No | 105 (85.4) | 335 (97.1) | |
| Religious bodies | 0.087 ¥ | ||
| Yes | 1 (0.8) | 16 (4.6) | |
| No | 122 (99.2) | 329 (95.4) |
* Divorced, separated, cohabiting, # Tiv, Ijaw, Urhobo, Fulani, Edo, Egun, ¥ Fisher exact Chi square, £ Pearson Chi square
There was also a significant association between the level of knowledge and sources of information. Sources of information such as electronic media, print media, HCP and organized programs were significantly associated with women having good level of knowledge of HPV and its related diseases (P=0.001, 0.011, <0.001 and <0.001 respectively). A significant proportion of women with good knowledge obtained their information on HPV from these sources compared to those with poor knowledge. HPV information obtained from friends /relatives and religious bodies did not significantly contribute to good knowledge (P=0.420 & 0.087 respectively).
Table 4 shows the univariable and multivariable predictors of knowledge of HPV infection and its associated diseases. On univariable analysis, age below 35 years [crude odd ratio (COR)=1.94, CI=1.28–2.95, P=0.002), tertiary education (COR=3.66, C1=2.12-6.33, P<0.001), having skilled occupation (COR=1.75, CI=1.14-2.68, P=0.010) and low parity (COR=5.78, CI=2.04-16.13, P<0.001) were significantly associated with increased odds of having good knowledge of HPV infection and its diseases. In addition, information from electronic media (COR=2.68, CI=1.50- 4.76, P=0.001), print media (COR=3.30, CI=1.31-8.33, P=0.008), HCP (COR=2.70, CI=1.74-4.07, P<0.001) and organized program (COR=5.75, CI=2.57-12.82, P<0.001) significantly increased the likelihood of having good knowledge about HPV & its diseases.
| Variables | Univariate predictors | Multivariate predictors | ||||
| Crude Odds ratio | P value | 95% Confidence Interval | Adjusted Odds ratio | P value | 95% Confidence Interval | |
| Age | ||||||
| ≥ 35 | 1 | 1 | ||||
| < 35 | 1.94 | 0.002 | 1.28 - 2.95 | 1.57 | 0.091 | 0.93 - 2.65 |
| Tribe | ||||||
| Others | 1 | - | ||||
| Yoruba | 1.15 | 0.506 | 0.76 - 1.75 | - | - | - |
| Marital status | ||||||
| Others | 1 | 1 | ||||
| Married | 0.73 | 0.155 | 0.47 - 1.13 | 0.78 | 0.379 | 0.45 - 1.35 |
| Religion | ||||||
| Others | 1 | - | ||||
| Christianity | 1.08 | 0.781 | 0.62 - 1.91 | - | - | - |
| Educational status | ||||||
| Secondary education & below | 1 | 1 | ||||
| Tertiary education | 3.66 | < 0.001 | 2.12 – 6.33 | 2.4 | 0.005 | 1.30 - 4.44 |
| Occupation | ||||||
| Semi-skilled & below | 1 | 1 | ||||
| Skilled & above | 1.75 | 0.01 | 1.14 – 2.68 | 1.21 | 0.479 | 0.71 - 2.06 |
| Parity | ||||||
| > 4 | 1 | 1 | ||||
| ≤ 4 | 5.78 | < 0.001 | 2.04 – 16.13 | 4.22 | 0.011 | 1.40 - 12.66 |
| Knowledge from friends & relatives | ||||||
| No | 1 | - | ||||
| Yes | 1.43 | 0.42 | 0.60 – 3.44 | - | - | - |
| Knowledge from electronic media | ||||||
| No | 1 | 1 | ||||
| Yes | 2.68 | 0.001 | 1.50 – 4.76 | 6.06 | <0.001 | 2.86 - 12.99 |
| Knowledge from print media | ||||||
| No | 1 | 1 | ||||
| Yes | 3.3 | 0.008 | 1.31– 8.33 | 4 | 0.023 | 1.21 - 13.16 |
| Knowledge from HCW | ||||||
| No | 1 | 1 | ||||
| Yes | 2.7 | <0.001 | 1.74 – 4.07 | 6.3 | <0.001 | 3.56 - 11.11 |
| Knowledge from organized programs | ||||||
| No | 1 | 1 | ||||
| Yes | 5.75 | <0.001 | 2.57 – 12.82 | 13.16 | <0.001 | 5.08 - 34.48 |
| Knowledge from religious bodies | ||||||
| No | 1 | 1 | ||||
| Yes | 0.17 | 0.087 | 0.02-1.29 | 0.6 | 0.64 | 0.07 - 5.13 |
However, after controlling for all significant factors on multivariable regression analysis, only tertiary education [adjusted odd ratio (AOR)=2.40, CI=1.30-4.44, P=0.005], low parity (AOR=4.22, CI=1.40-12.66, P=0.011), obtaining information from electronic media (AOR=6.06, CI=2.86- 12.9, P<0.001), print media (AOR=4.00, CI=1.21-13.16, P=0.023), HCP (AOR=6.30, CI=3.56-11.11, P<0.001) and organized program (COR=13.16, CI=5.08-34.48, P<0.001) remained independent predictors of good knowledge of HPV and its related diseases.
