COVID-19 Anxiety and Related Factors in Cancer Patients Undergoing External Radiation Therapy
Download
Abstract
Introduction: Studies have shown that anxiety caused by the COVID-19 epidemic affects the patient’s decision-making processes regarding treatment and may even force him to refuse to continue treatment or disrupt the function and efficiency of treatment. This study aimed to determine the anxiety caused by COVID-19 and related factors in cancer patients undergoing radiotherapy.
Methods: This analytical cross-sectional study included 125 cancer patients which sampled through convenience sampling from patients who admitted to radiotherapy centre in Yazd, Iran, in 2021. Patients had different primary cancers such as Breast, Lung, Head and Neck, Prostate, Stomach, Cervix, Blood, Intestine, Brain, Skin, Lymphoma, Kidney and Oesophagus. The COVID-19 Disease Anxiety Scale (CDSA) questionnaire was used to collect data. The frequency, percentage, mean (standard deviation), median (interquartile range=IQR) were used to description and the Mann–Whitney U and Kruskal-Wallis tests were used for data analysis. All analyses were performed in SPSS software (version 24) with a significance level of 5%.
Results: In total, 55.2% of patients (69 patients) were male, 85.6% (107 patients) were married, and the mean (SD) age of participants was 50.16 (13.93) years. Median (IQR) the scores of mental, physical and anxiety symptoms were 11 (13), 4 (8), and 16 (18), respectively, which were moderate in physical and psychological symptoms according to guidelines. In terms of total anxiety classification, total anxiety score in our study was in mild category. Median of the CDSA score was significantly different in levels of age, education, economic status, and type of job (p<0.001).
Conclusion: COVID-19 anxiety in cancer patients was in the mild level. Young people and people with lower social, economic, and educational status are more anxious. However, in addition to targeted safety and prevention measures, training and counselling programs may also be useful in reducing anxiety level.
Introduction
A new strain of Coronavirus (COVID-19) was identified in Wuhan, China in last month of 2019, and spread rapidly throughout China [1]. COVID-19 virus is a significant social threat that causes respiratory and intestinal infections in animals and humans. The virus has been transmitted from animal species to humans [2]. The rapid spread of the virus and the seriousness of the new disease prompted the World Health Organization to change its view of an international public health concern on January 30 to a pandemic on March 11 [3].
COVID-19 disease, in addition to being a significant threat to people’s physical health due to the increase and prolongation of fear and uncertainty about, when it will end, also threatens people’s mental health. People have shown negative emotions, including stress, anxiety, and anger, after the announcement of COVID-19 [4]. Another threat to public mental health is the implementation of nationwide quarantine measures to prevent the spread of COVID-19. While quarantine can be an effective public health measure, it entails significant economic, social, and psychological costs [5]. Chinese researchers report that cancer patients and cancer survivors are at greater risk of severe COVID-19-related events than non-cancer patients [6] and have shown greater rates of anxiety and depression than the general population [7-9]. Studies have shown that anxiety associated with COVID-19 affects patient decision about treatment [10] and can even stop treatment [11]. This fear and anxiety can confuse cancer patients to the point that they refuse to continue treatment for fear of infection which can lead to worsening of their condition [12].
Radiation therapy is one of the most common methods of cancer treatment that can be used alone or in combination with other treatments such as surgery, chemotherapy, or hormone therapy. Approximately 52% of cancer patients receive radiation therapy during their course of treatment [13]. These patients have an increased risk to be exposed to COVID-19 as they are scheduled to receive radiation therapy every day for several weeks. Also, if they become infected with the COVID-19, their treatment need to be stopped for several weeks and this potentially leads to a change in the radiation therapy program and cancer control [14].
Social isolation has been shown to have a significant effect on cancer survival [15, 16]. Moreover, it can be expected that psychological disorders will affect the treatment efficiency and also treatment program of patients undergoing radiation therapy. On the other hand, because COVID-19 in addition to the physical health, can also affect human economic, political, and social issues, this study aimed to determine the anxiety caused by COVID-19 and to evaluate the psychological and physical symptoms in cancer patient undergoing radiation therapy in order to improve the physical and mental health of these patients.
