Optimum Radiation Fractionation Schedule in Advanced Cancer Cervix; A Study from Low Resource North Indian Cancer Center
Download
Abstract
Introduction: Cervical cancer is the fourth most commonly occurring lethal cancer among women worldwide. The primary curative treatment option for women suffering from locally advanced cervical cancer includes external beam radiotherapy (EBRT) with concurrent weekly platinum-based radiosensitizing chemotherapy and brachytherapy (BT) to obtain finest treatment outcomes.
Aim: The purpose of this study is to assess tumor response following HDRBT preceded by EBRT and to identify optimum radiation fractionation schedule for better response with tolerable radiation toxicity.
Material and methods: 91 patients diagnosed with carcinoma of uterine cervix were screened for inclusion in the study. Patients were categorized according to FIGO Staging system The patient was put in lithotomy position and given anesthesia and fletcher suit applicator was applied to the patient push the bladder and rectum and finally shifted to the HDR treatment unit. All the associations were tested by using chi square test.
Results: In our study it was found that majority (44%) of the cases were aged 51-60 years. Vaginal bleeding and squamous cell carcinoma was found in most of the cases. The acute radiation toxicities were more in elderly age group and the association was found to be statistically significant (p<0.05) except Genitourinary – cystitis. Age group 51-60 years was significantly associated with response (p=0.034) with lower risk of partial response (OR=0.31 (0.10-0.95), while the symptom Backache/Pain in abdomen had significantly higher risk of partial response (p=0.002, OR=16.24 (1.7-154.8).
Conclusion: When compared to traditional techniques, HDR can achieve very high rates of local control while lowering morbidity.
Introduction
Cervical cancer is the fourth most commonly occurring lethal cancer among women worldwide [1]. Statistical data fetched from Indian reports suggests that India itself accounts for one-fourth of the global burden of cervical cancer [2]. It has been observed that in India it accounts for 17% of cancer deaths among women during their reproductive age group [1].
Patients presenting with small volume stage IB1 and IIA disease according to International Federation of Gynecologists and Obstetricians (FIGO) can be provided treatment either by radical hysterectomy and lymphadenectomy or radical radiotherapy as prime procedures. The two methods have equivalent survival rates (Level 1b) [3, 4]. The combination of surgery and radiotherapy escalates morbidity and should be avoided if possible [5]. Local control and survival are improved by the inclusion of concomitant chemotherapy in all stages, though the benefit may be lesser when only one node is positive or when the tumour size is <2 centimetres (cm) (Level 1b) [5, 6]. Overall treatment time should not exceed 56 days, including intracavitary brachytherapy (ICBT), for squamous carcinoma (Level 1b) [7, 8]. Hemoglobin levels during treatment aid in prognosis, with the best results in those subjects with hemoglobin greater than 12 grams per deciliter (g/dl) throughout treatment (Level 2b) [9].
The primary curative treatment option for women suffering from locally advanced cervical cancer includes external beam radiotherapy (EBRT) with concurrent weekly platinum-based radiosensitizing chemotherapy and brachytherapy (BT) to obtain finest treatment outcomes [10]. BT enables for dose escalation of the tumour and acts as cornerstone thereby minimizing the toxicity of nearby organs at-risk (OARs). Through multiple past clinical reports it was concluded that BT plays an essential role in the curative treatment paradigm, as it confers both local control and survival advantage when compared to cohorts who were treated through EBRT alone as a radiation treatment modality [11, 12].
BT, being a highly conformal form of radiation technique, allows delivery of high doses to the tumour, and is the cornerstone for optimal clinical outcomes and toxicities.
Various guidelines have been established for the treatment of cervical cancer which also includes brachytherapy [13, 14]. However; these guidelines are chiefly designed and applicable for the western world and are of limited value in low and middle-income countries (LMICs) including India. Furthermore, LMICs have an exclusive ethnic and cultural background, disease patterns, health care systems and access to treatment facilities [15]. The treatment practices are commonly influenced by regional variances in cultural and socioeconomic factors, resources availability and expertise, knowledge and technology improvements etc., resulting in extremely heterogeneous patterns of care [16, 17]. The majority of the centers in India, currently, practice high-dose-rate (HDR) brachytherapy for cervical cancers [18].
