Site Planning of a Newly Installed LINAC along with a Brachytherapy Unit at CMC, Nepal
Download
Abstract
The majority of cancer patients will require radiotherapy at some time during their illness, either for curative or palliative purposes, making it an important part of a multidisciplinary cancer treatment approach. External beam radiotherapy and brachytherapy are two methods of administering radiation to the tumor location. Cobalt tele source, Linear accelerator, and Tomotherapy are examples of external beam radiotherapy equipment; similarly, after loading brachytherapy unit is an example of brachytherapy equipment. Because these units generate radiation, a specific site design is required to guarantee that radiation leakage is kept to a minimum. Linear accelerator and Brachytherapy devices are housed in specialized chambers known as “Bunkers.” The engineering of these bunkers is still a difficulty. The layout of the radiation department is designed in such a way that it will smooth the day-to-day operations and maximize the efficiency of the working crew. The general considerations, location, and layout of different rooms built for the LINAC and brachytherapy unit at CMC, Bharatpur, Nepal are discussed in this study.
Int r oduction
Cancer is becoming more common over the world, and according to the World Health Organization (WHO), it is still the first or second leading cause of death in the majority of countries [1]. Nepal’s age-standardized cancer incidence and mortality rates were estimated to be 78.6/100000 and 54.8/100000, respectively, by the Global Cancer Observatory 2020 [2]. According to Delaney et al, radiotherapy is used by 52 percent of all cancer patients, implying that radiotherapy is used in some manner by more than half of all cancer patients [3]. For most patients, it is routinely used either as a stand-alone treatment or as part of a multidisciplinary strategy. It is also useful in palliative care for symptomatic alleviation of pain and other tumor-related symptoms.
Despite the fact that radiotherapy is an important aspect of cancer treatment, Nepal’s radiotherapy facilities are in poor condition due to the country’s unstable administration, lack of a national cancer control program, poor economic conditions, and lack of atomic energy regulating authority. The lack of skilled people and financial setbacks are major hurdles in establishing a radiation department in Nepal. Though the first radiation center opened in Kathmandu’s Bir hospital in 1991, the expansion of radiation facilities has been gradual since then, with just a small number of facilities accessible to date, with the majority of them focused in the capital [4]. In Low Middle-Income Countries (LMICs) like Nepal, the rising incidence has put a burden on individuals’ finances, as the majority of patients pay for their treatment out of pocket [5].
