The Prognostic Significance of Hydronephrosis and Role of Ureteric Stenting in Cervical Cancer Patients Treated with Radical Radiation Therapy, Real World Outcomes from a Regional Cancer Centre, South India
Download
Abstract
Background: The incidence of renal failure in carcinoma cervix ranges from 14% to 44·2%. The interventional strategies like ureteric stenting and percutaneous nephrostomy can be considered to improve renal function. The primary objective of our study is to analyze the impact of hydroureteronephrosis [HUN] in the outcome of cervical cancer patients treated with radical radiation. The secondary objective is to analyze the role of ureteric stenting to protect the renal function while proceeding with radical radiation.
Methods: In this retrospective study, all patients with stage IIIB cervical cancer treated with radical radiation therapy at our institution from January 2010 to December 2019 were included.
Results: Among the total 483 stage IIIB patients, 146 patients [30·22%] had hydronephrosis.Thirty eight [26·02%] out of 146 patients with HUN underwent ureteric stenting. The five year overall survival [OS] was 61·4 ± 0·04 % and on subset analysis, overallsurvival was 65·7 ± 0·05 % for patients without HUN and 50·6 ± 0·06 % for patientswith HUN. [P value <0·001]. Among patients with hydronephrosis, those with bilateral hydronephrosis or serum creatinine >1·1 mg/dL have benefitted more from stenting. In this high risk subgroup, the one year overall survival was 65·2 ± 0·11 % and 42·4 ±0·13 % for patients with and without stenting. [p value 0·07]. No major stent related morbidity occurred.
Conclusions: Hydronephrosis in cervical cancer patients indicates bad prognosis which results in decreased survival. The presence of hydronephrosis should be redesignated as a separate substage, IIIB2 in future FIGO updates, for better prognostication and treatment recommendations. The relief of obstructive uropathy should be sought out inpatients with serum creatinine levels > 1·1 mg/dL or bilateral hydronephrosis before theinitiation of oncological treatment.
Introduction
The survival of cervical cancer patients decreases with increasing disease stage, despite the use of standard treatment protocols. The Federation International Obstetrics and Gynaecology [FIGO] stage IIIB is defined as tumor extending upto pelvic side wall and/or presence of hydronephrosis or a non functioning kidney [1]. The incidence of renal failure in carcinoma cervix ranges from 14% to 44·2% [2]. The interventional strategies like ureteric stenting and percutaneous nephrostomy can be considered to improve renal function. Despite these aggressive measures, cervical cancer patients with hydronephrosis have poor survival outcomes [3]. Renal failure and subsequent uremia is the most common cause of death in cervical cancer patients with hydronephrosis. Survival data regarding cervical cancer patients with hydronephrosis are under reported in the literature. In 1999 the National Cancer Institute issued a clinical alert stating that the addition of cisplatin based chemotherapy to radiation treatment improved the survival rate for locally advanced cervical cancers. The chemotherapeutic agent cisplatin is associated with nephrotoxicity and hence many patients with hydroureteronephrosis [HUN] and elevated serum creatinine levels are not fit for concurrent cisplatin along with radical radiation therapy. As a result of aggressive management of ureteric obstruction and treatment with radical radiation therapy often combined with chemotherapy, the outcome of these patients are marginally improved.
The natural progression of hydronephrosis during concurrent chemoradiation is not studied well. The clinical experience is that chemoradiation may precipitates renal failure in patients with bilateral hydronephrosis and sometimes even with unilateral hydronephrosis. Tumor progression, pelvic inflammation by radiation, acute renal injury by cisplatin are some of the various reasons for this progressive obstructive uropathy. Hence ureteric stenting before radiation treatment planning process has many potential benefits such as improvement of renal functional status, uninterrupted radiation therapy, better toleration of full dose cisplatin chemotherapy and safe intravenous contrast injection during computed tomography [CT] or magnetic resonance imaging [MRI]. Ureteric stenting also helps in identification, contouring and application of dose constraints to ureters during interstitial brachytherapy [4].
