Infantile Fibromatosis of the Infratemporal Fossa Extending to Oropharynx
Download
Abstract
The Case Study describes the clinical radiographic Surgical Procedure with reconstruction and histopathology Infantile fibromatosis of infratemporal fossa extending to oral cavity and Oropharynx in a two-year-old male child. This condition is rarer in two-year-old child mainly in infratemporal fossa extending to Oropharynx and protruding into oral cavity leading to tremendous suffering of the child for breast feeding, eating with occasional profuse bleeding. The differential diagnosis, management and long term follow up for two years are also mentioned. The need for aggressive surgical management, rare site and operability in this region is very rarer of rarest. The absence of recurrence after 2 years follow up is significant and we can declare the patient is cured from the primary disease. This paper gives guide to how to approach the disease process.
Introduction
Infantile fibromatosis is a proliferative fibrous childhood condition that originates from skeletal muscles, fasciae or periosteum and may invade adjacent structures [1, 2] with unknown pathogenesis. The lesion has a strong tendency for local recurrence and aggressive infiltrating growth. It is most common in the shoulder girdle, the thigh and gluteal region of growing adults and head-neck region in children. Most cases of aggressive infantile fibromatosis were clinically misdiagnosed as fibroma, fibrous histiocytoma, granuloma, cyst, ameloblastoma, fibrous dysplasia or Sarcoma. Sarcoma was the initial clinical diagnosis in this case; however, the histopathological confirmation was aggressive infantile fibromatosis and the management was appropriate.
According to the World Health Organization Classification, infantile fibromatosis is classified in diffuse (Mesenchymal and desmoid types) [2]. The diffuse type is more common and is characterized by an infiltrative growth of premature fibroblasts and a low collagen component. The desmoids type is characterized by an infiltrative proliferation of more mature fibroblasts within a variable amount of collagen. The desmoid type of infantile fibromatosis represents the childhood counterpart of extra abdominal desmoids in adults. Imaging modality in the form of plain and contrast CT and MRI were used for characterization; pre-operative planning and follow-up. Therapy in our case is mainly surgical, since there is no risk of metastasis.
Local recurrences range from 20% to 70% of cases [3-5]. In this case after two years of follow up there was no recurrence. We declare this patient was free from primary disease.
Case Study
A two-year-old male child was moving from hospital to hospital for intra oral swelling which was obstructing baby’s feeding and bleeding with bites. Before coming to us (Figure 1) patient was treated with blood transfusions and antibiotics and also planned for pre operative chemotherapy to down stage the tumor and plan for surgery but the condition of mass was not permitting to do any other therapy as tumor was sloughing off and, also bleeding with baby bites.
Figure 1. Oral Lesion.

So, aggressive step was needed to take to save baby life (Figure 2).
Figure 2. Computed Tomography Scan Shows Extension of the Lesion into the Zygomatic Arch.

History of fever was reported in the past and the family history was unremarkable. Laboratory test were within normal limits after correction of anemia.
M. D. C. T. Report
A well-defined moderately enhancing soft tissue density mass lesion is seen in Lt. infratemporal fossa. This lesion has attenuation value of 30 to 33 H. U. on plain scan and 68 H. U. on contrast scan.
his lesion causes remodeling of the Lt. zygomatic process which is also mildly thinned out and is displaced outwards to Lt side. Lt. temporalis and masticator muscles are stretched over this mass lesion outwards. Inferiorly this lesion is seen extending into medial aspect of mandibular ramus on Lt side in the masticator space and also involves the buccinator space.
There is bony remodeling of the Lt. ramus of mandible. There is also small extension into the Lt. Bucco-gingival space.
Medially this lesion displaces the pterygoid muscles medially and also projects into the oral cavity and in the oropharynx causing mild narrowing of the oropharynx. Posterior portion of maxilla is also displaced medially with medial displacement of Lateral wall of Lt. maxillary sinus and the lateral pterygoid plate on Lt. side. T-M jt. appears normal.
Biopsy Report
a) Spindle cell lesion suggestive of infantile fibromatosis
b) Bone marrow biopsy – No diagnostic – abnormality seen.
Treatment
Surgical Plan – Incision, control of carotid, division of the mandible, excision of the tumor in total.
Lip splitting upper cervical incision taken upper and lower flaps raised (Figure 3 and 4), common carotid, internal carotid and external carotid arteries exposed (Figure 5).
Figure 3. Computed Tomography Scan Shows Involvement of the Buccinator Space and Bucco-gingival Space.

