Characteristics of Chronic Lymphocytic Leukemia in Sudanese Patients
Download
Abstract
Objective: Our study aimed to characterize clinical, hematological and Immunophenotyping patterns in Sudanese patients with Chronic Lymphocytic Leukemia.
Methods: A cross-sectional study was conducted in Khartoum state, Sudan, during the period from April 2017 to April 2018, involved 110 CLL patients. Physical examination, Complete Blood Count and Immunophenotyping were performed for all patients to confirm the diagnosis. Clinical staging such as Rai and Binet stages were applied. The statistical analysis was performed by using SPSS version 23.0.
Results: In this study, 71.8% were males and 28.2% were females. Lymphadenopathy, splenomegaly, hepatomegaly, leukocytosis, thrombocytopenia, and anemia were seen in 71%, 49%, 13%, 60.9%, 39% and 34.5% of patients respectively. However, about 90% of patients displayed an advanced Rai risk stage and 70% were at Binet stage B or C. All CLL samples expressed CD45, CD19 and CD20. All the CLL cases were negative for the T-cell marker CD3.CD5 was expressed in 80% patients; CD23 was expressed in 92.7% patients. CD22, CD79b and FMC7 were negative in 91.8%, 77.3%, and 96.4% of patients respectively.
Conclusions: CLL in Sudan is a disease of the elderly and more frequently in males than females. The incidence at young patients was higher than those reported by Western studies. Most of our patients presented advanced Rai and Binet stages. CD22 may be a highly specific marker for diagnosing CLL in Sudanese patients and should be included in all diagnostic panels used to differentiate CLL from other B cell lymphoproliferative disorders in Sudan.
Introduction
Chronic Lymphocytic Leukemia is a clonal lymphoid disease characterized by progressive accumulation of small CD5/CD19/CD23-positive lymphocytes in the blood, lymph nodes, spleen, liver and bone marrow [1]. The clinical course and prognosis of patients with B-cell chronic lymphocytic leukemia display a marked heterogeneity [2]. The asymptomatic disease is seen in about 25% of patients [2]. Physical examination revealed lymphadenopathy, splenomegaly, and hepatomegaly in approximately 85%, 50%, and 14% of the patients, respectively [2]. Autoimmune complications, primarily hemolytic anemia and thrombocytopenia, occur in up to 25% of the CLL patients [3]. Two staging systems that have been proposed for CLL have led to significant progress in predicting survival and in planning therapeutic schedules [4, 5].
For many years, the diagnosis of CLL was made based on morphologic examination of the peripheral blood smear, which demonstrates mature lymphocytes with an abundance of smudge cells. Despite rigorous morphology, many diseases can mimic CLL in both appearance and clinical presentation, resulting in incorrect diagnosis [6]. In recent years, the World Health Organization classified tumors in Hematopoietic and lymphoid tissues based on immunophenotype by Flow Cytometry [7]. The International Workshop of Chronic Lymphocytic Leukemia in 2008 require a peripheral blood B-cell count ≥5×10 9/L to diagnosis CLL and the presence of monoclonal (kappa or lambda) B-cells which have typical Immunophenotype of CLL cells (CD19+, CD5+, CD23+ and decreased expression of surface Ig, CD20, and CD79b) [1].
CLL is a quite heterogeneous disease (both morphologically and immunophenotypically), which makes diagnosis difficult [8, 9]. However, to help discriminate between CLL and other lymphoproliferative disorders, by using international scoring systems which depending on phenotypic marker expression [8, 9].
To the best of our knowledge, this is the first study with a large sample size make comprehensive describe the clinical presentation, hematological profile, and immunophenotype pattern in Sudanese patients with CLL. The objective of this study was to characterize the clinical presentation, hematological profile, and immunophenotype pattern in Sudanese patients with CLL.
Materials and Methods
Study Population
This study was a prospective cross-sectional descriptive study, conducted in Khartoum state, Sudan, in the period from 10 April 2017 to 10 April 2018. A total of 110 blood samples were collected from patients with CLL. Patients were referred to Flow Cytometry Laboratory for Leukemia & Lymphoma Diagnosis Center, for immunophenotypic diagnosis.
All patients were diagnosed based on clinical history, physical examination, and complete blood count. Peripheral blood, immunophenotypic criteria, and B lymphocytes count ≥5×109/l, according to the IWCLL [1]. The stage of the CLL was assessed by Rai and Binet [4, 5] classification. All patients were newly diagnosed without any previous CLL treatment. Patients with other lymphoid neoplasms (Both B and T-cell lineages) were excluded.