The primary objective of our study is to analyze the impact of hydroureteronephrosis in the outcome of cervical cancer patients treated with radical radiation. The secondary objective is to analyze the role of ureteric stenting to protect the renal function while proceeding with radical radiation.
Materials and Methods
In this retrospective study, all patients with stage IIIB cervical cancer treated with radical radiation therapy at our institution from January 2010 to December 2019 were included. Routine investigations included clinical examination, cervical punch biopsies, hemogram, renal function tests, liver function tests, chest X ray and ultrasonogram of abdomen and pelvis. Computed Tomography [CT] /Magnetic Resonance Imaging [MRI] of abdomen and pelvis with contrast was done as clinically indicated. Eligible patients were considered for radical radiation therapy along with concurrent weekly cisplatin. Patients with hydronephrosis or raised serum creatinine underwent ureteric stenting prior to radiation therapy. Percutaneous nephrostomy and anterograde stenting was done as an alternative strategy when retrograde stenting was not feasible
External beam radiation was delivered by either conventional or 3D conformal radiotherapy technique. Patients were treated with external beam radiation to pelvis, 45 to 50 Gy followed by 2- 3 cycles of High Dose Rate [HDR] intra cavitary application to deliver 16- 21 Gy to point A. If intracavitary application was not technically feasible, external radiation was continued with reduced fields upto 64 - 66 Gy. Total treatment duration was 7-8 weeks. The follow up schedule after treatment completion was every three months for initial three years, every six months up to five years and there after every year.
All data were collected after reviewing the records from Tumor registry department. The information regarding unilateral or bilateral hydronephrosis, serum creatinine values and stenting procedures were recorded. The details of radiation therapy and chemotherapy were also collected. Other data collected include date of disease progression and date of last follow up. Any major stent related complications were also documented. SPSS statistical software version 23·0 was used for data analysis. Kaplan Meier survival method with log rank test was used to analyze Progression Free survival [PFS] and Overall survival [OS]. The Cox Regression analysis was used to analyze all prognostic factors. A p value <0.05 is taken as significant.
Results
Among the total 483 stage IIIB patients, 146 patients [30·22%] had HUN. Out of the total HUN patients, 28 patients did not have parametrial involvement upto pelvic sidewall. They were staged as FIGO stage IIIB due to HUN alone. Fifteen patients had serum creatinine values more than 1·1 mg/dL and 25 patients had bilateral hydronephrosis. The patient characteristics are detailed in Table 1.
| Factor | No HUN [n=337] | HUN [n=146] |
| Mean Age | 56·48 ± 8·95 | 53·54 ± 8·99 |
| Histology | ||
| Squamous | 315 [93·5%] | 134 [91·8%] |
| Adeno | 13 [3·9%] | 8 [5·5%] |
| Adenosquamous | 7 [2·1%] | 4 [2·7%] |
| Neuroendocrine | 1 [0·5%] | 0 |
| Parametrium involvement upto pelvic wall | ||
| Nil | 0 | 28 [19·2%] |
| Bilateral | 74 [22%] | 36 [24·7%] |
| Unilateral | 263 [78%] | 82 [56·1%] |
| Pelvic nodes | ||
| Yes | 44 [13·1%] | 40 [27·4%] |
| No | 293 [86·1%] | 106 [72·6%] |
| HUN | ||
| Unilateral | 0 | 121 [82·8%] |
| Bilateral | 0 | 25 [17·2%] |
| S.Creatinine >1·1 | 0 | 15 [10·27%] |
Thirty eight [26·02%] out of 146 patients with HUN underwent ureteric stenting. Twenty six patients underwent bilateral ureteric stenting and remaining 12 patients underwent unilateral stenting. 461 [95·44%] patients received 45 to 50 Gy external beam radiation to pelvis followed by 2- 3 cycles of HDR intra cavitary application to deliver 16- 21 Gy to point A. In 20 patients [4·56%], intracavitary application was technically not feasible and external radiation was continued with reduced fields upto 64 - 66 Gy. Fifty six [38.35%] patients with HUN received weekly chemotherapy whereas 178 patients [52·8%] in the non-HUN group received weekly chemotherapy. Among 38 patients who underwent stenting, 20 patients received weekly cisplatin chemotherapy.