Discussion
Public awareness and knowledge about a disease and its etiological agent is critical to the successful implementation of any public health intervention that relates to disease prevention [19]. Our study aimed to assess women’s knowledge about HPV infection and its related diseases and to predict the factors that influence their knowledge. We found that approximately a quarter of women (26.3%) had good knowledge about HPV infections and its related diseases, with HCP, electronic media and organized health programs being the most common sources of information on HPV and its diseases. Level of education, occupational status, parity and source of information were significantly associated with participants’ level of knowledge about HPV and its diseases. However, only tertiary level of education, low parity, obtaining knowledge through electronic media, print media, HCP and organized health program significantly predicted good knowledge of HPV and its related diseases.
It is worrisome that most women in our environment had poor knowledge about HPV and its diseases despite the huge burden of the infection and its diseases among women in Sub-Saharan Africa [2-4][8,9]. This is consistent with findings in other studies in Nigeria [14-18], Africa [23-28] and LMIC [29-30] where the burden of HPV related diseases are high. The study also found that less than a quarter of women (21.4%) believed that they were at risk of having HPV infection while less than a third (29.5% & 28.0%) knew that CC and GW were associated with HPV infection respectively. This finding represents one of the reasons why the burden of HPV related diseases especially cervical CC has remained high in our environment. This wrong perception and poor knowledge can act as barrier to the acceptability and uptake of evidence based targeted interventions such as HPV vaccination and testing as these women may not consider them beneficial and needful.
The present study shows that majority of women are ignorant of the ubiquity of HPV infection, its potential to infect both males & females, to cause malignant and non-malignant diseases and the types of diseases it causes. Consequently, there is urgent need for government and stakeholders to invest in aggressive and sustained public health awareness and education about HPV and its related diseases to address these gaps in knowledge in order to enhance acceptability and uptake of HPV based preventive measures. These educational campaign should be carried out through appropriate and effective channels. Our study found that HCP, electronic media (television, radio, and internet) and organized programs such as health awareness programs, workshops, seminars, etc were the common sources of information and knowledge on HPV and its diseases among the study participants. This is congruent to findings in similar studies [14] [16] [22] [25] where HCP, electronic media and organized health programs accounted for at least two of the leading sources of knowledge. This is however contrary to findings by Bhuiyan et al (2018) [30] and Wong and Sam (2010) [31] where print media and friends/family were the leading sources of information. In addition, obtaining information through these channels including print media, significantly predicted good knowledge of HPV & its diseases. This is contrary to finding in another study [25]. Organized programs had the highest impact on knowledge with the likelihood of having good knowledge being thirteen times higher among women whose source of information was organized programs compared to those whose sources were different. This was followed by HCP and electronic media which were associated with a six fold increase in the likelihood of having good knowledge respectively. Several studies [22][32-36] had reported on the positive impact HCP had on health awareness, health seeking behaviour and uptake of health interventions. HCP are valuable agents for dissemination of health information and preventive health practices due to the public perception and trust bestowed on them as credible sources on health issues. Similarly, mass media has been shown to be an essential tool for information and knowledge dissemination about HPV, its related disease and preventive measures [31] [37]. These channels of health communication and knowledge dissemination allow for interaction between the communicator or educator and audience and provides for feedbacks to assess the effectiveness of the communication and education process.