Blood count
Two ml of peripheral blood were withdrawn from each patient, collected in EDTA tubes, and preserved at room temperature (22-24℃). All samples were processed within 6-24h from the collection. Complete Blood Count was performed by using automated hematology analyzer (SYSMEX KX-21N, Japan), Total WBC, Absolute Lymphocyte Count, Hemoglobin level, RBC and Platelets Count were recorded.
Immunophenotyping
The diagnosis of CLL was confirmed for each patient by Flow Cytometry (EPICS XL Beckman Coulter Flow Cytometer, Miami, FL, USA), standard protocol of Beckman Coulter was used in fluorescent dye-labeled monoclonal antibody for CD45, CD5, CD3, CD19, CD20, CD22, CD23, FMC7, CD79b, kappa, lambda light chain, CD38, and ZAP-70 (Immunostep-Spain).
A marker was considered positive at a cutoff level of ≥ 30%. as recommended by the British Committee for Standards in Haematology guideline [10]. Depending on Matutes et al., [8], score system allocates one point for each following marker expression CD5, CD23, weak SmIg, absent or low expression of CD22 and FMC7. By replacing CD22 with CD79b Moreau et al., [9] score system was assessed. The scoring system, however, was defined as ≥ 30% cell surface expression.
Absolute counts of peripheral blood B-cells and T-cells were calculated by using double platform methodology [11]. Proportions of peripheral blood B-cells (percentage of CD19+ cells/ lymphocytes) and T-cells (percentage of CD3+ cells/lymphocytes), detected by Flow Cytometry, were combined with the absolute leukocyte count and lymphocyte differential. Light chain restriction (marker of clonality) was defined by an abnormal kappa-lambda ratio > 3:1 (kappa restricted) or >2 (lambda restricted) [12, 13].
Statistical analysis
Data was analyzed using the SPSS version 23.0 (Chicago, IL, USA). Numerical data were summarized as mean and standard deviation and n (%) of study participants, respectively. Chi-Square test and Fisher‘s exact test were used for analyzing associations between categorical variables (Fisher‘s exact test was used when ˃ 20% of cells have expected count < 5). An independent t-test and One-Way ANOVA were used to compare the means of two groups. All P-values were two-sided, and < 0.05 was considered as the significance level.
Results
Out of 110 patients, 71.8% were males while 28.2% were females (M/F ratio, 2.55:1) (Table 1).
| Characteristic | No. of cases | Percentage % |
| Age (n=110) | ||
| ≥63 (mean age) | 62 | 56 |
| <63 (mean age) | 48 | 44 |
| Gender (n=110) | ||
| Male | 79 | 71.8 |
| Female | 31 | 28.2 |
| Binet Stage (n=110) | ||
| A | 33 | 30 |
| B | 35 | 31.8 |
| C | 42 | 38.2 |
| Rai Stage (n=110) | ||
| 0 | 10 | 9.1 |
| I | 23 | 20.9 |
| II | 23 | 20.9 |
| III | 36 | 32.7 |
| IV | 18 | 16.4 |
| CD38 (n=110) | ||
| <30% | 69 | 62.7 |
| ≥30% | 41 | 37.3 |
| ZAP70 (n=110) | ||
| <20% | 74 | 67.3 |
| ≥20% | 36 | 32.7 |
| Combined ZAP-70/CD38 (n=110) | ||
| Concordant –ve | 53 | 48.2 |
| Discordant | 37 | 33.6 |
| Concordant +ve | 20 | 18.2 |
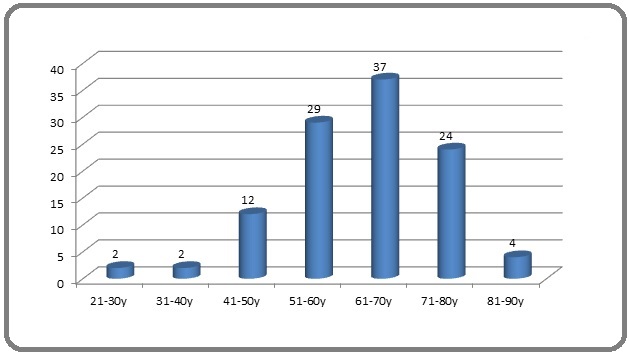
The mean age at the time of diagnosis was 62.97±12.06 years (range 22-85y). Mean age for males was 63.77±12.33 years and for females 60.93±11.26 years and there are no significant difference in mean age between the sexes (p≤0.269). The most common age group was 61-70 years 33.6% (Figure 1).
Figure 1. Age Distribution at Diagnosis.