The dose distribution will be manually calculated by changing relative dwell time values before an appropriate solution is reached, computer being used only to measure the dose distribution after the dosimetrist has agreed on the method. This method, or its combination with traditional optimization algorithms like geometrical or dose point optimization, necessitates time and expertise. It’s necessary to distinguish between a planning method that optimizes doses based on anatomic structures and optimized planning systems that optimize doses based on the position of active dwells or a few other dose points. The final step toward fully anatomy-based conformal dose preparation is to use an anatomy-based optimization. The purpose of this study is to assess tumor response following HDRBT preceded by EBRT and to identify optimum radiation fractionation schedule for better response with tolerable radiation toxicity.
Materials and Methods
This study was conducted in patients attending outpatient department of radiotherapy at North Indian hospital. 91 patients diagnosed with carcinoma of uterine cervix were screened for inclusion in the study. All patients underwent complete evaluation by history taking, gynaecological examination and systemic examination. Certain symptoms such as vaginal bleeding and discharge, pain in lower abdomen, backache difficulty in micturition and defecation etc. were also noted. All patients underwent complete evaluation by history taking, gynaecological examination and systemic examination. Malignancy was histologically proven through biopsy in all patients. Complete blood count, liver function tests, renal function tests, chest radiograph and, ultrasound abdomen and pelvis were some of the examinations carried out for all patients. CECT abdomen and pelvis or MRI pelvis was also done. Patients were categorized according to the stages on the basis of FIGO Staging system [5]. Ethical clearance was obtained from institutional ethical committee prior to the study. Written informed consent was taken from the patients before start of treatment (Table 1).
| Inclusion criteria | Exclusion criteria |
| Histo-pathologically confirmed carcinoma of uterine cervix cases. | Patients with any kind of pelvic infection, fibroid, ascites and other concurrent systemic illness. |
| FIGO stage IIA, IIB (bulky), IIIB | Pregnant women or lactating mothers |
| Karnofsky score >0 | |
| Patients who has given approved informed consent |
Treatment Allocation
All enrolled patients in this study after histopathological confirmation carcinoma; surface marking was done on the pelvis of the patients for teletherapy usually 15 X 15 field size and treated by APPA fields by the Telecobalt unit. Those patients who had separation of more than 20 cm were treated by four-field box technique. Two orthogonal X-rays pelvis and/ or CT assisted scanogram and slices and plato treatment planning system was utilized. After the completion of the external beam RT, the patients were evaluated for regression of tumor and given symptomatic treatment if required. Procedure was done under strict aseptic conditions under conscious sedation. The patient was put in lithotomy position and examined without anaesthesia for reassessment. The part was prepared followed by short anaesthesia ketamine). An assessment of fornices was done to decide upon the size of ovoids to be used whether half, small, medium and large.
The length of the uterus was assessed with uterine sound. The treatment was done for uterine length from 4 cm to 6 cm. Then the fletcher suit applicator was applied to the patient and adequate packing was done with gauge or placement of tungsten retractor to push the bladder and rectum. The patient was shifted to the HDR treatment unit where the catheters were connected and individualized treatment was received by the microselection afterloading system.
Treatment protocol
Combined external beam therapy and high dose brachy therapy in stages IIA,IIB and IIIB, IB>3 cm.
EBRT-ICRT
External beam therapy was followed for intracavitory high dose rate HDR micro-selection application at a gap of 2-3 weeks after completion of external beam radiotherapy Cases of cancer uterine cervix randomly received 4600cG in 23fractions, 45000cG in 20 fractions and 5000cG in 25 fractions preceded by ICRT. HDR dose- 800 cGy at point a repeated after 1 week ie; 2 fractions of HDR application with dose at point A being 800 cGy in each. None of the patients were given chemotherapy and all the cases were untreated prior to the study period. External beam therapy was delivered by theratron 780 C cobalt teletherapy unit and ICRT by HDR microselector after loading system using Ir 192 as the radioactive source.
Follow up
The patients were studied according to age, presenting complaints, clinical manifestation, histology, haemoglobin and treatment response acute radiation reactions. The patients were followed first after 2 weeks; 4 weeks and then 8 week till the completion of study period.
Statistical analysis
The results were analyzed using descriptive statistics and making comparisons among various groups. Categorical data were summarized as proportions and percentages (%) while discrete (quantitative) as mean (SD). All the associations were tested by using chi square test. Logistic regression analysis was performed for making model of treatment response outcome with general & clinical Profile of Patients. Statistical analyses were performed using SPSS version 23.0 (SPSS Inc., Chicago, IL, USA). A value of p<0.05 was considered statistically significant.
