Immunoglobulin G4-Related Disease of The Larynx Mimicking Malignancy: A Case Report and Review of the Literature
Download
Abstract
Immunoglobulin G4–related disease is characterized by increased serum immunoglobulin G4 level, enlargement in the relevant organs and histopathologically intense storiform fibrosis, lymphoplasmacytic infiltration rich in immunoglobulin G4 positive plasma cells, and obliterative phlebitis. In this report, a patient who underwent a laryngeal biopsy with a pre-diagnosis of malignancy, but had findings consistent with immunoglobulin G4–related disease in the biopsy sample, is described. Immunoglobulin G4–related disease can be seen in very rare localizations. It should be kept in mind in differential diagnosis when tissues especially containing inflammation rich in plasma cells are encountered. Clinical, laboratory and pathological correlation is extremely important in the diagnosis of an immunoglobulin G4-related disease.
Introduction
Immunoglobulin G4–related disease (IgG4-RD) is characterized by increased serum immunoglobulin G4 (IgG4) level, enlargement in the relevant organs and histopathologically intense storiform fibrosis, lymphoplasmacytic infiltration rich in IgG4 positive plasma cells, and obliterative phlebitis [1]. The etiopathogenesis of the IgG4-RD is uncertain. It was first reported in the pancreas in 2001 [2]. The IgG4-RD may infrequently involve a variety of head and neck sites primarily affecting the submandibular gland and less often seen in the thyroid gland, other salivary glands, lacrimal gland, sinonasal tract, oral cavity, orbit and lymph nodes [3]. Whereas, IgG4 RD cases identified in the larynx are very few [4-14].
In this case report, we present the probable IgG4-RD of the larynx that clinically mimics malignancy.
Case Report
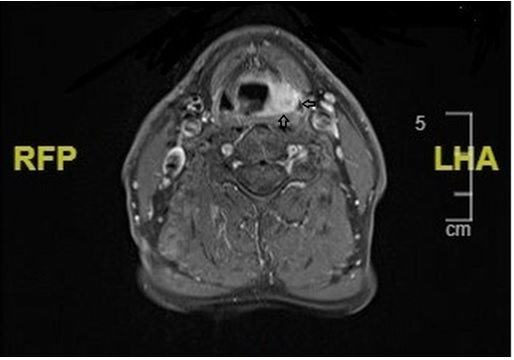
A 59-year-old male presented to the otolaryngology section with a 5-year history of hoarseness of voice. His medical history included hypertension and stroke. He had no other known disease or additional complaints. Complete blood count was normal. On neck magnetic resonance imaging revealed a lesion at the level of the supraglottic larynx, extending from the left aryepiglottic fold to the anterior commissure, and obliterating the left piriform sinus. The lesion was 19x14 mm in size and did not cause significant destruction in cartilage structures (Figure 1).
Figure 1. T1 Weighted and Fat-suppressed Axial Magnetic Resonance Images of the Neck. It was seen a lesion extending from the left aryepiglottic fold to the anterior commissure.
The patient underwent laryngoscopic biopsy with suspicion of malignancy.
During the laryngoscopy, it was observed that the movement of the left hemilarynx decreased. A lesion compatible with the submucosal mass, which filled the left ventricular band and vocal cord, was observed. The biopsy sample was reported as a piece of mucosal tissue containing chronic inflammation. It was stated that there was no evidence of malignancy. The biopsy was repeated because of the mass persisted.
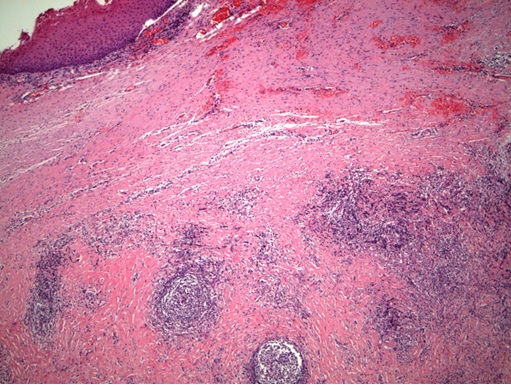
In the microscopic examination of the last taken incisional biopsy material, intense storiform fibrosis was seen under the mucosal surface. The fibrotic background was accompanied by pronounced lymphoid follicles and intense lymphoplasmacytic inflammatory cell infiltration (Figure 2).