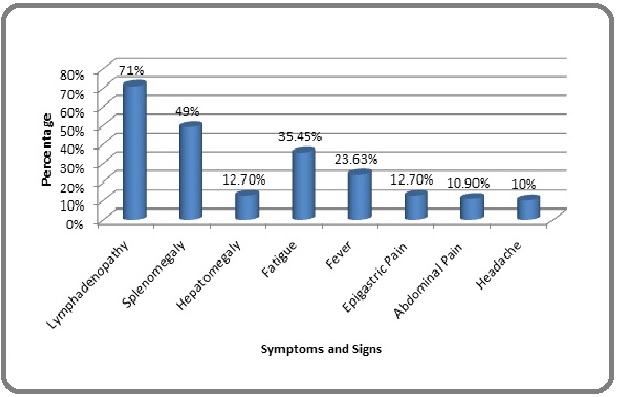
Fatigue was the most common presenting symptom in 35.45% patients followed by fever, epigastric pain, abdominal pain and headache. On the other hand, lymphadenopathy was the most presenting sign (Figure 2).
Figure 2. Frequency of the Most Presenting Symptoms and Signs in Chronic Lymphocytic Leukemia Patients.
The distribution of patients according to Rai stage system was 9.1% patients at stage 0, 20.9% patients at stage I, 20.9% patients at stage II, 32.7% patients at stage III, and 16.4% patients at stage IV. Regarding Binet staging system, 30% patients presented with stage A, 31.8% patients with stage B and 38.2% patients with stage C (Table 1).
Mean white blood cell count was 92.86 ±75.43×103/ul, absolute lymphocyte counts was 82.23±70.88×103/ul, B lymphocyte count was 75.16±68.20×103/ul, T lymphocyte was 4.81±5.58×103/ul, Mean hemoglobin level was 11.2±2.5g/dL and Mean platelet count was 189.24 ±104.91×103/ul. More details about hematological parameters in (Table 2).
| Parameter | Mean | Median | Minimum | Maximum |
| TWBC×10 3 /ul | 92.86 | 67.75 | 9.7 | 350.7 |
| RBCs×10 6 /ul | 3.7 | 3.85 | 1.19 | 6.18 |
| Platelets×10 3 /ul | 189.24 | 172 | 13.7 | 587 |
| Hemoglobin (g/dl) | 11.15 | 11.05 | 4.4 | 18.1 |
| Relative Granulocytes% | 12.33 | 12 | 1 | 35 |
| Relative Monocytes% | 2.6 | 2 | 0 | 10 |
| Relative Lymphocytes% | 85.07 | 86 | 60 | 98 |
| Absolute Lymphocyte×10 3 /ul | 82.23 | 56.68 | 7.76 | 325.5 |
| Absolute B Lymphocyte×10 3 /ul | 75.16 | 49.98 | 7.29 | 302.06 |
| Absolute T Lymphocyte×10 3 /ul | 4.81 | 3.81 | 0.23 | 52.04 |
A limited panel of antibodies was used, which includes CD45, CD3, CD5, CD19, CD20, CD22, CD79b, CD23, FMC7, kappa, and lambda. All CLL samples expressed CD45 with the mean positivity of 87.53±9.2% (range: 53.9-98.7%). All the 110 CLL samples have demonstrated a population of B lymphocytes (CD19+, CD20+) with mean positivity 87.92% and 85.66%, respectively. All the CLL cases were negative for the T-cell marker CD3. CD5 was expressed in 88 (80%) patients with overall mean positivity 74.60±32.9%; CD23 was expressed in 102 (92.7%) patients with overall mean positivity 75.38±21.3%. CD22 was negative in 91.8% patients. CD79b was negative in 77.3% patients. FMC7 was negative in 96.4% patients (Table 3).
| Marker | % (n/N) | Mean± SD (%) |
| CD45 | 100 (110/110) | 87.53±9.2 |
| CD3 | 0 (0/110) | 8.31±6.5 |
| CD5 | 80 (88/110) | 74.60±32.9 |
| CD19 | 100 (110/110) | 87.92±8.0 |
| CD20 | 100 (110/110) | 85.66±8.1 |
| CD22 | 8.2 (9/110) | 11.01±16.8 |
| CD23 | 92.7 (102/110) | 75.38±21.3 |
| CD79b | 22.7 (25/110) | 21.89±25.1 |
| FMC7 | 3.6 (4/110) | 6.99±13.0 |
| Kappa | 6.36 (7/110) | 8.72±18.65 |
| Lambda | 4.5 (5/110) | 5.71±16.46 |
n- number of patients that are positive for the analyzed antigen; N-total number of the analyzed patients.
