Indications, Surgical Techniques and Results of Breast Oncoplasty in West Africa, Case of Burkina Faso
Download
Abstract
Objective: To describe the indications, surgical techniques and results of breast oncoplasty.
Patients and methods: Retrospective and descriptive study of oncoplastic breast surgery performed between January 2013 and March 2021. We were interested in the indications, techniques, and aesthetic and oncological results. Overall survival was assessed by the Kaplan Meier technique and survival comparisons by logRank. Aesthetic results and quality of life were assessed by the modified BREAST-Q questionnaire.
Results: We report 64 cases of oncoplastic breast surgery in Ouagadougou, that is 6.9% of the 917 surgeries performed for breast cancers. We performed 14 Round Block for upper quadrant carcinomas. Eight external oncoplasties were performed for infiltrating ductal carcinomas of the external quadrants. The upper pedicle technique was performed in 19 cases and the Thorek amputation graft technique in 13 cases for lower quadrant carcinomas with macromastia and major ptosis. The supero-postero-internal pedicle technique help to avoid necrosis and amputation of the nipple in 8 cases. The 5-year overall survival was 90.5%. The patients were satisfied with the volume of the remaining breasts and their aesthetic appearance.
Conclusion: Oncoplasty is increasingly performed in Burkina Faso. It should take its place with the recent advent of radiotherapy in our country. A larger cohort will better describe its results.
Introduction
Breast cancers are the most common cancers in the world [1]. They represent 55% of gynecologic and breast cancers and 21% of all cancers in Burkina Faso [2]. Their frequency is constantly increasing and they keep the particularity of occurring in young patients in Africa [3-5]. Surgery remains the essential curative treatment. This surgery has undergone an important evolution since the first modern description by Halsted in 1889 [6]. Radical mastectomy is mutilating and a consequence of refusal of treatment, even depression [7]. This has prompted surgeons to develop less mutilating techniques [8, 9].
Surgical oncology has therefore become less and less extensive without compromising oncological safety [8, 9]. Indeed, with the advent of radiotherapy, breast cancer surgery has become more and more conservative [8, 9]. This results in a permanent concern to leave aesthetically acceptable breasts in place [10]. This gave birth to a subspecialty of oncology borrowing plastic surgery techniques, it is oncoplastic breast surgery. Commonly practiced in Europe, in the treatment of breast cancer, oncoplasty is still in its onset in West Africa, more particularly in Burkina Faso. Indeed, diagnostic delays and the inaccessibility of radiotherapy further reduce the scope for conservative surgery [7]. However, demand is growing, pushing surgeons to perform conservative surgery with the use of oncoplastic technique upon radiotherapy outside Burkina Faso [7]. Burkina Faso has just completed the construction of its first radiotherapy centre and oncoplasty should take off as soon as this centre begins to operate. This work aims to describe the first steps of oncoplastic breast surgery in Burkina Faso through its indications, techniques, difficulties and results.
Materials and Methods
Patients
Type and period of study: This was a retrospective and descriptive study of breast oncoplastic surgery carried out between January 2013 and March 2021.
Study setting: Our study took place in Burkina Faso. The surgical departments of the teaching hospital Yalgado Ouédraogo and the Schiphra hospital served as our study framework.
Study population: The study population consisted of records of patients followed for mammary carcinomas treated by conservative surgery with oncoplasty.
Sampling / sample: We carried out a simple exhaustive collection of all cases of breast carcinoma treated by oncoplastic breast surgery in the surgical departments of the teaching hospital of Yalgado Ouédraogo and the Schiphra hospital during the study period.
Study variables: We were interested in civil status, cancer stage, indications for oncoplastic breast surgery, techniques used, oncological and aesthetic results.
Data collection: The collection was done with a pre-established individual sheet. Patient charts, pathological anatomy registers and surgeries reports were used as data sources. The patients were also seen again in consultation.
Data analysis: Patients were reviewed systematically the 5 th postoperative day, 1 month, then every three months for 2 years, then every 6 months for 3 years. Survival was assessed by Kaplan Meier technique with IBM SPSS 26.0.0.0 software. For the evaluation of cosmetic results and the impact in terms of quality of life of our patients, the pre and postoperative questionnaires used complied with the modified BREAST-Q questionnaire.
