Squamous Cell Carcinoma of the Breast, a Rare Entity: Report of Case from Ouagadougou/Burkina Faso and Review of the Literature
Download
Abstract
Introduction: Squamous cell carcinoma (SCC) of the breast is a rare tumour. Histology and immunohistochemistry are the key to diagnosis. Treatment is similar to other breast cancers. Its prognosis is poor. We report our first documented case with the aim of describing our diagnostic and therapeutic features.
Case report: A 33-year-old married woman was presented with an ulcerated and oozing mass of the right breast that had been evolving for one year. The examination noted an 8 cm irregular mass attached to the skin which it ulcerated. It was necrotic and foul smelling. Pathological anatomy noted a carcinomatous proliferation centred by keratogenic maturation. Immunohistochemistry was positive for AE1 and AE3 antibodies. The tumour was classified as cT4bN1bM0. It was triple negative. We performed a mastectomy and an axillary curage. Three out of 16 nodes were invaded. She is currently undergoing well-tolerated chemotherapy.
Conclusion: Squamous cell carcinoma of the breast is a rare histological entity. The diagnosis is late like other breast cancers in Ouagadougou. Its prognosis remains poor. This is why early diagnosis, a better knowledge of its histogenesis and profile are important in order to better codify its management.
Introduction
Breast cancer is the most common cancer in the world [1]. It is a nonspecific invasive carcinoma (NSCLC) in over 85% of cases [1]. Primary squamous cell carcinoma (PSC) of the breast is a rare or even exceptional breast cancer [2]. It is known to occur more frequently in the skin and other organs lined with squamous epithelium such as the oesophagus and anal canal [2]. In the breast, PEC is estimated to account for 0.1% to 2% of all invasive carcinomas [3]. Its diagnosis is based on the same principles as other breast carcinomas, i.e. the concordant malignant tripod (clinical + echomammography and pathological anatomy) [3]. Immunohistochemistry plays a central role and shows positivity to anti-cytokeratin antibodies (AE1/AE3) [4]. The indication and type of adjuvant treatment remain poorly defined due to the rarity of the tumour. Its treatment is similar to the therapies used in common histological types of breast cancer [4,5]. These include chemotherapy, surgery, radiotherapy +/- targeted therapies [4,5]. Surgical treatment has the same indications and techniques as for non-specific infiltrating carcinoma (NSCLC) [6]. It is a very aggressive cancer, most often triple negative [7]. Its prognosis is comparable to that of undifferentiated carcinomas [8]. In Burkina Faso, PEC of the breast is exceptional and has never been reported in the literature. We describe our first documented case to describe the particularities of our diagnostic and therapeutic approach.
Observation
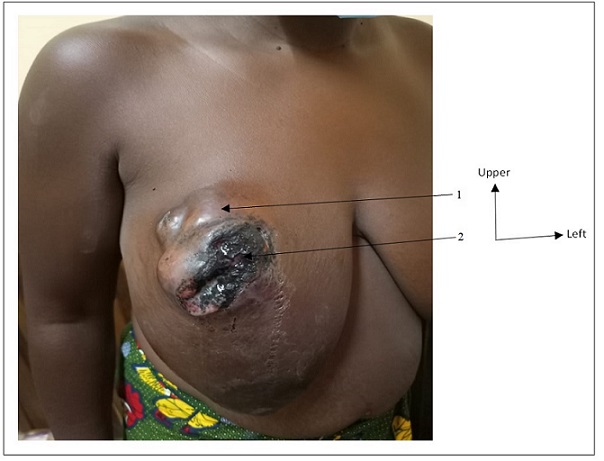
The patient was 33 years old, married, two gestures, two pares. She was admitted in July 2021 for an ulcerated and oozing mass of the right breast evolving for one year. The mass was reported to be initially nodular and then ulcerated. The oozing was profuse, wetting the patient’s clothes. She received traditional treatments such as applying black powder to the wound. She had no personal or family history of breast or gynaecological cancer. There was no evidence of a primary tumour in other organs. Her World Health Organization performance status was rated WHO 1. Breast examination noted an ulcerated, oozing mass with blackish deposits (traditional powder?) in the upper external quadrant (EQ) of the right breast. It measured 8 cm in long axis (Figure 1).
Figure 1. Anterior View Showing the Right Breast Tumour; 1. 8 cm long mass occupying the right superolateral quadrant; 2. Ulceration, oozing, black powder applied to the ulceration.