Furthermore, our study showed that parity was a significant independent predictor of good knowledge of HPV and its diseases. Women with low parity had a four- fold increase in the likelihood of having good knowledge compared to women with high parity. Even though Roik et al (2017) [33] also found a significant association between parity and knowledge, this relationship did not significantly predict knowledge. Education was the only socio-demographic factor that independently predicted good knowledge of HPV and its related diseases. Having a tertiary level of education significantly increased the likelihood of having good knowledge by more than two folds. This is comparable to findings in other studies [22] [33-35] [38] where high educational status was a significant determinant of good health awareness, behaviour and practice while Bhuiyan et al (2018) [30] reported a contrary finding. Most people with high educational status tend to have better quality of health [39]. This complex relationship between education and health is indirectly mediated by factors such as economic, social and behavioural variables which are directly influenced by education [38][40].
A limitation of this study is its generalizability. Being a hospital based study, the findings of this study may not be representative of the general population. A more representative population based study is recommended to confirm the findings of the study.
In conclusion, knowledge of HPV infection and its related diseases was very low among the study participants with only a quarter of the participants having good level of knowledge. Tertiary education, low parity and having electronic media, print media, HCP and organized health programs as primary sources of information were the significant predictors of good knowledge of HPV infection & its diseases. There is need for increased health awareness campaign through these identified information channels to bridge the gap in women’s knowledge and improve public knowledge about HPV and its related diseases in our environment.
Acknowledgements
The authors thank all those who contributed to the success of the study.
References
- Genital HPV infection Centers for Disease Control and Prevention . STD fact sheet.2021.
- Epidemiology and Burden of Human Papillomavirus and Related Diseases, Molecular Pathogenesis, and Vaccine Evaluation Kombe Kombe Arnaud John, Li Bofeng, Zahid Ayesha, Mengist Hylemariam Mihiretie, Bounda Guy-Armel, Zhou Ying, Jin Tengchuan. Frontiers in Public Health.2020;8. CrossRef
- Human papillomavirus vaccines World Health Organization . WHO position paper. Wkly Epidemiol Rec.2017;:241-68.
- Global burden of human papillomavirus and related diseases Forman D, de Martel C, Lacey CJ, Soerjomataram I, Lortet-Tieulent J, Bruni L, Vignat J, Ferlay J, Bray F, Plummer M, Franceschi S. Vaccine.2012;30 Suppl 5. CrossRef
- Human papillomavirus vaccines: WHO position paper, May 2017-Recommendations Vaccine.2017;35(43). CrossRef
- Human papillomavirus (HPV) and cervical cancer. . World Health Organization . Retrieved from https://www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer.Accessed on 22 August 2021.2020.
- Human papillomavirus and related diseases in Nigeria. Summary report. ICO/IARC information centre on HPV and cancer (HPV Information Centre) Bruni L, Albero G, Serrano B, Mena M, Collado JJ, Gómez D, Muñoz J, Bosch FX, de Sanjosé S. Retrieved from https://hpvcentre.net/statistics/reports/NGA.pdf. Accessed 22.2021.
- Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries Sung H, Ferlay J, Siegel Rl, Laversanne M, Soerjomataram I, Jemal A, Bray F. CA: a cancer journal for clinicians.2021;71(3). CrossRef
- Nigeria GLOBOCAN 2020 fact sheet. The Global Cancer Observatory. IARC/WHO . Retrieved from chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/viewer.html?pdfurl=https%3A%2F%2Fgco.iarc.fr%2Ftoday%2Fdata%2Ffactsheets%2Fpopulations%2F566-nigeria-fact-sheets.pdf&clen=267163&chunk=true. Accessed on 22 August 2021.2021.