Materials and Methods
Collecting data
This study is an analytical cross-sectional that was performed in the spring and summer of 2021 by random sampling of 125 cancer patients undergoing radiation therapy for various cancers (breast, lung, head and neck, prostate, stomach, cervix, blood, intestine, brain, skin, Lymphoma, kidney, esophagus). Sample size calculation was based on the rule of thumb in sample size for exploratory factor analysis (5 or 10 samples for each question) [17], The minimum sample size for evaluating the structural validity of the 18-item questionnaire is 90; On the other hand, according to the anxiety score reported in the study of Alipour et al. [18] and the use of mean and standard deviation, the sample size was calculated to be 100 people. With considering the 20% non-response probability of patients, the final sample size was calculated as 125 people.
After obtaining the necessary permits from the Vice Chancellor for Research, Shahid Sadoughi University of Medical Sciences, Yazd, and receiving the ethical code (IR.SSU.REC.1400.117), sampling began. Inclusion criteria in this study were all cancer patients referred to Radiation Therapy Center in Yazd since of 2021, who were selected after completing the informed consent form and were randomly selected. Exclusion Criteria for this study included patients who have a history of mental illness (anxiety and depression, Etc.) and people who were not in a favorable mental and physical condition when completing the questionnaire.
Anxiety evaluation Scale
This study was evaluated using the Corona Disease Anxiety Scale (CDSA) questionnaire and demographic factors [18]. Demographic factors in this study included: gender, age, religion, type of cancer, education, marital status, history of infection, history of death due to COVID-19 in friends and family, economic status, number of family members, and occupation.
The CDAS scale has been prepared and validated to measure anxiety caused by the outbreak of the COVID-19 virus in Iran. The validity and reliability of this study have been done by Alipour (2020) [18]. The final version of this tool has 18 items and two components (agents). Items 1 to 9 assess psychological symptoms, and items 10 to 18 assess physical symptoms. The instrument is scored on a 4-point Likert scale (never = 0, sometimes = 1, often = 2, and always = 3); Therefore, the highest and lowest scores that the respondents get in this questionnaire are between 0 and 54. High scores in this questionnaire indicate a higher level of anxiety in people.
According to the raw scores obtained from this questionnaire in Iran, its cutting point was determined and can be seen in Table 1.
| Factor | No anxiety or mild | Moderate anxiety | Severe anxiety |
| Psychological symptoms | 0-5 | 6-19 | 20-27 |
| Physical symptoms | 0-1 | 2-9 | 10-27 |
| Total anxiety | 0-16 | 17-29 | 30-54 |
The reliability of this tool was obtained using Cronbach’s alpha coefficient for the first factor, the second factor, and the whole questionnaire were 0.88, 0.86, and 0.92, respectively [18].
Statistical analysis
Frequency, percentage, mean (standard deviation), median (interquartile range=IQR) indices used for description, and also to evaluate the normality of error distribution in quantitative variables, the Kolmogorov- Smirnov test was used. For inferential statistics, Mann– Whitney U and Kruskal-Wallis tests were used. All analyzes were performed in SPSS 24 software (Chicago, Illinois) with a significance level of 5%.