Ethical considerations: This study was carried out with the authorization of hospital directors and heads of department. Anonymity and confidentiality of data were respected for all patients.
Results
We report 64 cases of oncoplastic surgery, that is 6.9% of the 918 surgeries performed for breast cancer over the past 9 years. The mean age of the patients was 44 +/- 15.2 years with extremes of 21 and 62 years (Table 1). The size of tumor was less than or equal to 2 cm in 63.3%. Infiltrating ductal carcinomas represented 84.4% of cases (Table 1).
| Number | Percentage % | |
| Age of patients (years) | ||
| [20-40] | 40 | 62.5 |
| [40-60] | 23 | 35.9 |
| [60-80] | 1 | 1.6 |
| Total | 64 | 100 |
| Topography of cancers | ||
| Inferior-internal quadrant | 20 | 31.3 |
| Infero-external quadrants | 18 | 28.1 |
| Superior-internal quadrant | 7 | 10.9 |
| Superior-external quadrant | 7 | 10.9 |
| Union of the upper quadrants | 1 | 1.6 |
| Union of outer quadrants | 9 | 14.1 |
| Union of internal quadrants | 2 | 3.1 |
| Total | 64 | 100 |
| Size of tumors | ||
| T1 | 40 | 62,5 |
| T2 | 14 | 21.9 |
| T3 | 10 | 15.6 |
| Total | 64 | 100 |
| Histological type | ||
| Ductal carcinoma in situ | 8 | 12.5 |
| Invasive ductal carcinoma | 54 | 84.4 |
| Intracanal papilloma | 2 | 3.1 |
| Total | 64 | 100 |
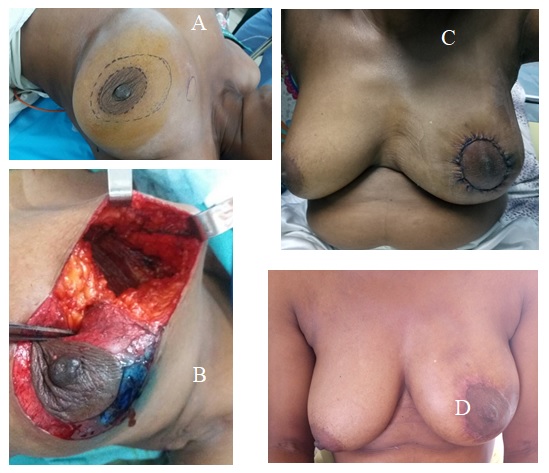
The tumors were located in the infero-internal quadrant in 31.3% of cases (Table 1). We performed 14 Round Block for carcinomas in situ (8 cases) and invasive (4 cases) of the upper quadrants (Figure 1).
Figure 1. Oncoplasty Using the Round Block Technique. A, Preoperative drawing of the patient in supine position. B, View after resection up to the plane of the pectoralis major. C, Breast Appearance at 3rd day post-operative. D, Appearance of the breast six months after radiotherapy.
Two other Round Block were performed for two intracanal mammary papillomas of the union of the upper quadrants and of the union of the internal quadrants with bloody nipple discharge (Tables 2).
| Indications/ Techniques | Round block | Upper pedicle | Lateral oncoplasty | Thorek | Techniques Saint Louis | Techniques Combined |
| Carcinoma in situ SQ | 12 | 0 | 0 | 0 | 0 | 0 |
| SQ ICNT | 0 | 0 | 0 | 0 | 0 | 0 |
| EQ ICNT | 0 | 0 | 8 | 0 | 0 | 0 |
| ICNT lower Q | 0 | 18 | 0 | 0 | 7 | 0 |
| ICNT lowers Q + ptosis + macromastia | 0 | 0 | 0 | 13 | 0 | 0 |
| ICNT of the internal Q | 0 | 0 | 0 | 0 | 0 | 1 |
| Intracanal papillomas | 2 | 0 | 0 | 0 | 0 | 0 |
| Reduction of remaining breast | 0 | 1 | 0 | 0 | 1 | 0 |
| ICNT Bilateral | 0 | 0 | 0 | 0 | 0 | 1 |
| Total | 14 | 19 | 8 | 13 | 8 | 2 |
ICNT, Invasive carcinoma of nonspecific type; Q, Quadrant; EQ, External quadrant
Eight external oncoplasties were performed for infiltrating ductal carcinomas clinically classified as CT2N1bMo (Figure 2).