With all of these obstacles in mind, the decision was made to establish a radiation facility with a LINAC and a Brachytherapy unit at Chitwan Medical College (CMC) in Bharatpur, Nepal. This article goes into the site design and specifications for all of the radiation department’s units that were built at CMC in great detail.
Site Planning Considerations
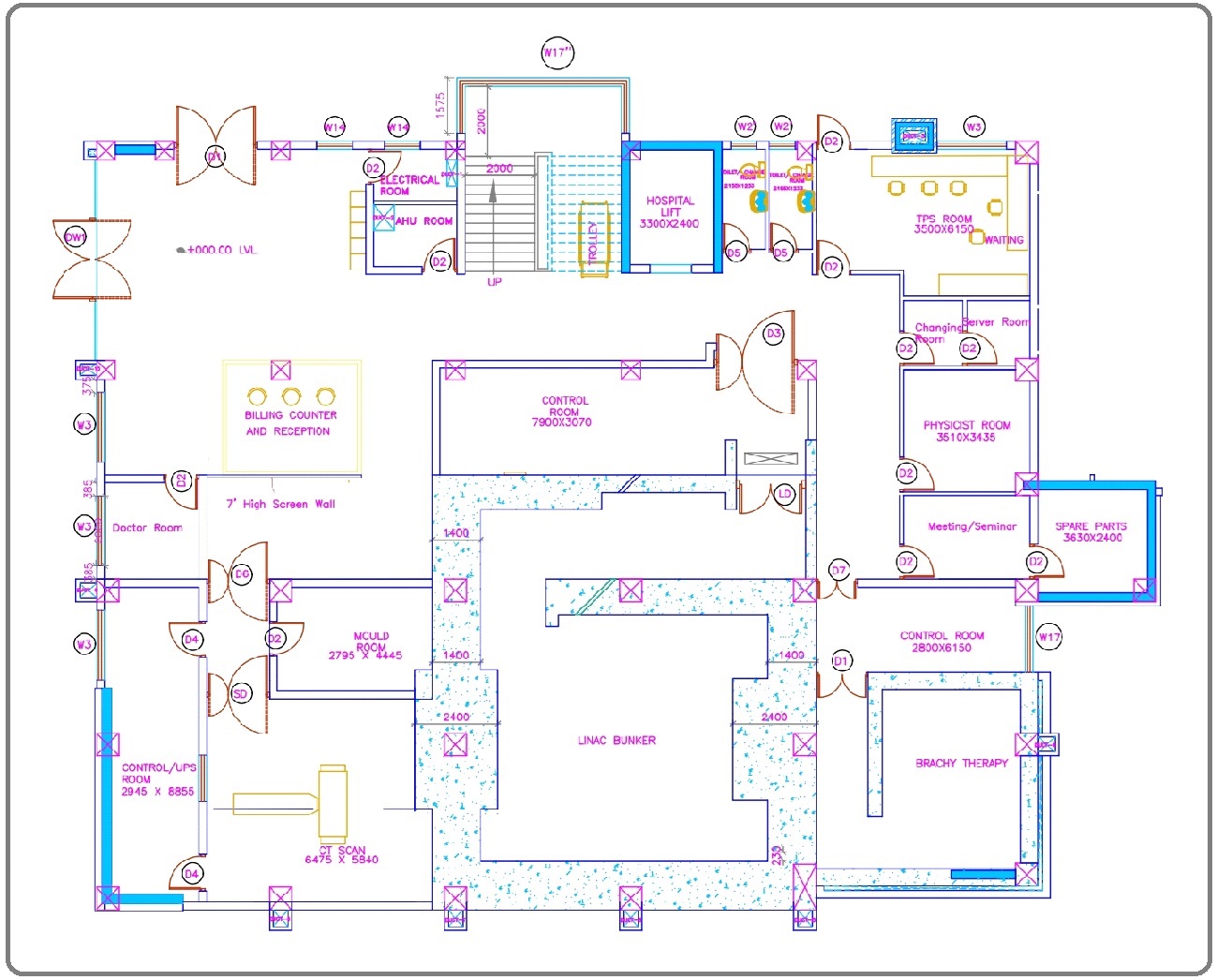
The main hospital’s site houses radiotherapy, which is part of a multidisciplinary approach to cancer treatment. The IAEA’s recommendations, such as a minimum size of 3500 m2 excluding access roads and parking areas, a geological survey of the location, and ground conditions for building foundations, were taken into account while developing the layout of the radiation facility [6]. The land acquisition is sufficient to cover the IAEA-recommended five primary functional areas of the radiotherapy department: reception, administration, and waiting spaces; clinical consultation areas; External Beam Radiotherapy (EBRT); Brachytherapy; Imaging and treatment planning [7]. The entire oncology block is constructed with a connection between each floor of the oncology block and the equivalent main building floor to allow for interdepartmental communication and to ensure that all other diagnostic and treatment options are within easy reach. At the same time, the radiation protection of radiation professionals and the general public was adequately considered by integrating a Radiation Safety Officer (RSO) in the site planning process from the start. RSO developed appropriate shielding for the LINAC bunker, brachytherapy treatment room, and CT simulator as per NCRP recommendations and the IAEA’s Basic Safety Standards [8-11]. Figure 1 depicts the overall structure of the radiation oncology department.
Figure 1. Shows the Ground Floor Layout (Radiotherapy Department).
Location
The building’s site was chosen with particular attention paid to operational efficiency, initial cost, and future growth potential. The expense of shielding floors and walls may have been avoided by establishing a treatment room below ground level, but this was not practicable at our site due to the risk of weakening the main hospital building, which is next to the Oncology Block. As a result, the radiotherapy unit is built on the ground floor of the Oncology Block, which is six stories tall.
Bunker/Treatment Room
Because the Bunker is designed to house a high-energy LINAC (>10 MV and electron energy >15 MeV), there will be neutron contamination. As a result, NCRP 151 and NCRP 79 [10, 11] have been used to build the bunker. The Bunker is home to the equipment with the following specification:
• Varian Medical System, Palo Alto, California, USA, True-Beam model
• Photon energy: 6 MV, 10 MV, 15 MV, 6 MV FFF, and 10 FFF
• Energy of electrons: 6, 9, 12, 15, and 18 MeV
• Dose Rate: 600 MU/min for Photon Beam and 2400 MU/min for Flattening Filter (FF).