Results
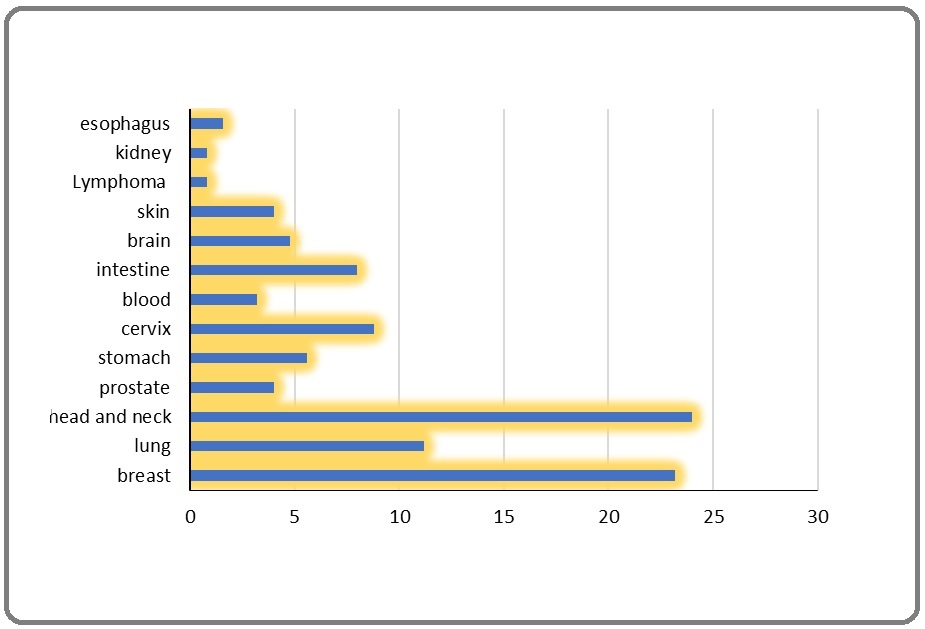
This study was performed on 125 cancer patients undergoing radiotherapy, of which 55.2% (69 patients) were male, and 44.8% (56 patients) were female. Mean (SD) age was 50.16 (13.93), maximum and minimum were 80 and 12 years, respectively. The highest number of patients related to head and neck cancer and breast cancer with 24% (n = 30) and 23.2% (n = 29), respectively, and the lowest number of patients related to lymphoma and kidney cancer, each with 0.8% (n = 1) (Figure 1).
Figure 1. Cancer Frequency.
The highest frequency was belonged to people with middle school education (33.6%, 42 people), housewives (41.6%, 52 people), average economic status (67.2%, 84 people), and married (85.6%, 107 people).
65.6% of patients (82 patients) had a history of COVID-19 in family and friends, and 20.8% of patients (26 patients) had a history of COVID-19 death in family and friends. The frequency of qualitative demographic variables is presented in Table 2.
| Variable | levels | Frequency (percentage) |
| Gender | Male | 69 (55.2) |
| Female | 56 (44.8) | |
| Age | 20 < | 2 (1.6) |
| 20-35 | 10 (8.0) | |
| 36-50 | 52 (41.6) | |
| 51-70 | 48 (38.4) | |
| 71 > | 13 (10.4) | |
| Religion | Shia | 124 (99.2) |
| Non-Shia | 1 (0.8) | |
| Type of cancer | Breast | 29 (23.2) |
| Lung | 14 (11.2) | |
| Head and Neck | 30 (24.0) | |
| Prostate | 5 (4.0) | |
| Stomach | 7 (5.6) | |
| Cervix | 11 (8.8) | |
| Blood | 4 (3.2) | |
| Intestine | 10 (8.0) | |
| Brain | 6 (4.8) | |
| Skin | 5 (4.0) | |
| Lymphoma | 1 (0.8) | |
| Kidney | 1 (0.8) | |
| Esophagus | 2 (1.6) | |
| Education | Illiterate | 3 (2.4) |
| Primary | 25 (20.0) | |
| Middle school | 42 (33.6) | |
| High school | 38 (30.4) | |
| Graduate | 17 (13.6) | |
| Marital status | Single | (14.4) 18 |
| Married | 107 (85.6) | |
| History of COVID-19 in family and friends | Yes | (65.6) 82 |
| No | 43 (34.4) | |
| History of death due to COVID-19 in family and friends | Yes | 26 (20.8) |
| No | 99 (79.2) | |
| The economic status | Weak | 24 (19.2) |
| Medium | 84 (67.2) | |
| Good | 17 (13.6) | |
| Excellent | 0 (0) | |
| The number of family members | Two-person | 4 (3.2) |
| Three-person | 17 (13.6) | |
| Four-person | 43 (34.4) | |
| Five person | 41 (32.8) | |
| Six people and more | 20 (16.0) | |
| Job | Unemployed | 5 (4.0) |
| Freelance | 50 (40.0) | |
| Housewives | 52 (41.6) | |
| Government's employee | 4 (3.2) | |
| Cultural | 2 (1.6) | |
| Student | 3 (2.4) | |
| Retired | 9 (7.2) |
The frequency of cancer patients undergoing radiotherapy to different items of the CDSA questionnaire were presented in Table 3.