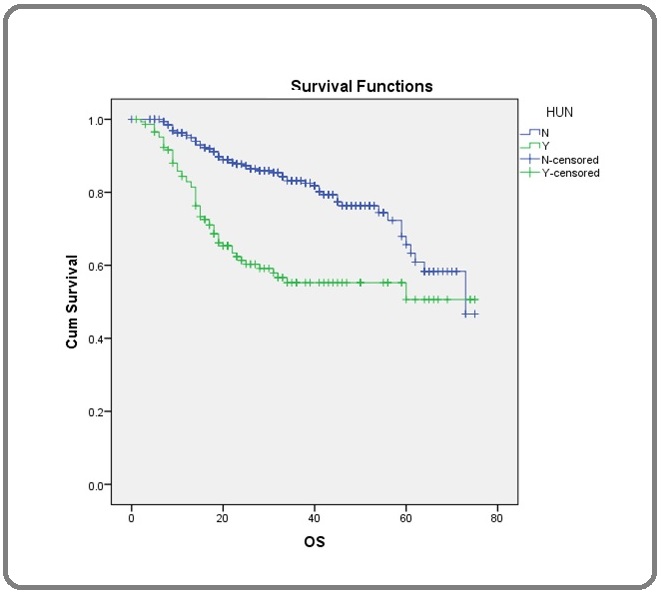
The median follow up time was 34 months. The five year overall survival [OS] was 61·4 ± 0·04 % and on subset analysis, the overall survival was 65·7 ± 0·05 % for patients without HUN and 50·6 ± 0·06 % for patients with HUN. [P value <0·001] (Figure 1).
Figure 1. Overall Survival of Patients with and without Hydroureteronephrosis. OS, Overall survival; HUN, Hydroureteronephrosis; N, No Hydroureteronephrosis; Y, Hydroureteronephrosis present.
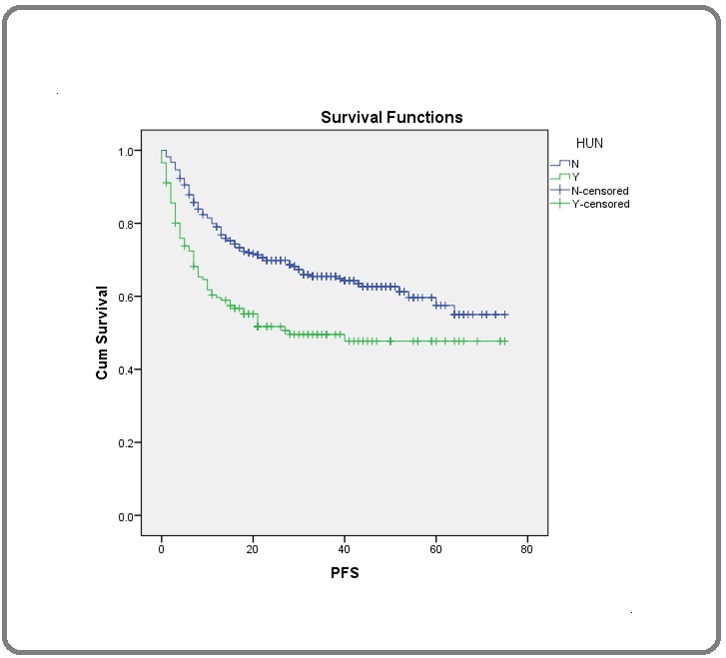
There was statistically significant difference in the progression free survival [PFS] too. The five year PFS was 57·5 ± 0·04 % in patients without HUN and 47·7 ± 0·04% in patients with HUN. [p value <0·001] (Figure 2).
Figure 2. Progression free Survival [PFS] of Patients with and without Hydroureteronephrosis [HUN]. PFS, Progression Free survival; HUN, Hydroureteronephrosis; N, No Hydroureteronephrosis; Y, Hydroureteronephrosis present.
Approximately 19·17% of patients with hydronephrosis didn’t have parametrial involvement upto pelvic side wall. The two year overall survival was 61·4 ± 0·04 % and 61·2 ± 0·09 % for patients with and without parametrial involvement respectively which was not statistically different (p value= 0·587). This again shows that irrespective of presence or absence of parametrial involvement upto pelvic wall, hydronephrosis indicate bad prognosis.