Figure 2. Lateral oncoplasty. A, Mass and preoperative design, 1: mark of the axillary incision, 2: mass, 3: drawing showing the future position of the nipple, B, Wound after lumpectomy and oncoplasty, C, Appearance at the end of the operation. D, Appearance 5 months after the operation, E, operative sample, 1: oriented lumpectomy patch, 2: axillary dissection product.

The upper pedicle technique was performed in 18 cases of mammary carcinoma of the lower quadrants (Table 2, Figure 3).
Figure 3. Superior Pedicle Oncoplasty for Lower Quadrant Carcinoma. A, Preoperative drawing of the patient in supine position. B, Breast appearance at 3rd day post-operative; C, Appearance of the breast one month postoperatively; D, Appearance of the breast one year after radiotherapy.

The Thorek amputation graft technique was performed in 13 cases of lower quadrant carcinoma with macromastia and major ptosis. Table 2 summarizes the different techniques used.
Patients with invasive carcinoma underwent BERG type II axillary dissection in 53/54 cases. In one case of invasive carcinoma (cT1micN0M0), the sentinel node technique was used and the nodes were histologically negative. The sentinel node technique was also performed in 3 cases of carcinoma in situ larger than 5 cm in size. Sentinel nodes were histologically negative. Neoadjuvant chemotherapy was performed in 7 cases of invasive breast carcinoma classified as T3 in patients seeking conservative surgery. It allowed tumor reduction and authorized conservation. Adjuvant chemotherapy was performed in 36 cases. All the patients received radiotherapy except two mammary papillomas. It was organized within two to four months after surgery in patients who did not have adjuvant chemotherapy (26 cases). In patients who had chemotherapy, radiotherapy was organized within three months of adjuvant chemotherapy (36 cases).
Aesthetic sequelae to grade I and II conservative treatment were noted in 2 and 3 cases, respectively. They were treated with lipofilling one year after radiotherapy.
The patients were satisfied with the volume of the remaining breasts and their aesthetic appearance. Evaluated according to the modified Breast Q questionnaire, our patients had satisfaction with physical well-being in 87.3%, psychosocial well-being in 100%. They were 98.4% satisfied with their breasts. Appreciation of sexual well-being was limited by reluctance to provide answers. Fifty-two (52/64) answered the question about sexual well-being and 90.2% were satisfied The mean duration of follow-up was 50.4 months with extremes ranging from 2 months to 99 months. The mortality rate was 10.9% and the lost represented 6.7% of the patients. Overall survival was 98.4% at one year, 96.8% at 2 years, 95.2% at 3 years and 90.5% at 5 years.
Discussion
Breast cancer is the most common female cancer [11]. In the West, conservative surgery and breast reconstruction have gained momentum and 74% of women in France benefit from them without the oncological prognosis being degraded [12]. In India, between 38.8 and 46.6% of patients benefit from this innovative surgery [13]. Although this is still timid in Burkina Faso, requests for conservative surgery are increasingly made by patients. This is why conservative surgery is gradually taking its place [7]. The patients eligible for conservative surgery were only those requesting, carrying a single mass, less than 3 cm, distant from the areola-nipple plaque when radiotherapy was available [14]. Currently, size of tumor is no longer the main eligible criteria for conservation [7, 14]. The conservative surgery with or without an oncoplastic technique is possible as soon as the ratio of tumor size to breast size is less than 20% [7, 14]. The only formal contraindications to conservative surgery are inflammatory tumors regardless of their response to neoadjuvant chemotherapy and also the patient’s refusal [7]. In our setting, the absence of radiotherapy between 2013 and 2020 reduced the potential number of oncoplastic breasts surgeries. This is why only 6.9% of women operated on for breast cancer have benefited from it. In fact, few women could afford radiotherapy outside the country after surgery. We used 6 oncoplastic techniques. The techniques most used in our series were the upper pedicle technique and the Round block technique respectively. The techniques used depend on the topography of the tumor [14]. Oncoplasty can be performed immediately or after neoadjuvant chemotherapy when the size of the mass is large [14, 15]. In all cases of invasive carcinoma, we have associated an axillary dissection removing the first two stages of Berg. This is consistent with the surgical management of invasive breast cancer [16].