Results
General & Clinical Profile of Patients
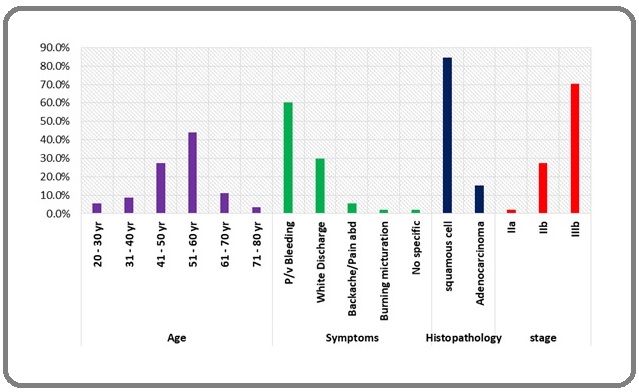
Majority (44%) of the cases were aged 51-60 years, most common symptoms was P/v bleeding (60.4%) followed by white discharge (29.7%). Other symptoms were Backache/Pain in abdomen (5.5%), burning micturition (2.2%) while in 2.2% cases it was non-specific. According to histopathology squamous cell carcinoma was found in majority 84.6% cases while in remaining 15.4% cases adenocarcinoma was observed. IIIb was the most common stage as found in 70.3% cases, while stage IIa and IIb was found in 2.2% and 27.5% cases respectively (Table 2) (Figure 1).
| Variable | Total | ||
| No. | % | ||
| Age | 20 - 30 yr | 5 | 5.5 |
| 31 - 40 yr | 8 | 8.8 | |
| 41 - 50 yr | 25 | 27.5 | |
| 51 - 60 yr | 40 | 44 | |
| 61 - 70 yr | 10 | 11 | |
| 71 - 80 yr | 3 | 3.3 | |
| Symptoms | P/v Bleeding | 55 | 60.4 |
| White Discharge | 27 | 29.7 | |
| Backache/Pain in abdomen | 5 | 5.5 | |
| Burning micturation | 2 | 2.2 | |
| No specific | 2 | 2.2 | |
| Histopathology | squamous cell | 77 | 84.6 |
| Adenocarcinoma | 14 | 15.4 | |
| stage | IIa | 2 | 2.2 |
| IIb | 25 | 27.5 | |
| IIIb | 64 | 70.3 |
Figure 1. General & Clinical Profile of Patients.
Association of Treatment Response with General & Clinical Profile of Patients
The analysis to find any association of treatment response with General & Clinical Profile of Patients (Table 3) revealed that the age group 51-60 years was significantly associated with response (p=0.034) with lower risk of partial response (OR=0.31 (0.10-0.95), while the symptom Backache/Pain in abdomen had significantly higher risk of partial response (p=0.002, OR=16.24 (1.7-154.8).
| Variable | CR (N=70) | PR (N=21) | chi sq | p-value | OR (95% CI) | |||
| No. | % | No. | % | |||||
| Age | 20 - 30 yr | 4 | 5.7 | 1 | 4.8 | 0.03 | 0.867 | 0.82 (0.09-7.81) |
| 31 - 40 yr | 4 | 5.7 | 4 | 19 | 3.58 | 0.058 | 3.88 (0.88-17.14) | |
| 41 - 50 yr | 19 | 27.1 | 6 | 28.6 | 0.02 | 0.898 | 1.07 (0.36-3.17) | |
| 51 - 60 yr | 35 | 50 | 5 | 23.8 | 4.5 | 0.034 | 0.31 (0.10-0.95) | |
| 61 - 70 yr | 6 | 8.6 | 4 | 19 | 1.81 | 0.178 | 2.51 (0.64-9.91) | |
| 71 - 80 yr | 2 | 2.9 | 1 | 4.8 | 0.18 | 0.668 | 1.70 (0.15-19.73) | |
| Symptoms | P/v Bleeding | 42 | 60 | 13 | 61.9 | 0.03 | 0.876 | 1.08 (0.40-2.95) |
| White Discharge | 23 | 32.9 | 4 | 19 | 1.48 | 0.224 | 0.48 (0.15-1.59) | |
| Backache/Pain in abdomen | 1 | 1.4 | 4 | 19 | 9.66 | 0.002 | 16.24 (1.70-154.76) | |
| Burning micturation | 2 | 2.9 | 0 | 0 | 0.61 | 0.433 | NA | |
| No specific | 2 | 2.9 | 0 | 0 | 0.61 | 0.433 | NA | |
| Histo-pathology | squamous cell | 63 | 90 | 14 | 66.7 | 6.76 | 0.009 | 0.22 (0.07-0.74) |
| Adenocarcinoma | 7 | 10 | 7 | 33.3 | 6.76 | 0.009 | 4.50 (1.36-14.90) | |
| stage | IIa | 2 | 2.9 | 0 | 0 | 0.61 | 0.433 | NA |
| IIb | 24 | 34.3 | 1 | 4.8 | 7.07 | 0.008 | 0.10 (0.01-0.76) | |
| IIIb | 44 | 62.9 | 20 | 95.2 | 8.12 | 0.004 | 11.82 (1.50-93.29) |
By histopathology squamous cell carcinoma had significantly lower risk of partial response (p=0.009, OR=0.22 (0.07-0.74)) compared to adenocarcinoma (p=0.009, OR=4.50 (1.36-14.90)).