| Items | Options Frequency | |||
| Always (%) | Often (%) | Sometimes (%) | Never (%) | |
| Thinking about Coronavirus makes me anxious | 24 (19.2) | 21 (16.8) | 48 (38.4) | 32 (25.6) |
| I feel tense when I think about the Coronavirus threat. | 13 (10.4) | 21 (16.8) | 44 (35.2) | 47 (37.6) |
| I am seriously worried about the prevalence of Coronavirus | 24 (19.2) | 19 (15.2) | 50 (40.0) | 32 (25.6) |
| I am afraid of contracting Coronavirus | 43 (34.4) | 17 (13.6) | 34 (27.2) | 31 (24.8) |
| I fear that I might contract Coronavirus anytime | 27 (21.6) | 11 (8.8) | 43 (34.4) | 44 (35.2) |
| Minor symptoms make me think that I am contracting the virus, and I start checking myself | 20 (16.0) | 21 (16.8) | 42 (33.6) | 42 (33.6) |
| I am concerned about transferring the virus to others around me. am concerned about transferring the virus to others around | 53 (42.4) | 37 (29.6) | 24 (19.2) | 11 (8.8) |
| My anxiety about Coronavirus has interfered with my daily activities | 25 (20.0) | 27 (21.6) | 34 (27.2) | 39 (31.2) |
| The mass medias focus on Coronavirus make me anxious | 16 (12.8) | 13 (10.4) | 40 (32.0) | 56 (44.8) |
| Thinking about Coronavirus has interrupted my sleep | 9 (7.2) | 10 (8.0) | 33 (26.4) | 73 (58.4) |
| I have lost my appetite because of thinking about Coronavirus | 8 (6.4) | 2 (1.6) | 17 (13.6) | 98 (78.4) |
| I get a headache when I think about Coronavirus | 7 (5.6) | 6 (4.8) | 33 (26.4) | 79 (63.2) |
| My body starts jittering when I think about Coronavirus | 6 (4.8) | 8 (6.4) | 13 (10.4) | 98 (78.4) |
| I get goose bumps when I think about Coronavirus | 6 (4.8) | 5 (4.0) | 11 (8.8) | 103 (82.4) |
| Coronavirus has become my nightmare | 5 (4.0) | 11 (8.8) | 25 (20.0) | 84 (67.2) |
| I have less physical activity because of my fear of Coronavirus | 18 (14.4) | 29 (23.2) | 45 (36.0) | 33 (26.4) |
| I find it hard to talk with others about Coronavirus | 8 (6.4) | 14 (11.2) | 55 (44.0) | 48 (38.4) |
| I feel my heart beating when I think about Coronavirus | 6 (4.8) | 14 (11.2) | 30 (24.0) | 75 (60.0) |
Among the answer options, the highest frequency of the “always” option was related to the item “I am concerned about transferring the virus to others around me” (42.4%) and the highest frequency of the “never” option was related to the item “I get goose bumps when I think about Coronavirus” (82.4 %).
Results of the Kolmogorov-Smirnov test showed that none of the quantitative variables of the study had a normal distribution (p <0.05).
As shown in Table 4, the median (IQR) scores of physical symptoms, psychological symptoms, and total anxiety caused by COVID-19 in cancer patients were 4 [8], 11 [13], and 16 [18], respectively. According to the scale of anxiety intensity (Table 1) in moderate physical and mental symptoms and the median of the total anxiety, the score is in the maximum range of anxiety or mild anxiety on the CDSA scale.
| Dimension | median (IQR) | Minimum score | Maximum score |
| Physical Symptoms | 4 (8) | 0 | 27 |
| Psychological Symptoms | 11 (13) | 0 | 27 |
| Total Anxiety | 16 (18) | 0 | 54 |
According to Table 5, results of Kruskal-Wallis test showed, there was a significant difference between median of scores in terms of age, education, economic status, and type of job (p <0.05).