This mass was mobile in relation to the deep plane and attached to the skin. Pressure on the mass gave rise to a purulent, foul-smelling fluid. We noted mobile, right homolateral, centimetric axillary adenopathies. The histology of the biopsy specimen showed carcinomatous proliferation of massive or lobular architecture.
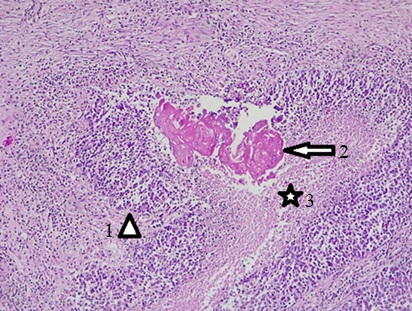
The cells were squamous cells with marked cytonuclear atypia, poor cohesion and abundant basophilic cytoplasm. The nuclei were irregularly outlined, hyperchromatic, with large nucleoli and marked anisokaryosis. Mitotic activity was low. The stroma was fibrous, chronically inflammatory, with no visible vascular emboli or perinuclear sheathing. It was a carcinomatous proliferation centred by keratotic maturation. A moderately differentiated, keratinising, infiltrating squamous cell carcinoma of the right breast was suggested (Figure 2).
Figure 2. Histological Section Showing Squamous Cell Carcinoma of the Breast. (H E stain, G40). 1, Carcinomatous proliferation. 2, Carcinomatous proliferation: centred by keratotic maturation. 3, Carcinomatous proliferation: centred by keratotic maturation: Presence of a focus of comedonecrosis.
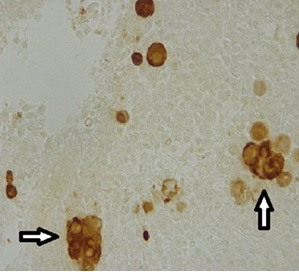
Immunohistochemistry showed labelling of the squamous metaplastic foci with the anti AE1/AE3 antibody confirming the diagnosis of squamous cell carcinoma (Figure 3).
Figure 3. Immunohistochemical Appearance of Squamous Cell Carcinoma of the Breast (Immunohistochemistry, G40). Labelling of squamous metaplastic foci with anti AE1/AE3 antibody.
The tumour was triple negative (RO-, RP-; HER2-).
Thoracic-abdominal-pelvic CT scan did not show any secondary location. The biological work-up showed normochromic and normocytic anaemia at 9.8g/dl, controlled by iron supplementation. In total, it was a primary squamous cell carcinoma of the right breast, triple-negative, classified as CT4bN1bM0, necrotic and leaking a foul-smelling liquid in an anemic patient. A mastectomy plus right axillary curage was performed. Histology of the surgical specimen confirmed the preoperative diagnosis of mature, differentiated squamous cell carcinoma. There was no nipple invasion, no vascular emboli, and no perineural sheathing. The surgical section margins were healthy. Three (3) out of 16 nodes were involved. Neoadjuvant chemotherapy was decided in a multidisciplinary consultation meeting based on the sequential protocol comprising four AC (Adriamycin, Cyclophosphamide) and 4 weekly paclitaxel. She will then receive external radiotherapy. The chemotherapy is well tolerated and she is awaiting her radiotherapy.
Discussion
A rare and poorly understood entity, PECs of the breast represent between 0.1% and 2% of all breast carcinomas [3]. Their ethiopathogeny remains controversial. Is it a separate entity? Or is it a breast adenocarcinoma that has undergone partial or total squamous metaplasia? [2]. According to the WHO, it belongs to the infiltrating ductal carcinomas with total or partial remodelling [2]. The term pure squamous cell carcinoma is used when there is total metaplasia [3]. A glandular or myoepithelial origin has been suggested by some authors [2, 3]. The age of onset of squamous cell carcinoma of the breast is similar to other breast carcinomas. It affects women between 31 and 83 years of age with a peak at 55 years of age [3]. Our patient was 33 years old. No predisposing factor has been established to date, but the notion of local trauma in the patient’s history has been noted in the literature [4]. The clinical and radiological aspects of these tumours are not specific. It can manifest itself as a mass ranging in size from 2 to 6 cm or more [4] as in our case. Sometimes, it can be abscessed or encysted with ulcerations of the skin and pose the problem of its primary or secondary origin [5]. The tumour may be uni or bilateral [3]. Radiologically, ultrasound may show a cystic mass [5]. Ultramammography, which was not performed in our case because of ulcerations and foul-smelling oozing, is not specific for other breast carcinomas [5]. Histology shows the same architecture and cytonuclear features found in squamous cell carcinomas of other organs [4]. Immunohistochemistry shows epithelial tumour cell expression