Among stages, IIb had significantly lower risk of partial response (p=0.008, OR=0.10 (0.01-0.76)) while IIIb had significantly higher risk of partial response (p=0.004, OR=11.82 (1.50-93.29)).
Logistic Regression Analysis to Find Relationship of Treatment Response Outcome with General & Clinical Profile of Patients
The Logistic Regression Analysis to find relationship of treatment response outcome with general & clinical Profile of Patients (Table 4) revealed minimum risk of partial response or maximum chances of complete response are those which have minimum beta coefficient in the category of the study variable which in this case was corresponding to age group 51-60 yr, complaints of burning micturition, squamous cell type and lower stage (IIa).
| Variable | B | S.E. | Sig. | Exp(B) |
| Age | 0.386 | |||
| 20 - 30 yr | -18.05 | 22248.8 | 0.999 | 1.45E-08 |
| 31 - 40 yr | -16.09 | 22248.8 | 0.999 | 1.03E-07 |
| 41 - 50 yr | -17.49 | 22248.8 | 0.999 | 2.52E-08 |
| 51 - 60 yr | -18.51 | 22248.8 | 0.999 | 9.12E-09 |
| 61 - 70 yr | -17.66 | 22248.8 | 0.999 | 2.14E-08 |
| 71 - 80 yr | 0 | |||
| Complaints | 0.673 | |||
| P/v Bleeding | 33.51 | 32311.98 | 0.999 | 3.56E+14 |
| White Discharge | 33.27 | 32311.98 | 0.999 | 2.80E+14 |
| Backache/ | 36.27 | 32311.98 | 0.999 | 5.62E+15 |
| Pain in abdomen | ||||
| Burning micturation | 15.47 | 44518.77 | 1 | 5.25E+06 |
| No specific | 0 | |||
| Squamous cell | -1.32 | 0.84 | 0.117 | 0.266 |
| Adenocarcinoma | 0 | |||
| Stage | 0.149 | |||
| IIa | -19.83 | 36276.52 | 1 | 2.44E-09 |
| IIb | -2.65 | 1.18 | 0.024 | 0.07 |
| IIIb | 0 | |||
| Constant | -15.26 | 23431.92 | 0.999 | 0 |
Association of Toxicities with Age
The acute radiation toxicities were more in elderly age group and the association was found to be statistically significant (p<0.05) except Genitourinary – cystitis. However complaint, Histopath and stage did not show significant association with acute radiation toxicities except moist desquamation with complaint which was seen more in Backache/Pain in abdomen and No specific (p<0.001). (Table 5A, 5B, 5C, 5D) Confluent mucositis was seen more in proportion among partial response cases compared to complete response (2.9% vs 14.3%, p=0.044) (Table 6).