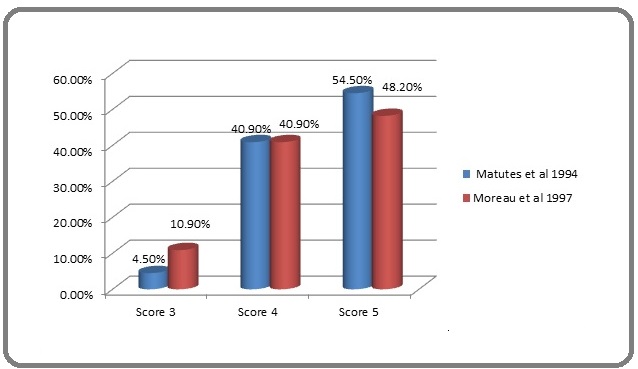
According to the Matutes scoring system; the frequencies of scores 5, 4 and 3 were 54.5%, 40.9%, and 4.5% respectively. Regarding the Moreau scoring system; the frequencies of scores 5, 4 and 3 were 48.2%, 40.9% and 10.9%, respectively (Figure 3).
Figure 3. Frequency of Scoring Systems Depending on Matutes et al and Moreau et al in CLL Patients.
Discussion
CLL is a heterogeneous disorder characterized by variable clinical course; the disease is the most common form of adult leukemia in Western countries and is rare in Asian countries [7].
In this cross-sectional study male to female ratio was 2.55:1. A nearly similar as ratio was previously reported [14, 15]. The higher male/female ratios in these studies may be due to high exposure to environmental and occupational hazards. In previous studies were reported that smoking [16] and quality of life [17] influence on development of CLL.
The mean age of our patients at diagnosis was 63 years. Nearly similar results (62, 62, 61 and 60 years) were reported in Sudan [18], Kenya [19], Senegal [20], and Nigeria [21], respectively. Other studies in Nigeria [22] and Ethiopia [23] revealed lower mean ages at diagnosis of 56 and 55 years, respectively. All previous studies in different regions in Africa revealed lower mean age than in Western countries [1, 7, 24]. In this study, Lymphadenopathy is the most common presenting finding, followed by the Splenomegaly, and Hepatomegaly. These findings differed from those in studies conducted by Salawu et al. [21] and Agrawal et al.,[25] who found that splenomegaly predominated amongst other organ enlargements. In this study, about 90% of patients displayed advanced Rai stages and 70% were at Binet stage B or C. Similar frequencies were reported by Ahmed and Osman [15] in Sudan and Gogia et al., [26] in India. As expected, reverse patterns with highest patient percentages at stage (Rai 0 and Binet A) and lowest percentages at advanced stages (III, IV and C) were reported in developed countries by Mauro et al., [27] in Italy and Apelgen et al., [28] in Sweden. In this study did not find a significant association between men and women compared to Rai and Binet stages (P-values of 0.051 and 0.213, respectively), our results were consistent with those of Ahmed and Osman [15], Sall et al., [20], and Mulwa et al., [19]. By contrast, Catovsky et al., [29] demonstrated that CLL ran a more benign clinical course in women than in men. Women were more likely to have Binet stage A than B or C. Furthermore, In this study did not find a significant association between mean age compared to Rai and Binet stages, these results were consistent with Sall et al., [20].
Mean total white blood cell count and mean absolute lymphocytes count in this study were 92.86×103/ul and 82.23×103/ul, respectively. In contrast, Higher mean total white blood cell count and mean absolute lymphocytes were by Salawu et al., [21] from Nigeria and Mohammed and Osman [15] in Sudan (111×103/ul, 103×103/ul) and (107×103/ul, 87×103/ul), respectively, whereas two studies in India revealed that relatively low mean total white blood cell count and mean absolute lymphocytes (50×103/ul, 41×103/ul, respectively) by Gogia et al., [26] and (70×103/ul, 51×103/ul, respectively) by Agrawal et al., [25]. This variation may be due to the advanced stage at presentation, and patients avoid medical consultation and ignore general health practices. Shvidel et al., [30] demonstrated that CLL patients with hyperleukocytosis at diagnosis generally had an aggressive clinical course.
Absolute lymphocyte counts and percentage of lymphocytes in our patients were higher than the normal range in healthy Sudanese population [31]. The analysis of the relative distribution of B-cells and T-cells in lymphocyte population showed that higher mean of B-cells as well as the lower mean proportion of T-cells, compared to normal ranges in healthy Sudanese population [31].