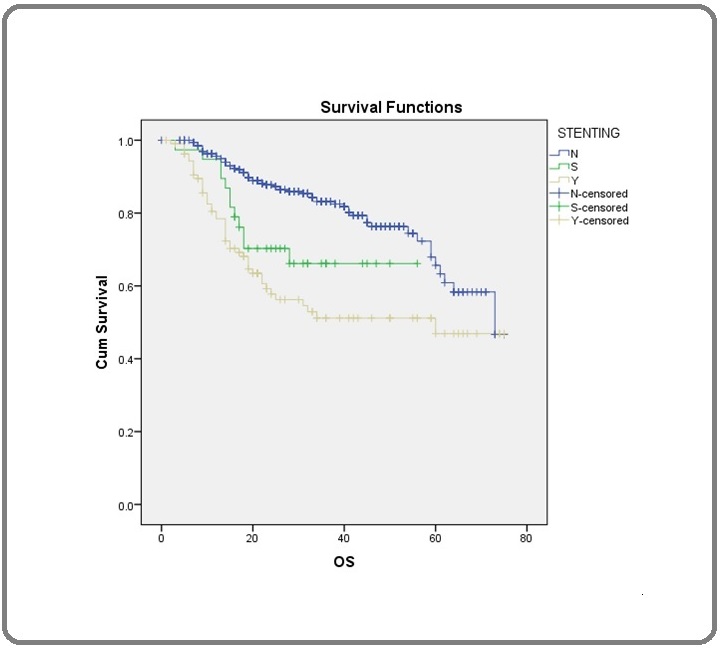
Among patients with hydronephrosis, those who underwent stenting had a mild increase in overall survival. The three year overall survival was 66·1 ± 0·08 % and 51·2 ± 0·05 % for patients with stenting and without stenting respectively [p value 0·168] (Figure 3 and 4).
Figure 3. Overall Survival of Hydronephrosis Patients with and without Stenting. OS, Overall survival; N, No Ureteric stenting; Y, Ureteric stenting.
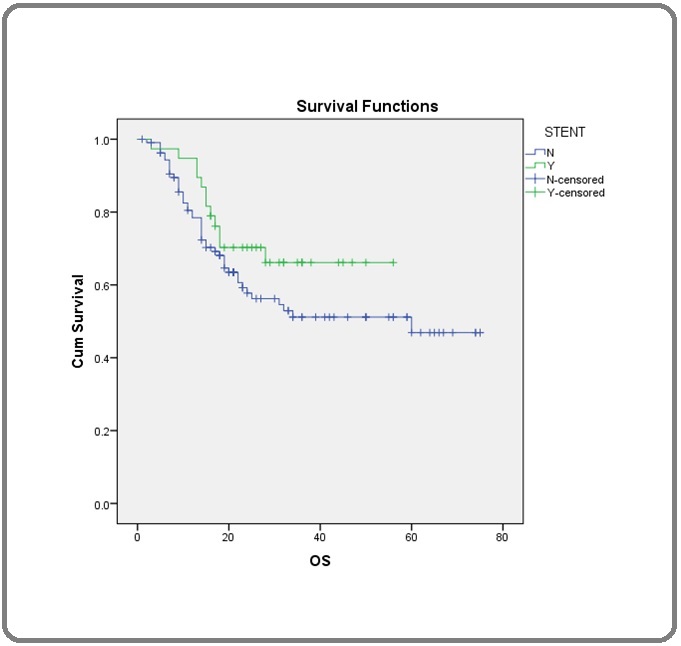
Figure 4. Overall Survival of Patients without Hydronephrosis, Hydronephrosis with Stenting and Hydronephrosis without Stenting. OS, Overall survival; N, No Hydroureteronephrosis; S, Hydroureteronephrosis present with stenting; Y, Hydroureteronephrosis present without stenting.