| Toxicities | Total | 20 - 30 yr (N=5) | 31 - 40 yr (N=8) | 41 - 50 yr (N=25) | 51 - 60 yr (N=40) | 61 - 70 yr (N=10) | 71 - 80 yr (N=3) | chi sq | p-value | |||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | |||
| Skin – Moist disquamation | 3 | 3.3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 30 | 0 | 0 | 25.1 | <0.001 |
| Ulceration | 5 | 5.5 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 5 | 3 | 30 | 0 | 0 | 14 | 0.016 |
| Confluent mucositis | 5 | 5.5 | 0 | 0 | 0 | 0 | 5 | 20 | 0 | 0 | 0 | 0 | 0 | 0 | 14 | 0.016 |
| Diarrhoea | 47 | 51.6 | 2 | 40 | 2 | 25 | 3 | 12 | 29 | 72.5 | 8 | 80 | 3 | 100 | 31.3 | <0.001 |
| Enteritis/ Proctitis | 28 | 30.8 | 0 | 0 | 1 | 12.5 | 1 | 4 | 18 | 45 | 6 | 60 | 2 | 66.7 | 21.5 | 0.001 |
| Genitourinary - cystitis | 3 | 3.3 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2.5 | 2 | 20 | 0 | 0 | 10.2 | 0.069 |
| Toxicities | Complaints | chi sq | p-value | |||||||||
| P/v Bleeding | White Discharge | Backache/ Pain in abdomen | Burning micturation | No specific | ||||||||
| N | % | N | % | N | % | N | % | N | % | |||
| Skin - moist desquamation | 0 | 0 | 0 | 0 | 2 | 40 | 0 | 0 | 1 | 50 | 37.68 | <0.001 |
| Ulceration | 1 | 1.8 | 3 | 11.1 | 1 | 20 | 0 | 0 | 0 | 0 | 5.33 | 0.255 |
| Confluent mucositis | 5 | 9.1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3.46 | 0.484 |
| Diarrhoea | 23 | 41.8 | 16 | 59.3 | 4 | 80 | 2 | 100 | 2 | 100 | 8.11 | 0.088 |
| Enteritis/Proctitis | 12 | 21.8 | 10 | 37 | 4 | 80 | 1 | 50 | 1 | 50 | 8.95 | 0.062 |
| Genitourinary - cystitis | 1 | 1.8 | 1 | 3.7 | 1 | 20 | 0 | 0 | 0 | 0 | 4.9 | 0.297 |
| Toxicities | Histopathology | chi sq | p-value | |||
| Squamous cell | Adenocarcinoma | |||||
| N | % | N | % | |||
| Skin - moist disquamation | 2 | 2.6 | 1 | 7.1 | 0.77 | 0.381 |
| Ulceration | 4 | 5.2 | 1 | 7.1 | 0.09 | 0.769 |
| Confluent mucositis | 5 | 6.5 | 0 | 0 | 0.96 | 0.327 |
| Diarrhoea | 39 | 50.6 | 8 | 57.1 | 0.2 | 0.655 |
| Enteritis/Proctitis | 23 | 29.9 | 5 | 35.7 | 0.19 | 0.663 |
| Genitourinary - cystitis | 2 | 2.6 | 1 | 7.1 | 0.77 | 0.381 |
| Toxicities | Stage | chi sq | p-value | ||||||||
| IIa | IIb | IIIb | |||||||||
| N | % | N | % | N | % | ||||||
| Skin - moist disquamation | 0 | 0.00 | 0 | 0.00 | 3 | 4.70 | 1.31 | 0.52 | |||
| Ulceration | 0 | 0.00 | 0 | 0.00 | 5 | 7.80 | 2.23 | 0.328 | |||
| Confluent mucositis | 0 | 0.00 | 1 | 4.00 | 4 | 6.30 | 0.29 | 0.863 | |||
| Diarrhoea | 1 | 50.00 | 9 | 36.00 | 37 | 57.80 | 3.43 | 0.18 | |||
| Enteritis/Proctitis | 0 | 0.00 | 8 | 32.00 | 20 | 31.30 | 0.91 | 0.633 | |||
| Genitourinary - cystitis | 0 | 0.00 | 0 | 0.00 | 3 | 4.70 | 1.31 | 0.52 |
| Toxicities | Response | chi sq | p-value | |||||
| CR | PR | |||||||
| N | % | N | % | |||||
| Skin - moist disquamation | 1 | 1.40 | 2 | 9.50 | 3.32 | 0.068 | ||
| Ulceration | 3 | 4.30 | 2 | 9.50 | 0.85 | 0.356 | ||
| Confluent mucositis | 2 | 2.90 | 3 | 14.30 | 4.06 | 0.044 | ||
| Diarrhoea | 35 | 50.00 | 12 | 57.10 | 0.33 | 0.566 | ||
| Enteritis/Proctitis | 21 | 30.00 | 7 | 33.30 | 0.08 | 0.772 | ||
| Genitourinary - cystitis | 2 | 2.90 | 1 | 4.80 | 0.18 | 0.668 |
Discussion
By virtue of HDR brachytherapy, high dose of radiation can be given in a shorter period of time (outpatient department) which reduces patient discomfort and inconvenience. Regardless of its practical benefits, HDR brachytherapy has experienced significant resistance because of worries regarding its possible toxicity and theoretical radiobiologic disadvantage as HDR involves a greater probability of late effects for a given level of tumor control. Certain crucial factors that aid in lowering the frequency of complications without compromising the treatment results are fractionation and dose adjustment of total dose.