Figure 2. Intense Storiform Fbrosis and Lymphoplasmacytic Inflammatory Cell Infiltration were Seen under the Mucosal Surface (HE x40).
There was no evidence of phlebitis. With immunohistochemical studies, it was determined that there were 50 IgG4-positive plasma cells in a high power field (HPF) (Figure 3).
Figure 3. There Were 50 IgG4-positive Plasma Cells in a HPF (IHC x400).
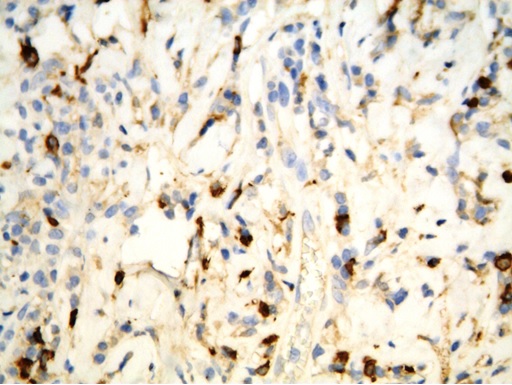
The ratio of IgG4/IgG positive plasma cells was over 40%. As a result, the patient was considered probable IgG4-RD. The patient was not come to follow up after the last biopsy. Therefore, he could not be evaluated in terms of serum IgG4 levels and other organ involvement.
Discussion
IgG4-RD can be seen in any organ in the body, but in the larynx has been reported very few cases. When the literature was examined, it was observed that 14 patients, consisting of 9 case reports, had laryngeal IgG4-RD [4-14].
The mean age of the patients included in the case reports was 51 (Age range: 29-69). The age of our patient was 59. 29% of the patients were female and 57% were male.
Our patient was male. It was noted that most of the cases were men over 50 years old. It was observed that patients presented with symptoms such as hoarseness, dysphonia, dysphagia, throat discomfort, cough, weight loss, odynophagia, dyspnea, and sore throat. Hoarseness was the most commonly seen complaint, as also our patient [4-14]. Although concomitant diseases vary, it was seen that one patient was found to be accompanied by retroperitoneal fibrosis which is in the spectrum of IgG4- RD. The clinical findings of the patients were summarized in the Table 1.
| 1 | 54 | Female | Dysphagia, odynophagia, weight loss, hoarseness | Serum IgG4 levels: 277 mg/dL | IgG lymphocytoid plasma-cell infiltrates | Not found |
| 2 | 58 | Male | Intermittent throat discomfort, voice strain | Serum IgG4 levels: 196 mg/dL | Diffuse storiform fibrosis, and a dense lymphoplasmacytic infiltrate containing reactive follicles | Prednisone, rituximab |
| 3 | 62 | Male | Cough, throat clearing, dysphagia, hoarseness | Serum IgG4 was normal. (28.6 mg/dL) | Intense lymphoplasmacytic infiltrate and fibrosis | Prednisone, rituximab |
| 4 | 50 | Female | Intermittent throat discomfort | Serum IgG4 levels: 154 | Lymphoplasmacytic infiltrate and storiform fibrosis | Rituximab, methylprednisolone |
| 5 | 62 | Male | Cough, globus symptoms, dysphagia, odynophagia, dysphonia, otalgia, malaise | Serum IgG4 levels: 176 mg/dL | Dense plasmacytoid infiltrate in the subepithelial tissue with small numbers of mature appearing lymphocytes | Prednisone |
| 6 | 56 | Male | Hoarseness, rhinitis | Serum IgG4 levels: 180 | Increased influx of IgG4 plasma cells, storiform | Prednisone |
| 7 | 57 | Male | Hoarseness, ulceration of the mouth and throat | Serum IgG4 levels: 196 | Increased influx of IgG4 plasma cells, fibrosis | Prednisone |
| 8 | 37 | Female | Dysphonia, aphthous ulcers | Serum IgG4 levels: 1.4 U | Lymphoplasmacytic infiltrate | Methylprednisolone |
| 9 | Not found | Not found | Not found | Not found | Inflammatory infiltration, obliterative phlebitis, fibrosclerosis | Not found |
| 10 | 29 | Male | Odynophagia, hoarseness, dysphagia | Serum IgG4 was normal. (35 | Storiform fibrosis, lymphoplasmacytic infiltrate | Prednisone |
| 11 | Not found | Not found | Not found | Not found | Not found | Not found |
| 12 | 30 | Female | Dyspnea | Serum IgG4 was normal. (48 mg/dL) | Chronic fibrotic inflammatory infiltrate | Glucocorticoids, rituximab |