• Size of the field: 0.5×0.5 - 40×40 cm2
• Hyperarc and 6D Robotic Couch
• Multi-Leaf Collimator (MLC): 120 leaves (60 pairs) spanning a field size of 40 x 40 cm; 40 pairs at the center of 5mm & 20 pairs at the periphery of 1cm
The bunker’s dimensions are 7.09×6.75 meters, which is plenty of room for the LINAC, a modular cabinet for generating high voltage electricity, and a cabinet for storing the accessories. An entrance door, a maze, a primary barrier, and a secondary barrier are all parts of a bunker. The principal barriers for attenuating the maximum energy, i.e., 15 MV produced by a LINAC, are directly confronting photons of the gantry, for which 240 cm of concrete of density (2.4 gm/cm3) is employed. The bunker’s secondary walls are the bunker’s remaining two walls, which are designed to attenuate stray photons and radiation leaks from the gantry head. Because the energy of radiation leak is higher than the energy of scattered radiation, these walls were built with the energy of radiation leak in mind, with a 140 cm wall thickness. The maze is a path from the bunker to the console room that is planned and constructed to prevent scattered photons and scattered neutrons from exiting the bunker directly. Because scattered neutrons carry more energy than scattered photons, the maze was designed to be as broad as feasible, with a length of 9.34 meters and a curve to limit neutron exposure at the entry. The bunker’s back wall has a chiller connection whose primary purpose is to keep the LINAC cool.
Control Console Room
The LINAC is controlled by radiation treatment technologists in the control console room, which is placed between the entrance to the bunker’s maze and the outer area where patients enter. The control console room at CMC is 7.9×3.07 meters in length. It has a computer system for controlling LINACs, electronic portal imaging, and dosimetry equipment, as well as closed-circuit video monitors for patient monitoring. In the console room, there is a door interlock that disables the radiation beam if the door is not properly closed. The LINAC’s components are controlled by console cabinets in the console room, and a UPS room next to the console room offers 30 minutes of backup power in the event of a power outage.
Treatment Planning System (TPS) Room
Computer terminals are installed in the TPS room so that patient images can be imported, contours can be drawn, and a plan for radiation delivery can be developed. In the TPS room, which is conveniently adjacent to the control console room, 3 Eclipse Planning systems and two somatom contouring stations are installed along with accessories like printers. The size of the TPS room is 4.2×6.15 meters.
Server Room
Often called the “brain of the system,” it stores information about the entire system. The data room stores all patient-related information and is key to its proper operation. Due to manual backup here, it is necessary to change the cassette every day according to the day indicated.
Computerized Tomography (CT) Simulator Room
The CT simulator room is built to accommodate a Siemens 64 slice scanner. In the CT simulator room, the dimensions are 6.48×5.8 meters, which is large enough to accommodate a CT simulator, contrast injector, base plates, and immobilization devices. With a bore diameter of 80 cm, the CT simulator machine provides easy access for the patient and immobilization devices. For accurate patient positioning and putting the fiducials in the right places, three lasers are installed in the simulator room, one on the front wall and two on the lateral walls. The fiducial markers are used for patient repositioning at the time of treatment. During the CT simulation, the simulator communicates with the CT control console from which technologists can see the patient and give commands to the machine to scan prescribed parts. The shielding for the CT simulator was constructed in accordance with NCRP 147 standards [12].
Mould Room
In the mold room, technicians create immobilizing devices based on the patient’s anatomy and the part to be treated. Radiotherapy immobilization devices are used to position, immobilize, and reposition patients during treatment. Patients can simply be taken for CT simulation after their immobilization device is prepared because the mold room is close to the CT simulator room. A tabletop, a water bath, a block cutter, and a cabinet for storing thermoplastic casts and other immobilization devices are all available in the mold room. The mold room has a length of 4.445 meters and a width of 2.98meters.