| Variable | Variable levels | Median (IQR) | p-value * |
| Gender | Male | 14.0 (16.0) | *0.229 |
| Female | 17.0 (18.7) | ||
| Age | 20 < | 23.5 (23.0) | |
| 20-35 | 4.0 (16.2) | ||
| 36-50 | 13.0 (14.5) | 0.019** | |
| 51-70 | 16.5 (21.2) | ||
| 71 > | 17.0 (30.0) | ||
| Religion | Shia | 16.0 (18.0) | *1 |
| Non-Shia | 14.0 (0) | ||
| Type of cancer | Breast | 14.0 (16.5) | |
| Lung | 16.5 (17.0) | ||
| Head and Neck | 17.5 (26.0) | ||
| Prostate | 14.0 (15.5) | 0.586** | |
| Stomach | 14.0 (13.0) | ||
| Cervix | 17.0 (34.0) | ||
| Blood | 12.5 (16.0) | ||
| Intestine | 10.0 (18.0) | ||
| Brain | 14.5 (18.0) | ||
| Skin | 6.0 (28.0) | ||
| Lymphoma | 38.0 (0) | ||
| Kidney | 12.0 (0) | ||
| Esophagus | 12.5 (9.0) | ||
| Education | Illiterate | 54.0 (41.0) | 0.013** |
| Primary | 22.0 (30.0) | ||
| Middle school | 16.0 (18.0) | ||
| High School | 12.0 (17.0) | ||
| Graduate | 13.0 (18.0) | ||
| Marital status | Single | 17.0 (21.0) | 0.640* |
| Married | 16.0 (17.0) | ||
| History of COVID-19 in family and friends | Yes | 14.5 (16.0) | 0.248* |
| No | 17.0 (26.0) | ||
| History of death due to COVID-19 in family and friends | Yes | 17.5 (11.2) | 0.152* |
| No | 14.0 (20.0) | ||
| The economic situation | Weak | 30.0 (18.0) | |
| Medium | 14.0 (15.7) | >0.001** | |
| Good | 9.0 (13.5) | ||
| Excellent | 0 | ||
| The number of family members | Two-person | 19.5 (29.7) | |
| Three-person | 13.0 (18.0) | **0.169 | |
| Four-person | 14.0 (17.0) | ||
| Five person | 14.0 (18.0) | ||
| Six people and more | 22.0 (29.2) | ||
| Job | Unemployed | 26.0 (14.0) | |
| Freelance | 11.0 (14.0) | ||
| Housewives | 17.0 (18.7) | ** 0.008 | |
| Government's employee | 5.0 (13.5) | ||
| Cultural | 17.5 (17.0) | ||
| Student | 23.0 (6.0) | ||
| Retired | 22.0 (27.0) |
* Mann–Whitney U, ** Kruskal-Wallis test
Discussion
Studies have shown that patients with malignancies show more anxiety and depression than the general population, and as the course of treatment slows down, there will be more anxiety [7-9].
Wang et al. in a study on the effect of the COVID-19 epidemic on patients with suspected breast cancer reported that COVID-19-related anxiety affects the patient’s decision about treatment [10]. In another retrospective study on 160 patients with or suspected breast cancer, he showed that anxiety caused by COVID-19 could stop treatment [11]. Although this fear and anxiety affect many people, it can confuse cancer patients to the point that they refuse to continue treatment due to fear of infection and worsen their condition [12].
Given the role of social isolation in cancer survival [15, 16], it can be expected that the psychological disorders caused by COVID-19 will affect the fractionated treatment program and the treatment efficiency of patients undergoing radiotherapy. Therefore, due to the lack of research on anxiety caused by COVID-19, especially on cancer patients undergoing radiation therapy, this study aimed to determine the anxiety caused by COVID-19 and its psychological and physical symptoms in these patients in order to decisions can be made to improve the physical and mental health of these patients.
This study is a cross-sectional analytical study performed in a charity radiotherapy center from April to September 2021. At some point during this time, the fourth and fifth outbreaks of COVID-19 occurred. We have found that factors such as economic status, history of illness, and history of death due to COVID-19 in family and friends directly affect the incidence of anxiety and depression.
COVID-19 has caused a wave of stress, anxiety, and depression worldwide [19]. Numerous environmental and social factors can affect the psychological and physical symptoms of anxiety. Economic and social status is one of the most critical factors in anxiety and one of the psychological and physical symptoms caused by anxiety in society [20]. In this study, the results showed that economic status is very effective in the anxiety score of cancer patients. The median score of anxiety in cancer patients undergoing radiotherapy with poor economic status (median score=30) was three times higher than the median anxiety score in patients with good economic status (median score =9). Unemployed people with a median anxiety score of 26 also have the most anxiety among the mentioned jobs. The authorities need to pay more attention to the unemployed peoples and pay special attention to them.