| 13 | 50 | Male | Dyspnea | Serum IgG4 was normal. (31 mg/dL) | Lymph follicle formation, interstitial follicular fibrosis, angiogenesis, and inflammatory cell infiltration with plasmacytosis | Prednisolone |
| 14 | 69 | Male | Cough, hoarseness | Seum IgG4 was normal. (29mg/dL) | Not found | Glucocorticoids, rituximab |
The diagnosis of IgG4-RD is made based on three main criteria. These are clinical, laboratory, and histopathological features. Clinically, involvement may be seen in one or more organs. Enlargement or organ dysfunction occurs in relevant organs. If all three of the clinical, laboratory and histopathological features are available, the diagnosis of the IgG4-RD is definitive. In patients with organ symptoms, if only one of the serological or histopathological criteria exists, the patient has probably IgG4-RD [15].
Serum IgG4 level (> 135 mg / dL) is expected to be high in IgG4-RD. However, many different diseases can increase the level of IgG4, and in 30% of IgG4-RD, the level of IgG4 was found to be normal. Serum IgG4 levels were noted to be high in 36% of the laryngeal IgG4-RD cases and ranged from 154 to 277 mg/dl [4-7]. In our case, the serum IgG4 level could not be determined because the patient did not come to follow up after the last biopsy.
IgG4-RD is characterized by histopathologically storiform fibrosis, lymphoplasmacytic infiltration rich in IgG4 positive plasma cells, and obliterative phlebitis. Inflammatory infiltration may be accompanied by eosinophils. When the cases were evaluated histopathologically, all of them had intense lymphoplasmacytic infiltration. Fibrosis was present in 71% of the cases. In one of the cases obliterative phlebitis was observed, while in another, marked eosinophilic infiltration was noted [4-14]. While lymphocytic infiltration rich in plasma cells, and fibrosis were evident in our case, obliterative phlebitis was not observed. Eosinophils were not apparent in concomitant infiltration. The number of IgG4-positive cells required for the diagnosis of IgG4-RD may vary. The IgG4/IgG ratio is as important as the number of IgG4-positive cells. It was shown that there were immunohistochemically at least 50 IgG4-positive cells per high power field (HPF) in the case reports [5,6]. In our case, 50 IgG4-positive cells were found per HPF.
In our case, IgG4-RD clinically mimicked malignancy because it had a mass effect on the larynx. Histopathologically, the differential diagnosis of IgG4-RD includes multiple myeloma, lymphoproliferative diseases, inflammatory myofibroblastic tumor, multicentric Castleman disease, Erdheim Chester disease, or infectious diseases. The diagnosis can be skipped in small biopsy specimens and localization where IgG4-RD is rare, so it is important to evaluate the case with clinical findings.
Systemic glucocorticoids are the first-line approach for IgG4-RD. However, due to the risk of developing steroid- related complications, discontinuation of the drug should be attempted in at least 3 years. For relapsed IgG4-RD, steroids may be re-administered or immunomodulatory drugs such as azathioprine may be added. Rituximab may be effective in many situations where treatment with immunomodulatory drugs has failed [16].
In conclusion, in this case report, we presented the IgG4-RD of the larynx. It should not be forgotten that IgG4-RD can be seen in very rare localization. Accurate diagnosis is important because IgG4-RD responds well to prednisone treatment and prevents unnecessary surgical procedures.