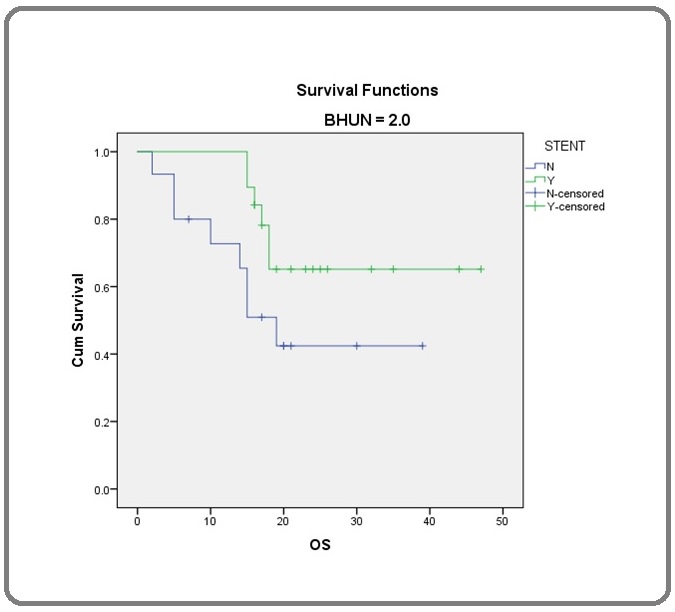
On subset analysis, patients with bilateral hydronephrosis or serum creatinine >1·1 mg/dL found to have benefitted more from stenting. The one year overall survival was 65·2 ± 0·11 % and 42·4 ± 0·13 % in hydronephrosis patients with and without stenting respectively with p value nearing significance. [p value 0·07] (Figure 5).
Figure 5. Overall Survival of Patients with Raised Serum Creatinine or Bilateral Hydronephrosis with and without Stenting. OS, Overall survival; Y, Hydroureteronephrosis present with stenting; N, Hydroureteronephrosis present without stenting.
No major stent related morbidity occurred in our retrospective study. The patients with hydronephrosis irrespective of the presence or absence of ureteric stent had frequent urinary tract infections which were managed with oral antibiotics after urine culture and sensitivity studies.
Univariate analysis was done for prognostic factors such as histology, node positive status, hydronephrosis and raised serum creatinine using Cox regression analysis. Among them adeno or adenosquamous histology, node positive status, hydronephrosis and raised serum creatinine [value > 1·1 mg/dL] emerged as significant unfavourable prognostic factors (Table 2).
| Factor | HR [95% CI] | P value |
| Histology [Adeno/Adenocarcinoma] | 2·04 [1·12 – 3·71] | P 0·019 |
| Pelvic Nodal status | 1·90 [1·25 – 2·90] | P 0·003 |
| Hydronephrosis | 2·54 [1·77 – 3·65] | P < 0·001 |
| Serum creatinine [value > 1·1 mg/dL] | 3·03 [1·47 – 6·24] | P 0·003 |
HR – Hazard Ratio
In multivariate analysis too, hydronephrosis emerged as an independent prognostic factor adjusting for histology, nodal status and raised serum creatinine levels with hazard ratio [HR] 2·19 [95% CI 1·49 – 3·21] [p value <0·001].
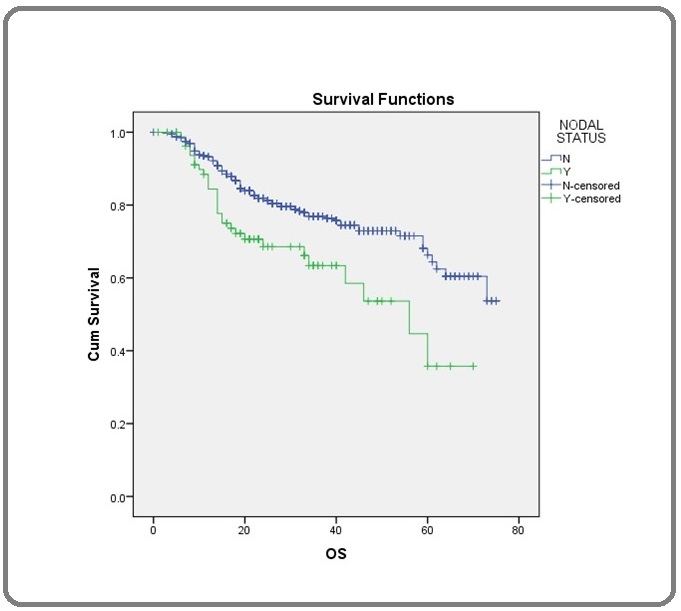
Among the unfavourable prognostic factors, pelvic node positive status results in a drop in overall survival worse than hydronephrosis. The five year overall survival was 35·8 ± 0·11 % and 66·3 ± 0·4% for patients with and without pelvic nodes respectively [p value 0·002] (Figure 6).