Complications were rare in our series and mainly consisted of aesthetic sequelae associated with grade 1 and 2 conservative treatment (ASCT) treated with lipoffiling. In the literature, many sequelae have been described and their treatment is done through lipoffilling, autologous or heterologous flaps [14, 17]. Recurrences were noted in 4.7% of cases. This recurrence rate in our group of patients who all had radiotherapy after surgery was not greater than the rate observed after radical surgery [18]. The 5-year survival was 90.5% in our series. It is better than that of the general population of patients followed for breast cancer [15]. This should be viewed with caution as these better results are largely due to the small size of the tumors in this series rather than to the oncoplastic technique used [9].
In addition to the better oncological results noted, oncoplasty provides aesthetic satisfaction and psychological well-being to the patient [19-21]. In our series, all patients remained satisfied with their breasts even after radiation therapy. In Africa, although satisfaction is objectively seeing it can be overestimated [7]. The patients religiously refrain from criticizing their doctor. Rather, they prefer to thank him for the little obtained [7].
In conclusion, oncoplastic breast surgery is possible in Ouagadougou. The techniques are diversified. The results are good both oncological and aesthetical. It provides physical and psychosocial satisfaction which should be better appreciated by a larger study. With the growing number of specialists, the efforts of associations fighting against cancer which educate women to consult early, and especially the recent advent of radiotherapy, conservative surgery and oncoplasty have a bright future in Burkina Faso.
Acknowledgements
Many thanks to Doctor Diane NDZANA for translating this article in English.
Competing Interests
No funding was received to assist with the preparation of this manuscript.
The authors have no relevant financial or non-financial interests to disclose
Ethics approval and consent to participate
The study was authorized by hospital management and department heads. The data collection was done anonymously and confidentiality was respected for all the patients.
Consent for publication
The pictures of breast cancers attached (Figs. 1, 2, and 3) were used with the agreement of the patient or their family for those who are deceased.
References
- Centre International de Recherche sur le Cancer. Dernières données mondiales sur les cancers : Globocan 2020. OMS. 2020 [cité 12 janv. 2021] Disponible sur : https://gco.iarc.fr/today/data/factsheets/populations/900-world-fact-sheets.pdf..
- Incidences and evolution of cancer frequency in Burkina Faso from 1988 to 2018. Burkina médical Zongo N, Ouédraogo AS , Ouédraogo S, Sanon-Lompo S, Ido FA . .