Following the outbreak of the COVID-19 epidemic, studies have been conducted on anxiety by gender. Moghanibashi et al. conducted a study to assess the level of anxiety in the general population of Iran at the time of the outbreak of the COVID-19 epidemic. The results showed that the anxiety symptoms were normal in 49.1% of cases, severe in 9.3%, and very severe in 9.8%. Also, the rate of anxiety in females was significantly higher than males [21]. A study by Cuiyan Wang et al. in China entitled “Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease” showed that more than 25% of the participants have experienced anxiety symptoms and females are significantly more likely than males to suffer from anxiety, stress, and depression [22]. The results of present study also showed that although females (median score =17) had more anxiety than males (median score =14), this difference was not significant.
Another demographic variable associated with anxiety and fear of death among humans is age. One of the most popular theories about death anxiety is that there will be more fear and anxiety about death as people get older. Some studies have suggested a direct relation between death anxiety and—aging [23]. Suhail et al. investigated the correlation between death anxiety and demographic factors of age, religion, and gender. The results showed that older people and people with less religious beliefs showed more death anxiety [24]. In the present study, gender has a significant effect on the incidence of COVID-19-induced anxiety in cancer patients undergoing radiotherapy, so that the incidence of anxiety has increased with age (p<0.05).
Sun et al. examined the prevalence of acute posttraumatic stress symptoms during the COVID-19 outbreak in Wuhan, China. In this study, which was conducted online, the three demographic variables of gender, age, and educational background were examined. The results showed that people with less education have more stress and anxiety against COVID-19 [25]. The present study showed that education had a significant effect on the level of anxiety caused by the COVID-19 epidemic (p<0.05). The median score of anxiety in illiterate participants was 54, and the median anxiety score in participants with university education was 13.
There seems to be no difference between gender, education, and the economic status of members of society in terms of the “chance” of getting COVID-19. Moreover, to prevent its adverse effects on the efficiency of radiation therapy or to prevent delays or changes in the fractionated treatment program of these patients, in the first step, it is necessary to take targeted educational, monitoring, and practical measures in safety and prevention in the face of COVID-19 by the authorities. However, the results of this study showed that the incidence of anxiety caused by the COVID-19 epidemic in cancer patients undergoing radiotherapy in the elderly, with lower social, economic, and educational status, is significant. Suppose it is possible to consider a relationship between socio-occupational status, education, age, and economic status of patients on the one hand and their level of knowledge about the COVID-19 epidemic, on the other hand. In that case, it can be accepted that education and counseling significantly affect their anxiety. However, accepting this relationship could be the subject of future studies.
Therefore, due to the uncertainty of the end of this epidemic, it may be better to develop training and counseling programs in the next step in order to reduce and improve the psychological and physical symptoms of anxiety in patients and companions during the COVID-19 period. In other words, it may be better for governments, in addition to safety and preventive measures to prevent the consequences of the COVID-19 outbreak, also consider the psychological problems caused by the COVID-19 and it is recommended that people with high score of psychological and physical symptoms of anxiety be identified in order to maintain their mental health by considering counseling programs by a psychologist. In this regard, psychotherapy through telemedicine technologies can be helpful.
This study was accompanied by limitations, such as the concern of families about getting the COVID-19 in the face of individuals and the confusion and boredom of some patients, which led to a prolongation of the data acquisition. Another case is that radiotherapy patients were not separated from patients who had chemotherapy in addition to radiotherapy, and also, the patient’s cancer stage was not considered in this study. Therefore, the intervening effect of variables of chemotherapy and cancer stage on anxiety caused by COVID-19 in radiotherapy patients could not be evaluated.
In conclusion, for the first time in Iran, this study examined the level of anxiety in cancer patients undergoing radiation therapy due to the COVID-19 epidemic to prevent the adverse effects of anxiety on the efficiency of radiation therapy or to prevent delay or change in fractionated radiation therapy program.