Figure 6. Overall Survival of Patients with and without Pelvic Nodes. OS, Overall survival; N, Pelvic Nodes absent; Y, Pelvic nodes present.
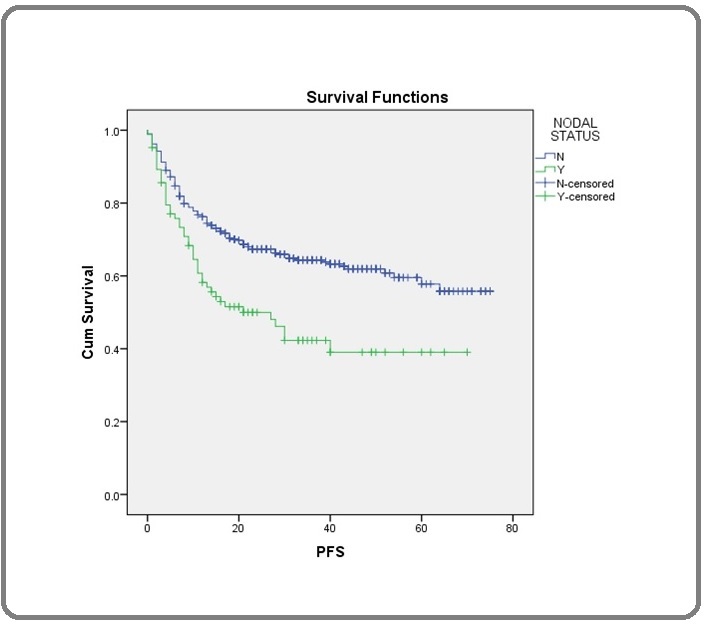
The difference in progression free survival was also statistically significant. The five year PFS was 57·8 ± 0·03% in patients without pelvic nodes whereas 39 ± 0·06 % in patients with pelvic nodes. [p value <0·001] (Figure 7).
Figure 7. Progression free Survival of Patients with and without Pelvic Nodes. PFS, Progression Free survival; N, Pelvic Nodes absent; Y, Pelvic nodes present.
Discussion
Indian subcontinent contributes a significant number of new cervical cancer cases across the globe and it accounts for nearly one third of global cervical cancer deaths [5]. Unfortunately data regarding the impact of hydronephrosis in stage IIIB cervical cancer patients is lacking in this region. There is an Indian study by Salunkhe et al.,(2020) [6] consisting of 125 patients, but it included advanced cervical cancer patients presenting with obstructive uropathy and raised serum creatinine levels requiring percutaneous nephrostomy only. This is a large retrospective study of stage IIIB cervical cancers from India which analyses the impact of hydronephrosis and role of ureteric stenting. Also the study was able to validate significant prognostic factors like histology, hydronephrosis, nodal status and raised serum creatinine levels. The survival rates in our study is higher than the general population data. The single institution data will be superior to population data in view of better selection of patients, individual patient tailored care, close monitoring of the patients during treatment and active follow up. Hence hospital based registries are mainly concerned with the outcome of patients treated in the institution with various interventions and treatment strategies.