References
- IgG4-related disease Stone JH , Zen Y, Deshpande V. The New England Journal of Medicine.2012;366(6). CrossRef
- High serum IgG4 concentrations in patients with sclerosing pancreatitis Hamano H., Kawa S., Horiuchi A., Unno H., Furuya N., Akamatsu T., Fukushima M., Nikaido T., Nakayama K., Usuda N., Kiyosawa K.. The New England Journal of Medicine.2001;344(10). CrossRef
- Recent advances in knowledge regarding the head and neck manifestations of IgG4-related disease Takano K, Yamamoto M, Takahashi H, Himi T. Auris, Nasus, Larynx.2017;44(1). CrossRef
- IgG4-related disease presenting as hoarseness and postcricoid ulcer Hamadani S, Wang B, Gupta S. Annals of Allergy, Asthma & Immunology: Official Publication of the American College of Allergy, Asthma, & Immunology.2018;120(2). CrossRef
- Clinical Manifestations of IgG4-Related Disease in the Pharynx: Case Series and Review of the Literature Reder L, Della-Torre E, Stone JH , Mori M, Song P. The Annals of Otology, Rhinology, and Laryngology.2015;124(3). CrossRef
- Supraglottic immunoglobulin-G4 related plasma cell granuloma: case report and literature review Khoo JF , Batt M, Stimpson P, Safdar A. Head & Neck.2014;36(6). CrossRef
- IgG4-related disease with atypical laryngeal presentation and Behçet/granulomatous polyangiitis mimicking features Shaib Y, Ton E, Goldschmeding R, Tekstra J. BMJ case reports.2013;2013. CrossRef
- Aphthous Stomatitis and Laryngitis, Another Form of Presentation of an IgG4-Related Disease? Suárez-Díaz S, Núñez-Batalla F, Fernández-García MS , Fernández-Llana MB , Yllera-Gutiérrez C, Caminal-Montero L. Reumatologia Clinica.2020;16(5 Pt 2). CrossRef
- [IgG4-related sclerosing disease of the larynx] Mustafaev D. M.. Vestnik Otorinolaringologii.2017;82(2). CrossRef
- Indolent Laryngeal Mass Causing Progressive Dysphagia Hill R, Baiyee D, Rivero A. JAMA otolaryngology-- head & neck surgery.2020;146(3). CrossRef
- [The invasive IgG4-related disease in larynx: one case report] Zhong H., Li Y., Qiu L. L., Wen W. P., Lei W. B.. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi = Chinese Journal of Otorhinolaryngology Head and Neck Surgery.2020;55(7). CrossRef
- Atypical presentation of immunoglobulin G4-related disease as subglottic stenosis: a case-based review Atienza-Mateo B, Díaz de Terán-López T, Gómez-Román J, Sánchez L, Mons-Lera R, Rubio-Suárez A, Cifrián JM , González-Gay MA . Rheumatology International.2021;41(6). CrossRef
- IgG4-related disease with pseudotumor formation in the larynx Matsushima K, Ohira S, Matsui H, Fukuo A, Honma N, Wada K, Matsuura K. Auris, Nasus, Larynx.2020;47(2). CrossRef
- Treatment-resistant cough: a rare manifestation of IgG4-related disease involving the larynx Syed AS , Colombo RE , Syed BS , Henning PM . BMJ case reports.2020;13(11). CrossRef
- Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011 Umehara H, Okazaki K, Masaki Y, Kawano M, Yamamoto M, Saeki T, Matsui S, Yoshino T, Nakamura S, Kawa S, Hamano H, Kamisawa T, Shimosegawa T, Shimatsu A, Nakamura S, Ito T, Notohara K, Sumida T, Tanaka Y, Mimori T, Chiba T, Mishima M, Hibi T, Tsubouchi H, Inui K, Ohara H. Modern Rheumatology.2012;22(1). CrossRef
- Diagnosis and Treatment of IgG4-Related Disease Kamisawa T, Okazaki K. Current Topics in Microbiology and Immunology.2017;401. CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times