This study showed that the expression of CD19 occurred in all CLL patients, which was the same as that in other studies [31-35].
CD5 was expressed in 80% of diagnosed CLL patients. While, 20% of CLL patients were negative CD5, which agrees with studies found the expression of CD5- in CLL varied from 7 to 20% [13, 36-38]. In a few studies by Rame Khasawneh et al., [31], Ivancevic et al., [33], and Deneys et al., [39] the expression levels of 99%, 99%, and 98%were detected.
In the current study, CD23 was expressed in 92.7% patients, which agreed with the finding of Rame Khasawneh et al., [31] who showed CD23 positivity in 93%. DiRaimondo et al., [40] found the expression in nearly 94% of CLL patients. The results obtained by Geisler et al., [13] considered 30% cut-off for CD23 expression in 71% of cases. On the contrary, Ahmad et al., [41]and Ivancevic et al., [33] reported higher expression levels of 100% and 98%, respectively. Earlier studies have reported that CD23 is a reliable marker in the distinction between CLL and MCL [33, 41]. According to the results of recent studies, CD23 alone is insufficient to make a differential diagnosis between CLL and MCL.
FMC7 antigen is considered a reliable marker for differential diagnosis of CLL; this antigen can also be used to distinguish between CLL from other MBCN [41, 42]. Our results showed that only 3.6% of CLL patients expressed FMC7, which agreed with results of El-Sewefy et al., [34], Rame Khasawneh et al., [31], and Ivancevic et al.,[33] who reported FMC7 expression in 0%, 8% and 8% of patients, respectively. Furthermore, some studies have shown a wide frequency range of FMC7 (12%–42%) positive in CLL cases [13, 14, 39, 42].
The CD22 expression in our CLL patients was detected in 8.2% patients. A nearly similar result was found in a previous study conducted in Sudan, which found that only 7% of CLL patients expressed CD22 [38]. Another report in Kenya revealed a nearly similar result [19]. Higher expression was reported by different reports [13, 14, 33, 34], with values of 42%, 47%, 86% and 94%, respectively. Our result and that of a previous study in Sudan revealed low expression of CD22 in CLL Sudanese patients.
CD79b is an antigen that was incorporated into the CLL scoring system [9]. In this study CD79b was positive in 22.7% patients. This result was consistent with the previous study in Sudan which found 29% of CLL patients had expressed CD79b [38]. Our result also agreed with that of a previous study reported by Schlette et al, who found that 18% of CLL patients expressed CD79b [43]. The expression levels of CD79b in different studies differed with values that ranges from 37%-82% [14, 31, 33, 34, 44]. Our result and that of a previous study in Sudan revealed low expression of CD79b in CLL Sudanese patients.
Amongst 110 CLL patients, 77.3% patients expressed κ immunoglobulin light chain and 22.7% expressed λ light chain. The frequency of sIgκ+ was higher than that of sIgλ+ cases (a ratio of 3.4:1). Our result was consistent with that of previous studies that showed higher expression of κ immunoglobulin light chain than that of λ light chain [45, 46]. Surface Ig light chains were undetectable in 2.7% of our patients. Surface Ig negative CLL has been reported by many studies with a variable percentage that ranges from 0% to 23.3% [19, 32, 33, 47, 48].
By replacing CD22 with CD79b, improved Moreau et al. scoring system was applied. In this study revealed (89% of patients had score 4 or 5 and 11% of patients had score 3). [9]. A similar distribution was found in the previous results reported by Moreau et al., [9]. This finding was opposite to that reported by by Falay and Özet [14] who who found that 60% scored 3.
Furthermore, a previous work conducted by Altayeb in Sudan revealed the sensitivity and specificity of the CD22 marker of 60.1% and 93.4%, respectively [38]. In the meantime, the sensitivity and specificity of the CD79b marker were 76.4% and 62.6%, respectively, in the differentiation between CLL and NHL. This finding indicated that the CD22 marker was highly specific in distinguishing between CLL and NHL in Sudanese patients. This result was also consistent with our findings that showed a highly typical CD22 expression in our patients. On the contrary, Moreau et al. revealed higher accuracy of CD79b 91.8% markers than CD22 82.1% in the differential diagnosis of CLL versus NHL [9].
In conclusion, CLL in Sudan is a disease of the elderly according to mean age, and more frequently in males than females. The incidence at young patients was higher than those reported by Western studies. Most of our patients presented advanced Rai and Binet stages. CD22 may be a highly specific marker for diagnosing CLL in Sudanese patients and should be included in all diagnostic panels used to differentiate CLL from other B cell lymphoproliferative disorders in Sudan.