One of the limitations of this study is the lack of CT or MR imaging for all patients. The major fallacy of FIGO clinical staging system is its subjective variations which can lead to upstaging or down staging of a patient. On pelvic examination, one clinician may find that a patient has parametrial involvement just short of pelvic side wall. The second clinician may find parametrial involvement upto pelvic side wall in the same patient. This would make the stage of the patient IIIB instead of IIB. In our study this inter examiner variation is kept minimum since there were only two examiners. More than 85 percentage of the study population was personally examined by the first author and confirmed the clinical staging. This very problem of inter observer variation in FIGO clinical staging system highlight the importance of an objective radiological prognostic factor like hydronephrosis.
The current 2019 FIGO staging update categorized cervical cancer patients with pelvic and para aortic nodes as stage IIIC1 &IIIC2 respectively. The previous FIGO staging didn’t have a separate staging for node positive patients. Hence in our study period [2014-2019] even though ultrasound imaging showed significant pelvic nodes, they were staged as IIIB only. If significant para aortic nodes were detected in ultrasound imaging they were staged as IVB during the study period based on previous FIGO staging and hence were not included in the study.
The poor survival of cervical cancer patients with hydronephrosis has been documented by various studies.
The Patel et al., (2015) [7] study from Mayo clinic tumor registry showed that hydronephrosis was associated with poor survival (hazard ratios ranged from 1·47 to 4·69). Pradhan et al., (2011) [8] also showed hydronephrosis is a poor prognostic factor. Our study also showed that the presence of hydronephrosis results in poor overall survival. Another interesting finding is that the survival for patients with hydronephrosis was relatively superior to those having positive nodes but inferior to those having parametrial involvement alone. Hence we believe that the presence of hydronephrosis should be redesignated as a separate substage, IIIB2 and patients with parametrial involvement upto pelvic side wall without hydronephrosis as IIIB1 in future FIGO updates, for better prognostication and treatment recommendations.
The obstructive uropathy should be relieved before the initiation of radiation treatment. This helps to prevent treatment breaks during radiotherapy and also helps to deliver concurrent chemotherapy with cisplatin. The most common cause of mortality in hydronephrosis patients is renal failure rather than advanced malignancy itself [9]. Thus ureteric stenting prevents or at least delay renal failure and can translate to modest increase in survival. Rose et al., (2010) [2] data showed that interventional procedures like stenting or percutaneous nephrostomy help to improve survival in cervical cancer patients with obstructive uropathy. Our study also proved this but due failed to achieve statistical significance due to retrospective nature of the study. This study included only those patients whose serum creatinine was improved after ureteral stenting or percutaneous nephrostomy and started on treatment. The patients who had elevated renal function even after intervention were not started on curative radiotherapy treatments and hence not included in this study.
It is a known fact that all patients with hydronephrosis will not require ureteric stenting. It is important to define a high risk subset of hydronephrosis patients who are prone for renal complications during concurrent chemoradiation and these high risk patients may benefit from elective ureteric stenting before the initiation of concurrent chemoradiation. In our study the improvement in survival was more predominant in a subset of cases with bilateral hydronephrosis or serum creatinine levels >1·1 mg/dL. Hence we recommend to consider ureteric stenting in this high risk patients with serum creatinine levels > 1·1 mg/dL or bilateral hydronephrosis.
In a study by Ku et al., (2004) [10] it was observed that ureteric stenting is associated with higher failure rates when compared to percutaneous nephrostomy. Therefore it is better to closely monitor patients with ureteric stents for any inadvertent incidences like slipping of the stent, kinking of the stent or stent block. The failure rate of ureteral stent placement is in the range of 16% to 58% [11,12]. In such cases percutaneous nephrostomy can be done and anterograde stenting through the PCN can be considered. It is difficult to distinguish the morbidity associated with hydronephrosis from stent related morbidity. The patients with ureteric stent may experience frequent urinary tract infections. These problems can be avoided by adequate hydration, frequent stent exchanges and proper antibiotic therapy. Stent exchange is frequently done through cystoscopic procedure since it is less invasive and is associated with less complications [13]. In our study we didn’t encounter any critical stent related complications except urinary tract infections which were treated with oral antibiotics.