- Practice Bulletin No. 168: Cervical Cancer Screening and Prevention Obstetrics and gynecology.2016;128(4). CrossRef
- Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study de Sanjose S, Quint WG, Alemany L, Geraets DT, Klaustermeier JE, Lloveras B, Tous S, Felix A, Bravo LE, Shin HR, Vallejos CS, de Ruiz PA, Lima MA, Guimera N, Clavero O, Alejo M, Llombart-Bosch A, Cheng-Yang C, Tatti SA, Kasamatsu E, Iljazovic E, Odida M, Prado R, Seoud M, Grce M, Usubutun A, Jain A, Suarez GA, Lombardi LE, Banjo A, Menéndez C, Domingo EJ, Velasco J, Nessa A, Chichareon SC, Qiao YI, Lerma E, Garland SM, Sasagawa T, Ferrera A, Hammouda D, Mariani L, Pelayo A, Steiner I, Oliva E, Meijer CJ, Al-Jassar WF, Cruz E, Wright TC, Puras A, Llave Cl, Tzardi M, Agorastos T, Garcia-Barriola V, Clavel C, Ordi J, Andújar M, Castellsagué X, Sánchez GI, Nowakowski AM, Bornstein J, Muñoz N, Bosch FX. The Lancet. Oncology.2010;11(11). CrossRef
- Cervical Cancer Screening Programs in Europe: The Transition Towards HPV Vaccination and Population-Based HPV Testing Chrysostomou AC, Stylianou DC, Constantinidou A, Kostrikis LG. Viruses.2018;10(12). CrossRef
- Public Knowledge of Human Papillomavirus and Receipt of Vaccination Recommendations Suk R, Montealegre JR, Nemutlu GS, Nyitray AG, Schmeler KM, Sonawane K, Deshmukh AA. JAMA pediatrics.2019;173(11). CrossRef
- Human papillomavirus (HPV) infection and vaccines: knowledge, attitude and perception among female students at the University of Lagos, Lagos, Nigeria Makwe CC, Anorlu RI, Odeyemi KA. Journal of epidemiology and global health.2012;2(4). CrossRef
- Knowledge of Human Papilloma Virus (HPV) and its Vaccine Among Female Undergraduates in Awka, South Eastern Nigeria Ezebialu CU, Ezebialu IU, Ezeifeka GO, Nwobu RUA, Unegbu VN, Eze EM, Ezenyeaku CC. International Journal of Medicine and Public Health.2018;8. CrossRef
- Knowledge, attitude and practice of cervical cancer prevention, among women residing in an urban slum in Lagos, South West, Nigeria Olubodun Tope, Odukoya Oluwakemi Ololade, Balogun Mobolanle Rasheedat. The Pan African Medical Journal.2019;32. CrossRef
- Awareness and uptake of human papilloma virus vaccines among female secondary school students in Benin City, Nigeria Ezeanochie M, Olasimbo P. African health sciences.2020;20(1). CrossRef
- Increasing Human Papillomavirus Vaccination and Cervical Cancer Screening in Nigeria: An Assessment of Community-Based Educational Interventions Nkwonta Chigozie Anastacia, Hilfinger Messias DeAnne K., Felder Tisha, Luchok Kathryn. International Quarterly of Community Health Education.2020;41(1). CrossRef
- Knowledge matters and empowers: HPV vaccine advocacy among HPV-related cancer survivors Shelal Zeena, Cho Dalnim, Urbauer Diana L., Lu Qian, Ma Bridgette Y., Rohrer Anna M., Kurian Shiney, Sturgis Erich M., Ramondetta Lois M.. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer.2020;28(5). CrossRef
- How to calculate sample size for different study designs in medical research? Charan J, Biswas T. Indian journal of psychological medicine.2013;35(2). CrossRef
- Cervical Cancer and Human Papilloma Virus Knowledge and Acceptance of Vaccination among Medical Students in Southwest Nigeria Adejuyigbe FF, Balogun MR, Sekoni AO, Adegbola AA. Afr J Reprod Health.2015;19:140-8.