Acknowledgments
We would like to thank the staff of the Hematology Department at Al Neelain University for facilities and supporting and we are grateful to the staff of Flow Cytometry Laboratory for Leukemia & Lymphoma for their collaboration. Finally special thanks to the patients for being cooperative, despite their pains.
Availability of data and materials
The individual data are available in the archives of the Flow Cytometry for Leukemia & Lymphoma Diagnosis, Khartoum, Sudan and can be obtained from the corresponding author on request.
Ethics approval and consent to participate
Ethical clearance was obtained from the Institutional Review Board at Al Neelain University. The principal investigator obtained written informed consent from all participants prior to their inclusion in the study.
Funding
The research did not receive any funds or financial support.
References
- Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Döhner H, Hillmen P, Keating MJ , Montserrat E, Rai KR , Kipps TJ . Blood.2008;111(12). CrossRef
- Mature B-cell neoplasm. In: Naeim F, Rao PN, Grody WW, editors. Hematopathology : morphology, immunophenotype, cytogenetics, and molecular approaches 1st ed. London: Academic; Naeim F, P R , W G . 2008;:297-372.
- Autoimmune complications of chronic lymphocytic leukemia Hamblin Terry J.. Seminars in Oncology.2006;33(2). CrossRef
- Clinical staging of chronic lymphocytic leukemia Rai K. R., Sawitsky A., Cronkite E. P., Chanana A. D., Levy R. N., Pasternack B. S.. Blood.1975;46(2).
- A new prognostic classification of chronic lymphocytic leukemia derived from a multivariate survival analysis Binet J. L., Auquier A., Dighiero G., Chastang C., Piguet H., Goasguen J., Vaugier G., Potron G., Colona P., Oberling F., Thomas M., Tchernia G., Jacquillat C., Boivin P., Lesty C., Duault M. T., Monconduit M., Belabbes S., Gremy F.. Cancer.1981;48(1). CrossRef
- Chronic Lymphocytic Leukemia. In: Hoffman R, Benz Jr EJ, Silberstein LE, Heslop H, Anastasi J, Weitz J, editors. Hematology: basic principles and practice Elsevier Health Sciences; 2013 Thomas SL , Farrukh T, Awan , Byrd aJC . .
- WHO classification of tumours of haematopoietic and lymphoid tissues. In: Bosman FT JE, Lakhani SR OH, editors Swerdlow SH, E C , Harris NL. WHO classification of tumours. 22008. 4th ed. Lyon, France: IARC.2008;:439.
- The immunological profile of B-cell disorders and proposal of a scoring system for the diagnosis of CLL Matutes E., Owusu-Ankomah K., Morilla R., Garcia Marco J., Houlihan A., Que T. H., Catovsky D.. Leukemia.1994;8(10).
- Improvement of the chronic lymphocytic leukemia scoring system with the monoclonal antibody SN8 (CD79b) Moreau E. J., Matutes E., A'Hern R. P., Morilla A. M., Morilla R. M., Owusu-Ankomah K. A., Seon B. K., Catovsky D.. American Journal of Clinical Pathology.1997;108(4). CrossRef
- Guidelines on the diagnosis, investigation and management of chronic lymphocytic leukaemia Oscier D, Dearden C, Eren E, Erem E, Fegan C, Follows G, Hillmen P, Illidge T, Matutes E, Milligan DW , Pettitt A, Schuh A, Wimperis J. British Journal of Haematology.2012;159(5). CrossRef
- Flow cytometry: new guidelines to support its clinical application D'Archangelo M. Cytometry. Part B, Clinical Cytometry.2007;72(3). CrossRef
- Diagnostic value of clonality of surface immunoglobulin light and heavy chains in malignant lymphoproliferative disorders Batata A., Shen B.. American Journal of Hematology.1993;43(4). CrossRef
- Prognostic importance of flow cytometric immunophenotyping of 540 consecutive patients with B-cell chronic lymphocytic leukemia Geisler C. H., Larsen J. K., Hansen N. E., Hansen M. M., Christensen B. E., Lund B., Nielsen H., Plesner T., Thorling K., Andersen E.. Blood.1991;78(7).