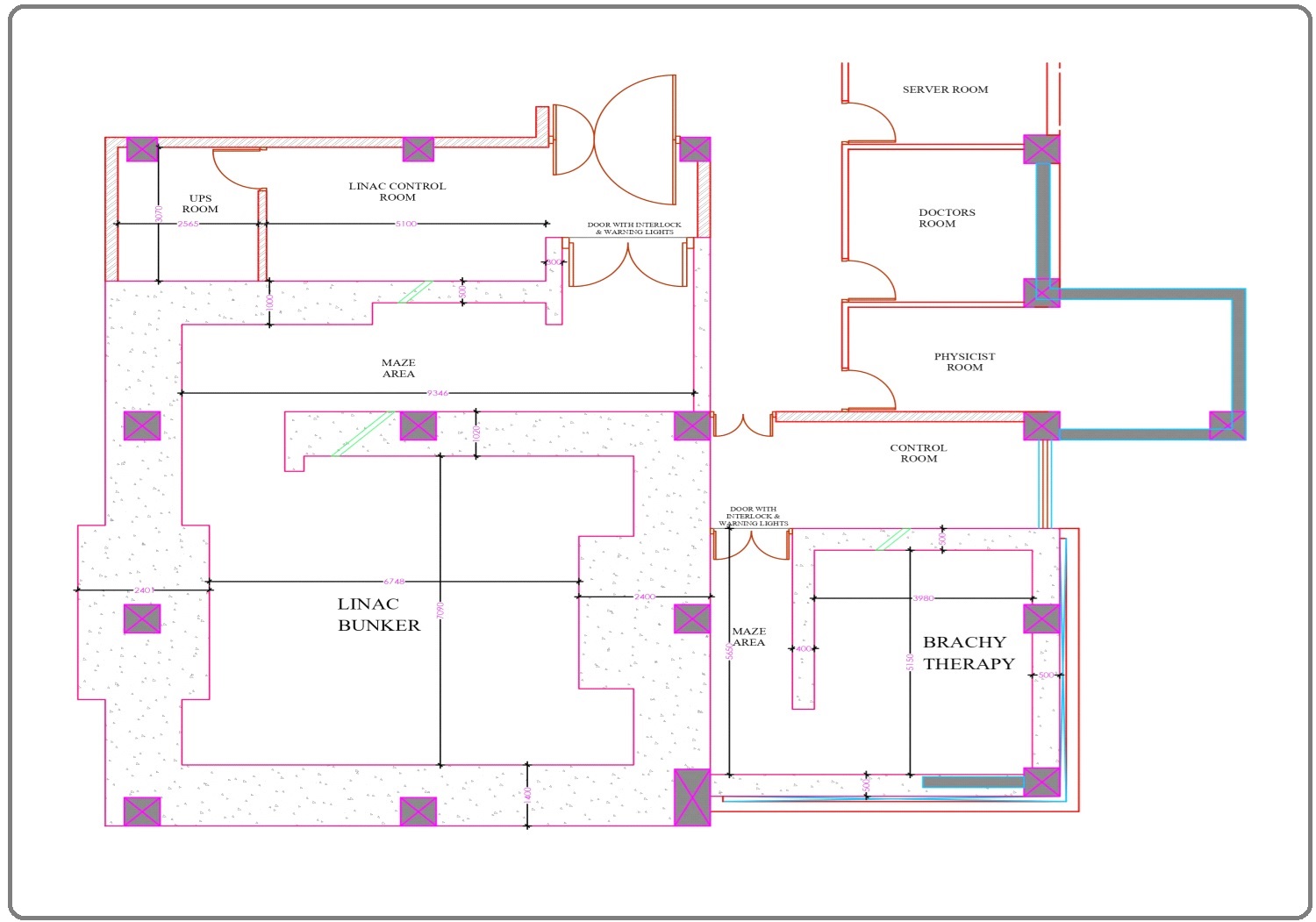
Brachytherapy Treatment Room
The after-loading HDR brachytherapy equipment, patient’s couch, and other accessories may all be accommodated in the brachytherapy treatment room, which is 5.15×3.98 meters in length. According to the plan, the application insertion will take place in the main hospital’s Operation Theatre (OT), and the brachytherapy bunker would only be used to give radiation to the patient. The CMC brachytherapy bunker has a 50 cm wall and ceiling thickness, which is sufficient to offer shielding from the Ir192 source. For isotropic radiation sources, the idea of primary and secondary barriers is meaningless, hence a thickness of 50 cm for the walls and ceiling is sufficient. The brachytherapy bunker’s maze is 1.8 meters wide to provide patients with an easy entry in the event of an emergency. Figure 2 depicts the layout of the brachytherapy treatment room.
Figure 2. LINAC Bunker and Brachytherapy Bunker Layout.
Brachytherapy Control Console Room
The technologist monitors the patient receiving treatment inside the bunker from the brachytherapy control console. This control room is equipped with a mechanism that allows it to feed the source into the patient and return it to the shielded brachytherapy machine directly from the console. The brachytherapy room is 2.45×6.0 meters in length.
Electrical and Networking Requirements
425 VAC, 3-phase 100 Amps, and 55 KVA power are provided to the main power disconnect. The disconnect box for the LINAC bunker is installed on the wall beside the treatment console room. Within the main power disconnect, a 4-gauge lug was used to ground to the grounded building earth. In the event of a power outage, an online UPS will provide power to the therapy delivery, data server, and networking devices. The entire radiation facility is networked with a 1 Gbps, 24 port network switch, and 99.99 percent pure copper wire.