- Épidémiologie descriptive des cancers en Côte d’Ivoire Effi AB , Koffi KE , Aman NA , Doukouré B, N’dah KJ , Koffi KD , Kouyaté M, Koui BBS , Hondé M, Diomandé MIJM . Bulletin du Cancer.2013;100(2). CrossRef
- Profile of black woman in Senegal with breast cancer Gueye M., Kane Gueye S. M., Ndiaye Gueye M. D., Gueye L., Moreau J.-C.. Medecine Et Sante Tropicales.2016;26(2). CrossRef
- Place de la chirurgie dans la prise en charge des cancers du sein chez la femme au Centre Hospitalier Universitaire Yalgado Ouedraogo: à propos de 81 cas Zongo N, Millogo-Traore TFD , Bagre SC , Bagué A, Ouangre E, Zida M, Bambara A, Bambara TA , Traoré SS . The Pan African Medical Journal.2015;22. CrossRef
- I. The Results of Radical Operations for the Cure of Carcinoma of the Breast Halsted W. S.. Annals of Surgery.1907;46(1). CrossRef
- Oncoplastie selon la technique de Thorek pour cancers des quadrants inférieurs en situation de gigantomastie Zongo N., Yaméogo S. L. C., Zamané H., Tiemtoré S., Zida M., Sanou A., Ouédraogo C., Lompo O. M.. Gynécologie Obstétrique Fertilité & Sénologie.2019;47(9). CrossRef
- Oncoplastic partial breast reconstruction: concepts and techniques Chu CK , Hanson SE , Hwang RF , Wu LC . Gland Surgery.2021;10(1). CrossRef
- Breast surgery for young women with early-stage breast cancer Sun Z, Chen C, Kuang X, Song J, Sun S, Wang W. Medicine.2021;100(18). CrossRef
- Should oncoplastic breast conserving surgery be used for the treatment of early stage breast cancer? Using the GRADE approach for development of clinical recommendations Rocco N, Catanuto G, Cinquini M, Audretsch W, Benson J, Criscitiello C, Di Micco R, Kovacs T, Kuerer H, Lozza L, Montagna G, Moschetti I, Nafissi N, O'Connell RL , Oliveri S, Pau L, Scaperrotta G, Thoma A, Winters Z, Nava MB . Breast (Edinburgh, Scotland).2021;57. CrossRef
- Chirurgie du cancer du sein : traitement conservateur, oncoplastie et reconstruction [Internet]. Issy-les-Moulineaux [France: Elsevier Massons; 2011 [cité 11 mars 2021]. Disponible sur : http://site.ebrary.com/id/10537305 Fitoussi A, Martinet C. .
- Variation in rates of breast cancer surgery: A national analysis based on French Hospital Episode Statistics Rococo E., Mazouni C., Or Z., Mobillion V., Koon Sun Pat M., Bonastre J.. European Journal of Surgical Oncology: The Journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology.2016;42(1). CrossRef
- Rate of Breast-Conserving Surgery vs Mastectomy in Breast Cancer: a Tertiary Care Centre Experience from South India Hassan Ali Shaziya, S P Somashekhar, N Arun Kumar. Indian Journal of Surgical Oncology.2019;10(1). CrossRef
- Oncoplastie avec conservation mammaire dans le traitement du cancer du sein. EMC - Tech chir - Gynécol. 2008;3(1):1–24 Fitoussi A, Alran S, Couturaud B, Charitansky H, Pollet G, Fourchotte V, et al . .
- Oncological Safety of Oncoplastic Level II Mammoplasties After Neoadjuvant Chemotherapy for Large Breast Cancers: A Matched-Cohort Analysis Parra RFD , Clough KB , Thygesen HH , Levy E, Poulet B, Sarfati I, Nos C. Annals of Surgical Oncology.2021;28(11). CrossRef
- The significance of axillary node levels in the study of breast carcinoma Berg J. W.. Cancer.1955;8(4). CrossRef
- [Lipofilling and breast cancer: Literature review in 2015?] Ho Quoc C., Carrabin N., Meruta A., Piat J.-M., Delay E., Faure C.. Journal De Gynecologie, Obstetrique Et Biologie De La Reproduction.2015;44(9). CrossRef
- Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer Fisher B, Anderson S, Bryant J, Margolese RG , Deutsch M, Fisher ER , Jeong J, Wolmark N. The New England Journal of Medicine.2002;347(16). CrossRef
- Oncoplastic breast surgery: Achieving oncological and aesthetic outcomes Paridon MW , Kamali P, Paul MA , Wu W, Ibrahim AMS , Kansal KJ , Houlihan MJ , Morris DJ , Lee BT , Lin SJ , Sharma R. Journal of Surgical Oncology.2017;116(2). CrossRef
- Oncoplastic breast-conserving surgery: More relevant than ever? Results of a survey among breast surgeons Heil J, Riedel F, Solbach C, Gerber B, Marx M, Brucker S, Heitmann C, Hoffmann J, Wallwiener M, Lux MP , Wallwiener D, Hahn M. Archives of Gynecology and Obstetrics.2019;299(4). CrossRef
- Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q Pusic AL , Klassen AF , Scott AM , Klok JA , Cordeiro PG , Cano SJ . Plastic and Reconstructive Surgery.2009;124(2). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times