- Women's Knowledge on Ovarian Cancer Symptoms and Risk Factors in Nigeria: An Institutional-based Study Okunowo Adeyemi Adebola, Adaramoye Victoria Olawunmi. Journal of Epidemiology and Global Health.2018;8(1-2). CrossRef
- Knowledge of HPV among HIV-Infected and HIV-Uninfected Adolescent Women in South Africa Griffith DC, Adler D, Wallace M, Bennie T, Abar B, Bekker LG. Journal of women's health, issues & care.2015;4(5). CrossRef
- Tanzanian women´s knowledge about Cervical Cancer and HPV and their prevalence of positive VIA cervical screening results. Data from a Prevention and Awareness Campaign in Northern Tanzania, 2017 - 2019 Henke A, Kluge U, Borde T, Mchome B, Serventi F, Henke O. Global health action.2021;14(1). CrossRef
- Knowledge and Awareness of Cervical Cancer and Human Papillomavirus among Female Students in an Ethiopian University: A Cross-sectional Study Tesfaye ZT, Bhagavathula AS, Gebreyohannes EA, Tegegn HG. International journal of preventive medicine.2019;10. CrossRef
- A cross-sectional study to assess HPV knowledge and HPV vaccine acceptability in Mali Poole DN, Tracy JK, Levitz L, Rochas M, Sangare K, Yekta S, Tounkara K, Aboubacar B, Koita O, Lurie M, De Groot AS. PloS one.2013;8(2). CrossRef
- Human papillomavirus (HPV) awareness and vaccine receptivity among Senegalese adolescents Massey PM, Boansi RK, Gipson JD, Adams RM, Riess H, Dieng T, Prelip MI, Glik DC. Tropical medicine & international health : TM & IH.2017;22(1). CrossRef
- Knowledge and awareness of HPV vaccine and acceptability to vaccinate in sub-Saharan Africa: a systematic review Perlman S, Wamai RG, Bain PA, Welty T, Welty E, Ogembo JG. PloS one.2014;9(3). CrossRef
- Knowledge and awareness about human papillomavirus infection and its vaccination among women in Arab communities Alsous Mervat M., Ali Ahlam A., Al-Azzam Sayer I., Abdel Jalil Mariam H., Al-Obaidi Hala J., Al-Abbadi Esraa I., Hussain Zainab K., Jirjees Feras J.. Scientific Reports.2021;11(1). CrossRef
- Knowledge and Acceptance of Human Papillomavirus Vaccine for Cervical Cancer Prevention Among Urban Professional Women in Bangladesh: A Mixed Method Study Bhuiyan Afsana, Sultana Farhana, Islam Jessica Yasmine, Chowdhury Mohiuddin Ahsanul Kabir, Nahar Quamrun. BioResearch Open Access.2018;7(1). CrossRef
- Ethnically diverse female university students' knowledge and attitudes toward human papillomavirus (HPV), HPV vaccination and cervical cancer Wong Li Ping, Sam I.-Ching. European Journal of Obstetrics, Gynecology, and Reproductive Biology.2010;148(1). CrossRef
- Provider communication and HPV vaccination: The impact of recommendation quality Gilkey MB, Calo WA, Moss JI, Shah PD, Marciniak MW, Brewer NT. Vaccine.2016;34(9). CrossRef
- Knowledge about human papillomavirus and prevention of cervical cancer among women of Arkhangelsk, Northwest Russia Roik EE, Sharashova EE, Nieboer E, Kharkova OA, Postoev VA, Odland JØ. PloS one.2017;12(12). CrossRef
- Women's knowledge of cervical cancer and uptake of Pap smear testing and the factors influencing it in a Nigerian tertiary hospital Okunowo AA, Daramola ES, Soibi-Harry AP, et al . J Cancer Res Pract.2018;5:105-11.
- Beliefs About HPV Vaccine's Success at Cervical Cancer Prevention Among Adult US Women Fokom Domgue J, Chido-Amajuoyi OG, Yu RK, Shete S. JNCI cancer spectrum.2019;3(4). CrossRef
- Cervical cancer screening among urban Women in Lagos, Nigeria: Focus on barriers and motivators for screening Okunowo AA, Smith-Okonu ST. Niger J Gen Pract.2020;18:10-6.
- Change in knowledge of women about cervix cancer, human papilloma virus (HPV) and HPV vaccination due to introduction of HPV vaccines Donders Gilbert G. G., Bellen Gert, Declerq Ann, Berger Judith, Van Den Bosch Thierry, Riphagen Ine, Verjans Marcel. European Journal of Obstetrics, Gynecology, and Reproductive Biology.2009;145(1). CrossRef
- Predictors of Adults' Knowledge and Awareness of HPV, HPV-Associated Cancers, and the HPV Vaccine: Implications for Health Education McBride Kimberly R., Singh Shipra. Health Education & Behavior: The Official Publication of the Society for Public Health Education.2018;45(1). CrossRef
- The influence of education on health: an empirical assessment of OECD countries for the period 1995-2015 Raghupathi V, Raghupathi W. Archives of public health = Archives belges de sante publique.2020;78. CrossRef
- The Relationship Between Education and Health: Reducing Disparities Through a Contextual Approach Zajacova A, Lawrence EM. Annual review of public health.2018;39. CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times