Environmental Requirements
The air conditioning system has been set up to regulate the temperature of the entire working space between 18 and 23 degrees Celsius, 24 hours a day, seven days a week, with a humidity range of 30 to 70%.
Commissioning Tools and Quality Assurance (QA) Equipment
Radiation Field Analyzer (RFA) with reservoir, thimble chamber, parallel plate chamber, diode detector, small volume ionization chamber, Arc Check 4D and Stereophan, 1D Scanner, thermometer, barometer, and electrometer were procured for LINAC commissioning, patient QA and machine QA. During installation and commissioning, a Fluke 451 ion-based survey meter was used to conduct a radiation survey.
Other Technical Specifications
Lasers
There are four lasers in the LINAC bunker: two on the sidewalls, one on the front wall, and one on the ceiling. In the CT Simulator room, three lasers have been installed: two on the sidewalls and one on the front wall (digital laser). In the mould chamber, a digital laser was placed for optimum patient positioning while making immobilization casts.
Warning Light
At the maze’s entrance, an illuminated warning sign linked with a treatment control unit is located at a height of 1700 meters above the floor level. Figure 3 depicts the mounted warning light.
Figure 3. Warning Light.

Patient Surveillance
Operators can observe patients undergoing treatment from the treatment control console room thanks to a closed-circuit camera with tele zoom capabilities installed in the bunker. In the bunker, an audio communication system has been established to allow for two-way contact between the operator and the patient. A patient-activated alarm has also been installed for patients who are unable to make an audible call.
In conclusions, due to a shortage of experienced staff, financial constraints, and other geopolitical obstacles, designing and constructing a radiotherapy facility in a developing nation like Nepal remains a problem. This article includes information on radiation facility site design that will be useful to those planning to develop a comparable unit in Nepal in the future.
References
- Global health estimates: Leading causes of death. (n.d.). WHO | World Health Organization https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death..
- World Health Organization (WHO). Union for International Cancer Control Nepal fact sheet: GLOBOCAN 2020..
- The role of radiotherapy in cancer treatment: estimating optimal utilization from a review of evidence-based clinical guidelines Delaney Geoff, Jacob Susannah, Featherstone Carolyn, Barton Michael. Cancer.2005;104(6). CrossRef
- A medical physics perspective: Radiation therapy in Nepal Adhikari KP. Medical Physics International.2018;6:145-147.
- Estimating the Direct Cost of Cancer in Nepal: A Cross-Sectional Study in a Tertiary Cancer Hospital Khatiwoda SR, Dhungana RR, Sapkota VP, Singh S. Frontiers in Public Health.2019;:p. 160.
- International Atomic Energy Agency, Radiotherapy Facilities: Master Planning and Concept Design Considerations, Human Health Reports, 2014 .
- IAEA - radiotherapy facilities master planning and concept ... (n.d.) Retrieved April 7, 2022, from https://conferences.iaea.org/event/162/contributions/7277/attachments/3203 HYPERLINK "https://conferences.iaea.org/event/162/contributions/7277/attachments/3203/3851/IAEA_-_Radiotherapy_Facilities_Master_Planning_and_Concept_Design_Considerations.pdf"/3851/IAEA_-_Radiotherapy_Facilities_Master_Planning_and_Concept_Design_Consid HYPERLINK "https://conferences.iaea.org/event/162/contributions/7277/attachments/3203/3851/IAEA_-_Radiotherapy_Facilities_Master_Planning_and_Concept_Design_Considerations.pdf"e HYPERLINK "https://conferences.iaea.org/event/162/contributions/7277/attachments/3203/3851/IAEA_-_Radiotherapy_Facilities_Master_Planning_and_Concept_Design_Considerations.pdf"rations.pdf..
- National Committee ON Radiation Protection and Measurements, Structural shielding design and evaluation for medical use of X-rays and gamma rays of energies up to 10 MeV, NCRP 49, NCRP, Washington, DC (1976) .
- International Atomic Energy Agency, International Basic Safety Standards for Protection against Ionizing Radiation and for the Safety of Radiation Sources, Safety Series No. 115, IAEA, Vienna (1996) .
- NCRP Report No. 151. Structural Shielding Design and Evaluation for Megavoltage X- and Gamma-Ray Radiotherapy Facilities, National Council on Radiation Protection and Measurements. 2005 .
- Neutron Contamination from Medical Electron Accelerators (NCRP Report No. 79) Olsen Kjeld J.. Medical Physics.1986;13(6). CrossRef
- National Council on Radiation Protection and Measurements (2004) Structural Shielding Design for Medical X-ray Imaging Facilities Bethesda: NCRP; NCRP Report 147..
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times