The results showed that age and social, economic, and educational status significantly affected the incidence of anxiety caused by the COVID-19 epidemic in cancer patients undergoing radiotherapy, in such a way that in older people as well as people with lower social, economic and educational status, more anxiety occurs. Investigating the relationship between these variables and patients’ knowledge can be the subject of future studies; however, if this relationship can be accepted, it may be suggested that the authorities, in addition to targeted educational, monitoring and practical measures in safety and prevention, consider training and counseling programs to prevent anxiety in cancer patients.
Acknowledgments
Thanks to all the patients who patiently participated in this study and Yazd Radiation Therapy Center staff. This study was conducted with the permission and support of Shahid Sadoughi University of Medical Sciences, Yazd, Iran, and with the ethics code of IR.SSU.REC.1400.117.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Declaration of interest statement
The authors declare that they have no competing interests.
Funding
All authors hereby declare that there is no potential or actual personal, financial, or political interest related to this study.
Authors’ contributions
Korosh Saber collected the data, drafted and wrote the manuscript. Farzan Madadizadeh contributed to the statistical analysis. Nima Hamzian participated in the study design and helped drafted and edited the manuscript. All authors contributed to the interpretation of the findings and read and approved the final manuscript.
References
- A pneumonia outbreak associated with a new coronavirus of probable bat origin Zhou Peng, Yang Xing-Lou, Wang Xian-Guang, Hu Ben, Zhang Lei, Zhang Wei, Si Hao-Rui, Zhu Yan, Li Bei, Huang Chao-Lin, Chen Hui-Dong, Chen Jing, Luo Yun, Guo Hua, Jiang Ren-Di, Liu Mei-Qin, Chen Ying, Shen Xu-Rui, Wang Xi, Zheng Xiao-Shuang, Zhao Kai, Chen Quan-Jiao, Deng Fei, Liu Lin-Lin, Yan Bing, Zhan Fa-Xian, Wang Yan-Yi, Xiao Geng-Fu, Shi Zheng-Li. Nature.2020;579(7798). CrossRef
- Origin and evolution of pathogenic coronaviruses Cui Jie, Li Fang, Shi Zheng-Li. Nature Reviews. Microbiology.2019;17(3). CrossRef
- World Health Organization 2. WHO Director-General’s remarks at the media briefing on 2019-nCoV on 11 February 2020 .
- Addressing mental health needs: an integral part of COVID-19 response Adhanom Ghebreyesus Tedros. World psychiatry: official journal of the World Psychiatric Association (WPA).2020;19(2). CrossRef
- The psychological impact of quarantine and how to reduce it: rapid review of the evidence Brooks Samantha K., Webster Rebecca K., Smith Louise E., Woodland Lisa, Wessely Simon, Greenberg Neil, Rubin Gideon James. The Lancet.2020;395(10227). CrossRef
- Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China Liang W, Guan W, Chen R, Wang W, et al . The Lancet. Oncology.2020;21(3). CrossRef
- Cancer, immune suppression and Coronavirus Disease-19 (COVID-19): Need to manage drug safety (French Society for Oncology Pharmacy [SFPO] guidelines) Slimano Florian, Baudouin Amandine, Zerbit Jérémie, Toulemonde-Deldicque Anne, Thomas-Schoemann Audrey, Chevrier Régine, Daouphars Mikaël, Madelaine Isabelle, Pourroy Bertrand, Tournamille Jean-François, Astier Alain, Ranchon Florence, Cazin Jean-Louis, Bardin Christophe, Rioufol Catherine. Cancer Treatment Reviews.2020;88. CrossRef
- Depression and anxiety in patients with cancer Pitman Alexandra, Suleman Sahil, Hyde Nicholas, Hodgkiss Andrew. BMJ (Clinical research ed.).2018;361. CrossRef
- Assessment of Depression and Anxiety in Breast Cancer Patients: Prevalence and Associated Factors Tsaras Konstantinos, Papathanasiou Ioanna V., Mitsi Dimitra, Veneti Aikaterini, Kelesi Martha, Zyga Sofia, Fradelos Evangelos C.. Asian Pacific journal of cancer prevention: APJCP.2018;19(6). CrossRef