In our study it was found that majority (44%) of the cases were aged 51-60 years. According to Globocan reports In India the peak age for cervical cancer incidence is 55–59 years [19]. The major symptoms that were discovered included P/v bleeding (60.4%) followed by white discharge (29.7%). Other symptoms were Backache/ Pain in abdomen (5.5%), burning micturition (2.2%) while in 2.2% cases it was non-specific. P/v bleeding and white discharge have been the common symptoms of cervical carcinoma according to Shah et al and Nganwai et al however the percentage is contradictory to our results 86.9 and 77.7 % menstrual abnormality and 94.2% and 92.4% abnormal vaginal discharge respectively [20, 21].
According to histopathology squamous cell carcinoma was found in majority 84.6% cases while in remaining 15.4% cases adenocarcinoma was observed. IIIb was the most common stage as found in 70.3% cases, while stage IIa and IIb was found in 2.2% and 27.5% cases respectively. Histopathological analysis done by Bhandari et al revealed that 92.5 % were Squamous cell carcinoma (SCC), and 7.5 % were Adenocarcinoma which were again not concomitant with our results. However our results were consistent with his study in terms of stages as he also found that the common stage was 67 % IIIB followed by 11.1 % in stage IVA, 9.8 % in stage IIB, 8.5 % in IIA, and 3.5 % in stage IB [22].
Our results revealed that revealed that the age group 51-60 years was significantly associated with response (p=0.034) with lower risk of partial response (OR=0.31 (0.10-0.95), while the symptom Backache/ Pain in abdomen had significantly higher risk of partial response (p=0.002, OR=16.24 (1.7-154.8). However the results were consistent with the outcomes attained by Saibishkumar et al. revealed that age > 50 y was linked with higher rates of no residual tumor [15] while Rahakbauw et al found no statistical relationship [23]. By histopathology squamous cell carcinoma had significantly lower risk of partial response (p=0.009, OR=0.22 (0.07-0.74)) compared to adenocarcinoma (p=0.009, OR=4.50 (1.36-14.90)). Similar study done by Fletcher et al. revealed that the squamous cell carcinoma group responded similarly to those with non-squamous cell carcinoma. Among stages, IIb had significantly lower risk of partial response (p=0.008, OR=0.10 (0.01-0.76)) while IIIb had significantly higher risk of partial response (p=0.004, OR=11.82 (1.50-93.29)) [24].
The Logistic Regression Analysis to find relationship of treatment response outcome with general & clinical profile of patients revealed minimum risk of partial response or maximum chances of complete response are those which have minimum beta coefficient in the category of the study variable which in this case was corresponding to age group 51-60 year, complaints of Burning micturition, squamous cell type, lower stage (IIa) and Hb level more than 10 mg/dl. Similar results were found by Rahakbauw et al which revealed that 26–50-year-olds tended to exhibit decreased response, by 0.87 times, compared to those older than age 50 [23].
The acute radiation toxicities were more in elderly age group and the association was found to be statistically significant (p<0.05) except Genitourinary – cystitis. However complaint, Histopath and stage did not show significant association with acute radiation toxicities except moist desquamation with complaint which was seen more in Backache/Pain in abdomen. No specific (p<0.001) Confluent mucositis was seen more in proportion among partial response cases compared to complete response (2.9% vs 14.3%, p=0.044).Consistently, Kunos [25] and Laurentius et al [26], also found higher haematological toxicity in elderly patients.