Figure 4. Incision Marking.

Figure 5. External Carotid Artery.

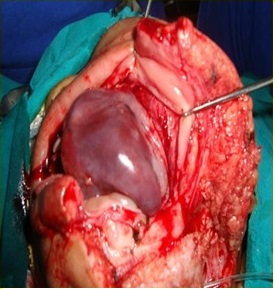
No. 5 infant feeding tube passed around external carotid artery and tied temporarily. Lymph nodes along with upper Jugular and carotid removed. Mandible was divided in midline, tumor mobilized from masseter, buccinator along with part of muscle (Figure 6), continued towards retromolar triangle, Infratemporal fossa.
Figure 6. Mobilization of Tumor.
Medial and lateral pterygoid muscles, superiorly from infra orbital fissure, there was no capsular breach in dissection, dissection done with sharp and electrocautery. Tumor was excised in total bleeding controlled from infra orbital fossa; external carotid ligation released bleeding rechecked (Figure 7).
Figure 7. After Completion of Excision.

Local flaps were raised, intra oral reconstruction done, mandible fixed with wire, incision closed in two layers (Figure 8).
Figure 8.Shows Clinical Photograph of the Fifth Postoperative Day of the Kid.

Histopathology Report
Left cheek swelling
Ulcerated inflammatory myofibroblastic tumor (Intermediate category of Managerial Group of soft tissue tumors) Infantile fibromatosis Surgical Lines of excision: Uninvolved.
Lympho – vascular space invasion: Not seen Lymph node - all exhibiting reactive reticuloendothelial cell hyperplasia.
Follow Up
For a period of 2 years no local recurrence, no facial defects. Patient was free from the disease.
Discussion
Infantile fibromatosis was first described by Stout [1, 2] in 1954 as a distinct entity that develops from the tissues of the musculo aponeurotic system. Such tumors tend to invade adjacent structures without any distant metastases [3,4].
The etiology is unclear. The presence of membrane specific hormone receptors on the fibroblasts supports a hormonal-based theory although previous trauma has also been considered as a predisposing factor [1,6]. Clinical and radiologically it is almost impossible to make a diagnosis of infantile fibromatosis. Pre- op. diagnosis is confirmed by biopsy only.
In conclusion we conclude that infantile fibromatosis of the infratemporal fossa is a rare locally aggressive benign lesion. It is a challenge to surgeon whether to operate or go for pre- operative down staging procedures like chemotherapy/radiotherapy, but in this case considering critical conditions like bleeding, difficulty in feeding, biting of child surgical excision is must, and pre operative CT and Biopsy are used for surgical planning and treatment. This case is a rarest of rarer.
References
- A textbook of Oral Pathology 4th edition Shafer W , Hine M , Levy B . Churchill Liniston.1984;171.
- Juvenile fibromatosis affecting the jaws. Report of three cases Melrose RJ , Abrams AM . Oral Surgery, Oral Medicine, and Oral Pathology.1980;49(4). CrossRef
- Juvenile fibromatoses Stout AP . Cancer.1954;7(5). CrossRef
- Aggressive fibromatosis of the head and neck Wilkins SA , Waldron CA , Mathews WH , Droulias CA . American Journal of Surgery.1975;130(4). CrossRef
- [Maxillary and mandibular desmoid fibromas (author's transl)] Bertrand JC , Plautier D, Chanterelle A, Mazza N. Revue De Stomatologie Et De Chirurgie Maxillo-Faciale.1981;82(2).
- Soft tissue tumors: Fibromatosis (4th ed) St Louis, Mosby Enzinger F, Weiss S. 2001;:371.
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2023
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times