- Immunophenotyping of Chronic Lymphocytic Leukemia Falay M, Özet G. Clinical Laboratory.2017;63(10). CrossRef
- Clinical and Haematological Pattern of Chronic Lymphocytic Leukaemia in Sudanese Patients Ahmed R, Osman I. International Blood Research & Reviews.2017;7. CrossRef
- Mortality and cancer incidence following occupational radiation exposure: third analysis of the National Registry for Radiation Workers Muirhead C R, O'Hagan J A, Haylock R G E, Phillipson M A, Willcock T, Berridge G L C, Zhang W. British Journal of Cancer.2009;100(1). CrossRef
- The physician-patient relationship and quality of life: lessons from chronic lymphocytic leukemia Shanafelt TD , Bowen DA , Venkat C, Slager SL , Zent CS , Kay NE , Reinalda M, Tun H, Sloan JA , Call TG . Leukemia Research.2009;33(2). CrossRef
- Evaluation of CD38 expression in Sudanese patients with chronic lymphocytic leukemia Abdelgader EA , Eltayeb NH , Eltahir TA , Altayeb OA , Fadul EA E, Abdel Rahman EM , Merghani TH . BMC research notes.2018;11(1). CrossRef
- Chronic lymphocytic leukemia in Kenya: an immunophenotypic and clinicopathologic study Mulwa-Babu E., Paresh D., Riyat M.. J. Afr. Cancer.2013;5.
- Characteristics of chronic lymphocytic leukemia in Senegal Sall A, Touré AO , Sall FB , Ndour M, Fall S, Sène A, Faye BF , Seck M, Gadji M, Dièye TN , Mathiot C, Reynaud S, Diop S, Raphaël M. BMC hematology.2016;16. CrossRef
- Chronic lymphocytic leukaemia: a-twenty-years experience and problems in Ile-Ife, South-Western Nigeria Salawu L., Bolarinwa R. A., Durosinmi M. A.. African Health Sciences.2010;10(2).
- Chronic lymphoid leukaemia: clinico-haematological correlation and outcome in a single institution in Niger Delta region of Nigeria Omoti C. E., Awodu O. A., Bazuaye G. N.. International Journal of Laboratory Hematology.2007;29(6). CrossRef
- Chronic lymphocytic leukaemia in Ethiopians Shamebo M., Gebremedhin A.. East African Medical Journal.1996;73(10).
- High incidence of chronic lymphocytic leukemia (CLL) diagnosed by immunophenotyping: a population-based Canadian cohort Seftel M. D., Demers A. A., Banerji V., Gibson S. B., Morales C., Musto G., Pitz M. W., Johnston J. B.. Leukemia Research.2009;33(11). CrossRef
- Chronic lymphocytic leukemia in India--a clinico-hematological profile Agrawal N, Naithani R, Mahapatra M., Panigrahi I, Kumar R, Pati H. P., Saxena R, Choudhary V. P.. Hematology (Amsterdam, Netherlands).2007;12(3). CrossRef
- Assessment of 285 cases of chronic lymphocytic leukemia seen at single large tertiary center in Northern India Gogia A, Sharma A, Raina V, Kumar L, Vishnubhatla S, Gupta R, Kumar R. Leukemia & Lymphoma.2012;53(10). CrossRef
- Clinical characteristics and outcome of young chronic lymphocytic leukemia patients: a single institution study of 204 cases Mauro F. R., Foa R., Giannarelli D., Cordone I., Crescenzi S., Pescarmona E., Sala R., Cerretti R., Mandelli F.. Blood.1999;94(2).
- Evaluation of clinical staging in chronic lymphocytic leukemia- population-based study Apelgren P, Hasselblom S, Werlenius O, Nilsson-Ehle H, Andersson P. Leukemia & Lymphoma.2006;47(12). CrossRef
- The clinical significance of patients' sex in chronic lymphocytic leukemia Catovsky D, Wade R, Else M. Haematologica.2014;99(6). CrossRef
- Absolute lymphocyte count with extreme hyperleukocytosis does not have a prognostic impact in chronic lymphocytic leukemia Shvidel L, Bairey O, Tadmor T, Braester A, Ruchlemer R, Fineman R, Joffe E, Berrebi A, Polliack A. Anticancer Research.2015;35(5).
- Flow Cytometric Pattern In Diagnosis Of Chronic Lymphocytic Leukemia, King Hussein Medical Center Experience ejpmr Rame Khasawneh F, Hala Alsokhni , Bayan Alzghoul , Nabeeha Abbasi , Asim Momani , Nazmi Kamal . 2017;4(04):511-514.
- Immunophenotypic characterization of the leukemic B-cells from Iranian patients with chronic lymphocytic leukemia: Association between CD38 expression and disease progression Hojjat-Farsangi M, Jeddi-Tehrani M, Razavi S, Sharifian R, Khoramabadi A, Rabbani H, Shokri F. Iranian journal of immunology : IJI.2008;5.