of high molecular weight cytokeratins (CK14, CK5/6 and CK17) as in cases described in the literature [5]. Hormone receptor testing is often negative [6]. Our patient was triple negative. The diagnosis of this type of breast cancer is only made after eliminating a cutaneous origin, glandular breast cancer and breast metastasis of a distant squamous cell carcinoma [4]. In our case, the patient had no other primary site or histological type of breast carcinoma in the affected breast. Treatment is based on mastectomy with axillary lymph node dissection for large tumours, combined with radiotherapy and chemotherapy [8]. Conservative treatment is possible for small tumours [8]. Squamous cell carcinoma is not very lymphophilic and in 70% of cases, curage is free of lymph node metastasis [9]. However, curage of the homolateral axilla is systematic [8]. In our patient, 16 lymph nodes were found and 3 were invaded by squamous cell carcinoma. Neoadjuvant and/or adjuvant chemotherapy uses several protocols. These include CMF (Cyclophosphamide, Methotrexate, 5Fluoro-Uracile) [7], FAC (5-Fluoracil, Adriamycin, Cyclophosphamide) [2] and CF (cis- platinum, 5-Fluoracil) [10]. Our patient received a sequential protocol of antracyclines and taxanes. Age, tumour size, surgery, lymph node status, marital status and initial tumour location were found to significantly influence the mean survival of patients (P<0.001) [8]. Our patient, 5 months after her diagnosis, is at the end of a well tolerated chemotherapy.
In conclusion, primary squamous cell carcinoma of the breast is a rare entity. The diagnostic approach is similar to that of other histological types, but immunohistochemistry is particularly important. The presence of keratotic maturation is a key histological finding. It is a diagnosis of elimination. Therefore, it is always necessary to ensure that it is not a secondary invasion of the skin of the breast by a breast carcinoma, nor a secondary skin localisation of a squamous cell carcinoma located on another part of the body. The prognosis remains poor. This is why early diagnosis and a better understanding of its histogenesis and profile are so important in order to better codify its management.
References
- Organisation Mondiale de la Santé. Le cancer du sein. 2021 [cité le 19 juin 2022] Disponible sur : https://www.who.int/fr/news-room/fact-sheets/detail/breast-cancer#..
- Carcinome épidermoïde du sein: à propos d’un cas en Mauritanie Ahmed Z, Idriss AM , Heiba A, Sidi I. The Pan African Medical Journal.2019;33(143). CrossRef
- Occult squamous cell carcinoma of the axillary tail of breast presenting as isolated axillary lymph node mass Agarwal G, Mishra SK , Dutta NR , Jain M. The European Journal of Surgery = Acta Chirurgica.2000;166(2). CrossRef
- Carcinome épidermoïde du sein: à propos d’un cas et revue de la literature Ziyadi M, Boujoual M, Raiteb Ha, Babahabib MA , Kouach J, Moussaoui DR , Dehayni M. The Pan African Medical Journal.2016;24. CrossRef
- Carcinome épidermoide primitif du sein mimant un abcès Chahdi Hafsa, Abdellah B. Pan African Medical Journal.2018;30. CrossRef
- Carcinome épidermoïde du sein : revue de la littérature : illustrée par le rapport d'un cas Belaabidia B, Sellami S, Hamdaoui A, Ait Ben Kadour Y, Abbassi H. J GynecolObstetBiolReprod (Paris).2002;31(1):34-39 . PMID : 11976575.
- Carcinome épidermoïde primitif du sein. À propos de 3 cas Tayeb K, Saâdi I, Kharmash M, Hadadi K, El Omari-Alaoui H, El Ghazi E, Mansouri A, Errihani H, Benjaafar N, El Gueddari BK . Cancer/Radiothérapie.2002;6(6). CrossRef
- Prognostic factors for breast cancer squamous cell carcinoma and nomogram development for prediction: population-based research Cheng Z, Han T, Zhang X, Li X, Li H, Gu J. Translational Cancer Research.2019;8(5). CrossRef
- Pathologie et génétique des tumeurs du sein et des organes génitaux féminins Tavassol FA , Devilee P. Classification OMS des tumeurs, éditeursLyon :presse .2003;:13-59.
- Primary squamous cell carcinoma of the breast: Sensitivity to cisplatinum-based chemotherapy Dejager D, Redlich PN , Dayer AM , Davis HL , Komorowski RA . Journal of Surgical Oncology.1995;59(3). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2022
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times