In conclusion, recent advances have been incorporated in brachytherapy for cervical cancer which allow for better demarcation and coverage of the tumor, as well as improved avoidance of OARs. As a result, when compared to traditional techniques, HDR can achieve very high rates of local control while lowering morbidity. This article gives a summary of a small effort in defining an optimum radiation schedule in Indian patients who present advanced stages and when there is heavy patient load. Taking into account of increased hospital burden of locally advanced cancer cervix patients in Indian context, increase in sample size and extending the follow-up duration may produce more reliable results.
References
- Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis Arbyn Marc, Weiderpass Elisabete, Bruni Laia, Sanjosé Silvia, Saraiya Mona, Ferlay Jacques, Bray Freddie. The Lancet. Global Health.2020;8(2). CrossRef
- Burden of cervical cancer and role of screening in India Bobdey Saurabh, Sathwara Jignasa, Jain Aanchal, Balasubramaniam Ganesh. Indian Journal of Medical and Paediatric Oncology: Official Journal of Indian Society of Medical & Paediatric Oncology.2016;37(4). CrossRef
- Combined chemotherapy and radiotherapy compared with radiotherapy alone in patients with cancer of the esophagus A Herskovic, K Martz, M al-Sarraf, L Leichman, J Brindle, V Vaitkevicius, J Cooper, R Byhardt, L Davis, B Emami. The New England journal of medicine.1992;326(24). CrossRef
- INT 0123 (Radiation Therapy Oncology Group 94-05) phase III trial of combined-modality therapy for esophageal cancer: high-dose versus standard-dose radiation therapy Minsky Bruce D., Pajak Thomas F., Ginsberg Robert J., Pisansky Thomas M., Martenson James, Komaki Ritsuko, Okawara Gordon, Rosenthal Seth A., Kelsen David P.. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2002;20(5). CrossRef
- Definitive chemoradiotherapy for oesophageal cancer -- a promising start on an exciting journey Rackley T., Leong T., Foo M., Crosby T.. Clinical Oncology (Royal College of Radiologists (Great Britain)).2014;26(9). CrossRef
- National Comprehensive Cancer Network, NCCN Clinical Practice Guidelines in Oncology: Cervical Cancer v1.2016 [cited 2016 September 19]; Available from: http://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf..
- Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer Cunningham David, Allum William H., Stenning Sally P., Thompson Jeremy N., Van de Velde Cornelis J. H., Nicolson Marianne, Scarffe J. Howard, Lofts Fiona J., Falk Stephen J., Iveson Timothy J., Smith David B., Langley Ruth E., Verma Monica, Weeden Simon, Chua Yu Jo, MAGIC Trial Participants null. The New England Journal of Medicine.2006;355(1). CrossRef
- Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction Macdonald J. S., Smalley S. R., Benedetti J., Hundahl S. A., Estes N. C., Stemmermann G. N., Haller D. G., Ajani J. A., Gunderson L. L., Jessup J. M., Martenson J. A.. The New England Journal of Medicine.2001;345(10). CrossRef
- Role of (chemo)-radiotherapy in resectable gastric cancer Foo M., Crosby T., Rackley T., Leong T.. Clinical Oncology (Royal College of Radiologists (Great Britain)).2014;26(9). CrossRef
- Curative radiation therapy for locally advanced cervical cancer: brachytherapy is NOT optional Tanderup Kari, Eifel Patricia J., Yashar Catheryn M., Pötter Richard, Grigsby Perry W.. International Journal of Radiation Oncology, Biology, Physics.2014;88(3). CrossRef
- Trends in the utilization of brachytherapy in cervical cancer in the United States Han Kathy, Milosevic Michael, Fyles Anthony, Pintilie Melania, Viswanathan Akila N.. International Journal of Radiation Oncology, Biology, Physics.2013;87(1). CrossRef
- American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part I: general principles Viswanathan Akila N., Thomadsen Bruce. Brachytherapy.2012;11(1). CrossRef