- The role of immunophenotyping in differential diagnosis of chronic lymphocytic leukemia Ivancević TD , Kurtović NK , Knezević V, Bogdanović A, Mihaljević B, Bozić B, Gotić M. Srpski Arhiv Za Celokupno Lekarstvo.2014;142(3-4). CrossRef
- Flow cytometric evaluation of CD200 as a tool for differentiation between chronic lymphocytic leukemia and mantle cell lymphoma El-Sewefy DA , Khattab DA , Sallam MTH , Elsalakawy WA . The Egyptian Journal of Haematology.2014;39(2). CrossRef
- Chronic lymphoproliferative disorders at an Indian tertiary cancer centre - the panel sufficiency in the diagnosis of chronic lymphocytic leukaemia Okaly GVP , Nargund AR , Venkataswamy E, Jayanna PK , Juvva CR , Prabhudesai S. Journal of clinical and diagnostic research: JCDR.2013;7(7). CrossRef
- Immunophenotypic subclassification of chronic lymphocytic leukaemia (CLL) Kurec A. S., Threatte G. A., Gottlieb A. J., Smith J. R., Anderson J., Davey F. R.. British Journal of Haematology.1992;81(1). CrossRef
- CD5 negative lymphocytosis mimicking typical B-chronic lymphocytic leukaemia. Description of 26 cases De Rossi G., Mauro F. R., Lo Coco F., Caruso R., Niscola P., Pasqualetti D., Mandelli F.. Nouvelle Revue Francaise D'hematologie.1993;35(4).
- Flow Cytometric Immunophenotyping of Mature B-cell Neoplasm in Adult Sudanese Patients: Sudan University of Science and Technology; 2013 Altayeb OAM . .
- Atypical lymphocytic leukemia and mantle cell lymphoma immunologically very close: flow cytometric distinction by the use of CD20 and CD54 expression Deneys V., Michaux L., Leveugle P., Mazzon A. M., Gillis E., Ferrant A., Scheiff J. M., De Bruyère M.. Leukemia.2001;15(9). CrossRef
- The clinical and diagnostic relevance of CD23 expression in the chronic lymphoproliferative disease DiRaimondo F, Albitar M, Huh Y, O'Brien S, Montillo M, Tedeschi A, Kantarjian H, Lerner S, Giustolisi R, Keating M. Cancer.2002;94(6). CrossRef
- Clinical utility of CD23 and FMC7 antigen coexistent expression in B-cell lymphoproliferative disorder subclassification Ahmad E, Garcia D, Davis BH . Cytometry.2002;50(1).
- Diagnostic significance of CD20 and FMC7 expression in B-cell disorders Delgado J, Matutes E, Morilla AM , Morilla RM , Owusu-Ankomah KA , Rafiq-Mohammed F, Giudice I, Catovsky D. American Journal of Clinical Pathology.2003;120(5). CrossRef
- CD79b expression in chronic lymphocytic leukemia. Association with trisomy 12 and atypical immunophenotype Schlette E, Medeiros LJ , Keating M, Lai R. Archives of Pathology & Laboratory Medicine.2003;127(5). CrossRef
- Expression of CD79b, CD25 and CD100 molecules on B cells in chronic lymphocytic leukemia (B-CLL) Ekspresja molekuł CD79b, CD25 i CD100 na komórkach B w przewlekłej białaczce limfocytowej (PBL-B). 2012 Kopeć-Szlęzak J, Podstawka U, Gajewska A, Sikorska A. .
- Immunoglobulin light chain repertoire in chronic lymphocytic leukemia Stamatopoulos K, Belessi C, Hadzidimitriou A, Smilevska T, Kalagiakou E, Hatzi K, Stavroyianni N, Athanasiadou A, Tsompanakou A, Papadaki T, Kokkini G, Paterakis G, Saloum R, Laoutaris N, Anagnostopoulos A, Fassas A. Blood.2005;106(10). CrossRef
- Surface antigen expression in chronic lymphocytic leukemia: clustering analysis, interrelationships and effects of chromosomal abnormalities Hulkkonen J., Vilpo L., Hurme M., Vilpo J.. Leukemia.2002;16(2). CrossRef
- Surface and cytoplasmic immunoglobulin expression in B-cell chronic lymphocytic leukemia (CLL) Lewis RE , Cruse JM , Pierce S, Lam J, Tadros Y. Experimental and Molecular Pathology.2005;79(2). CrossRef
- Flow cytometric analysis of surface light chain expression patterns in B-cell lymphomas using monoclonal and polyclonal antibodies Horna P, Olteanu H, Kroft SH , Harrington AM . American Journal of Clinical Pathology.2011;136(6). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times