To conclude, hydronephrosis in cervical cancer patients indicates bad prognosis which results in decreased survival. The presence of hydronephrosis should be redesignated as a separate substage, IIIB2 in future FIGO updates, for better prognostication and treatment recommendations. The relief of obstructive uropathy should be sought out in patients with serum creatinine levels > 1·1 mg/dL or bilateral hydronephrosis before initiation of oncological treatment. This helps to deliver radical radiation therapy often combined with chemotherapy without treatment breaks. Cystoscopic ureteric stenting is the preferred method and percutaneous nephrostomy and anterograde stenting can be considered as an alternative strategy. Adequate hydration, close monitoring of stent, frequent stent exchanges and proper antibiotic therapies should be considered to prevent any critical stent related complications. This risk stratification, prognostication and relief of obstructive uropathy is the initial step towards improving the survival of cervical cancer patients with hydronephrosis.
References
- Revised FIGO staging for carcinoma of the cervix uteri Bhatla N, Berek JS , Fredes MC , Denny LA , Grenman S, Karunaratne K, Kehoe ST , Konishi I, Olawaiye AB , Prat J, Sankaranarayanan R. International Journal of Gynecology & Obstetrics.2019;145(1):129-135. CrossRef
- Impact of hydronephrosis on outcome of stage IIIB cervical cancer patients with disease limited to the pelvis, treated with radiation and concurrent chemotherapy: a Gynecologic Oncology Group study Rose PG , Ali S, Whitney CW , Lanciano R, Stehman FB . Gynecologic oncology.2010;117(2). CrossRef
- Long-term outcome after radiotherapy for FIGO stage IIIB and IVA carcinoma of the cervix Yeung AR , Amdur RJ , Morris CG , Morgan LS , Mendenhall WM . International journal of radiation oncology, biology, physics.2007;67(5). CrossRef
- Ureteral stent insertion for gynecologic interstitial high-dose-rate brachytherapy Demanes DJ , Banerjee R, Cahan BI , Lee SP , Park SJ , Fallon JM , Reyes P, Van TQ , Steinberg MI , Kamrava MR . Brachytherapy.2015;14(2). CrossRef
- Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries Sung H, Ferlay J, Siegel RL , Laversanne M, Soerjomataram I, Jemal A, Bray F. CA: a cancer journal for clinicians.2021;71(3). CrossRef
- Outcomes of locally advanced cervical cancer presenting with obstructive uropathy: An institutional audit Salunkhe R, Chopra S, Kulkarni S, Shetty N, Engineer R, Mahantshetty U, Ghosh J, Gupta S, Shrivastava SK. Indian journal of cancer.2020;57(4). CrossRef
- Hydronephrosis in patients with cervical cancer: an assessment of morbidity and survival Patel Krishna, Foster Nathan R., Kumar Amanika, Grudem Megan, Longenbach Sherri, Bakkum-Gamez Jamie, Haddock Michael, Dowdy Sean, Jatoi Aminah. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer.2015;23(5). CrossRef
- Hydronephrosis as a prognostic indicator of survival in advanced cervix cancer Pradhan T S, Duan H, Katsoulakis E, et al . Int J Gynecol Cancer.2011;21:129-5.
- Pelvic radiotherapy in patients with hydronephrosis in stage IIIB cancer of the cervix: renal effects and the optimal timing for urinary diversion? G Horan, O McArdle, J Martin, Cd Collins, C Faul. Gynecologic oncology.2006;101(3). CrossRef
- Percutaneous nephrostomy versus indwelling ureteral stents in the management of extrinsic ureteral obstruction in advanced malignancies: are there differences? Ku Ja Hyeon, Lee Sang Wook, Jeon Hwang Gyun, Kim NHyeon Hoe, Oh Seung-June. Urology.2004;64(5). CrossRef
- The management of malignant ureteral obstruction treated with ureteral stents Ganatra AM , Loughlin KR . The Journal of urology.2005;174(6). CrossRef
- Malignant ureteral obstruction: outcomes after intervention. Have things changed? Wong LM , Cleeve LK , Milner AD , Pitman AG . The Journal of urology.2007;178(1). CrossRef
- Stent-change therapy in advanced malignancies with ureteral obstruction Rosenberg BH , Bianco Jr FJ , Wood Jr DP , Triest JA . Journal of endourology.2005;19(1). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times