- The European Society of Gynaecological Oncology/European Society for Radiotherapy and Oncology/European Society of Pathology guidelines for the management of patients with cervical cancer Cibula David, Pötter Richard, Planchamp François, Avall-Lundqvist Elisabeth, Fischerova Daniela, Haie Meder Christine, Köhler Christhardt, Landoni Fabio, Lax Sigurd, Lindegaard Jacob Christian, Mahantshetty Umesh, Mathevet Patrice, McCluggage W. Glenn, McCormack Mary, Naik Raj, Nout Remi, Pignata Sandro, Ponce Jordi, Querleu Denis, Raspagliesi Francesco, Rodolakis Alexandros, Tamussino Karl, Wimberger Pauline, Raspollini Maria Rosaria. Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2018;127(3). CrossRef
- Radiation Oncology in India: Challenges and Opportunities Grover Surbhi, Gudi Shivakumar, Gandhi Ajeet Kumar, Puri Priya M., Olson Adam C., Rodin Danielle, Balogun Onyi, Dhillon Preet K., Sharma Daya Nand, Rath Goura Kishor, Shrivastava Shyam Kishore, Viswanathan Akila N., Mahantshetty Umesh. Seminars in Radiation Oncology.2017;27(2). CrossRef
- Treatment and outcome in cancer cervix patients treated between 1979 and 1994: a single institutional experience S Shrivastava, U Mahantshetty, R Engineer, H Tongaonkar, J Kulkarni, K Dinshaw. Journal of cancer research and therapeutics.2013;9(4). CrossRef
- Concurrent Chemoradiation for Cancer of the Cervix: Results of a Multi-Institutional Study From the Setting of a Developing Country (India) Nandakumar Ambakumar, Kishor Rath Goura, Chandra Kataki Amal, Poonamalle Bapsy P., Gupta Prakash C., Gangadharan Paleth, Mahajan Ramesh C., Nath Bandyopadhyay Manas, Kumaraswamy null, Vallikad Elizabeth, Visweswara Rudrapatna N., Selvaraj Roselind Francis, Sathishkumar Krishnan, Daniel Vijaykumar Dampilla, Jain Ankush, Lakshminarayana Sudarshan Kondalli. Journal of Global Oncology.2015;1(1). CrossRef
- Brachytherapy in India – a long road ahead Banerjee Susovan, Mahantshetty Umesh, Shrivastava Shyamkishore. Journal of Contemporary Brachytherapy.2014;6(3). CrossRef
- World – both sexes estimated incidence by age Available from: http://www.globocan.iarc.fr/old/age_specific_table_r.asp?..
- Awareness and knowledge of cervical cancer and its prevention among the nursing staff of a tertiary health institute in Ahmedabad, Gujarat, India Shah V., Vyas S., Singh A., Shrivastava M.. Ecancermedicalscience.2012;6. CrossRef
- Nganwai P, Truadpon P, Inpa C, Sangpetngam B, Mekjarasnapa M et al (2008) Knowledge, attitudes and practices vis-a-vis cervical cancer among registered nurses at the Faculty of Medicine, Khon Kaen University, Thailand Asian Pac J Cancer Prev 9 15–18 .
- Unusual Metastasis from Carcinoma Cervix Bhandari Virendra, Kausar Mehlam, Naik Ayush, Batra Manika. Journal of Obstetrics and Gynaecology of India.2016;66(5). CrossRef
- Prognostic value of response to external radiation in stage IIIB cancer cervix in predicting clinical outcomes: a retrospective analysis of 556 patients from India Saibishkumar Elantholi P., Patel Firuza D., Sharma Suresh C., Karunanidhi Gunaseelan, Ghoshal Sushmita, Kumar Vinay, Kapoor Rakesh. Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2006;79(2). CrossRef
- Radiotherapy response and related clinicopathological factors of patients with cervical cancer Rahakbauw E, Winarto H. Journal of Physics: Conference Series.2018;1073. CrossRef
- Fletcher G H 1971 Cancer of the uterine cervix Janeway Lecture, 1970 Am. J. Roentgenol. Rad...
- Retrospective analysis of concomitant Cisplatin during radiation in patients aged 55 years or older for treatment of advanced cervical cancer: a gynecologic oncology group study Kunos Charles, Tian Chunqiao, Waggoner Steven, Rose Peter G., Lanciano Rachelle. International Journal of Gynecological Cancer: Official Journal of the International Gynecological Cancer Society.2009;19(7). CrossRef
- Impact of age on morbidity and outcome of concurrent radiochemotherapy in high-risk FIGO stage I to IVA carcinoma of the uterine cervix following laparoscopic surgery Laurentius Thea, Altendorf-Hofmann Annelore, Camara Oumar, Runnebaum Ingo B., Wendt Thomas G.. Journal of Cancer Research and Clinical Oncology.2011;137(3). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times