- Epidemiology of mental health problems among patients with cancer during COVID-19 pandemic Wang Y, Duan Z, Ma Z, Mao Y, Li X, Wilson A, et al . Translational psychiatry.2020;10(1). CrossRef
- Breast Cancer and COVID-19: The Effect of Fear on Patients' Decision-making Process Vanni Gianluca, Materazzo Marco, Pellicciaro Marco, Ingallinella Sara, Rho Maurizio, Santori Francesca, Cotesta Maria, Caspi Jonathan, Makarova Anna, Pistolese Chiara Adriana, Buonomo Oreste Claudio. In Vivo (Athens, Greece).2020;34(3 Suppl). CrossRef
- "Pandemic fear" and COVID-19: mental health burden and strategies Ornell Felipe, Schuch Jaqueline B., Sordi Anne O., Kessler Felix Henrique Paim. Revista Brasileira De Psiquiatria (Sao Paulo, Brazil: 1999).2020;42(3). CrossRef
- Evidence-based estimates of the demand for radiotherapy Delaney G. P., Barton M. B.. Clinical Oncology (Royal College of Radiologists (Great Britain)).2015;27(2). CrossRef
- Effects of prolongation of overall treatment time due to unplanned interruptions during radiotherapy of different tumor sites and practical methods for compensation Bese Nuran Senel, Hendry Jolyon, Jeremic Branislav. International Journal of Radiation Oncology, Biology, Physics.2007;68(3). CrossRef
- Social isolation: Impact on treatment and survival in patients with advanced cancer. Moore Sara, Leung Bonnie, Bates Alan, Ho Cheryl. Journal of Clinical Oncology.2018;36(34_suppl). CrossRef
- A systematic review of the supportive care needs of people living with and beyond cancer of the colon and/or rectum Kotronoulas Grigorios, Papadopoulou Constantina, Burns-Cunningham Kathryn, Simpson Mhairi, Maguire Roma. European Journal of Oncology Nursing: The Official Journal of European Oncology Nursing Society.2017;29. CrossRef
- Cross-cultural adaptation and psychometric validation of the Persian version of the Cardiac Rehabilitation Barriers Scale (CRBS-P) Ghanbari-Firoozabadi Mahdieh, Mirzaei Masoud, Vafaii Nasab Mohammadreza, Grace Sherry L., Okati-Aliabad Hassan, Madadizadeh Farzan, Dadras Hakimeh, Amrolahi Najmeh, Entezari Mohamadmehdi, Sadrbafghi Seyed Mahmood. BMJ open.2020;10(6). CrossRef
- A New Self-Reported Assessment Measure for COVID-19 Anxiety Scale (CDAS) in Iran: A Web-Based Study Alipour Ahmad, Ghadami Abolfazl, Farsham Aida, Dorri Negin. Iranian Journal of Public Health.2020;49(7). CrossRef
- 2019-nCoV epidemic: address mental health care to empower society Bao Yanping, Sun Yankun, Meng Shiqiu, Shi Jie, Lu Lin. Lancet (London, England).2020;395(10224). CrossRef
- Neighbourhood socioeconomic status, maternal education and adverse birth outcomes among mothers living near highways Généreux M., Auger N., Goneau M., Daniel M.. Journal of Epidemiology and Community Health.2008;62(8). CrossRef
- Assessing the anxiety level of Iranian general population during COVID-19 outbreak Moghanibashi-Mansourieh A. Asian journal of psychiatry.2020;51. CrossRef
- Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China Wang Cuiyan, Pan Riyu, Wan Xiaoyang, Tan Yilin, Xu Linkang, Ho Cyrus S., Ho Roger C.. International Journal of Environmental Research and Public Health.2020;17(5). CrossRef
- Death anxiety in Japan and Australia Schumaker J. F., Warren W. G., Groth-Marnat G.. The Journal of Social Psychology.1991;131(4). CrossRef
- Correlates of death anxiety in Pakistan Suhail Kausar, Akram Saima. Death Studies.2002;26(1). CrossRef
- Prevalence and risk factors of acute posttraumatic stress symptoms during the COVID-19 outbreak in Wuhan, China Sun L, Sun Z, Wu L, Zhu Z, Zhang F, Shang Z, et al . MedRxiv.2020;:1-17. CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times