The Impact of the COVID-19 Pandemic on the Management of Patients with Oral Potentially Malignant Disorders in a Tertiary Care Hospital, Sri Lanka
Download
Abstract
Introduction: Oral potentially malignant disorders (OPMD) have a higher risk to develop into oral cancer, which is the comments cancer in males in Sri Lanka. The covid-19 pandemic had significant ill effects on the health care systems, worldwide.
Objective: To retrospectively investigate the management of OPMD patients presented to the oral medicine clinic of the University Dental Teaching Hospital Peradeniya, Sri Lanka before and during the pandemic.
Methods: This was a hospital-based cross-sectional study using medical records. The pre-pandemic group included patients diagnosed with OPMD presenting between Jan 2018 - Dec 2019; the pandemic group from Jan 2020 to Dec 2021.
Results: There were 321 eligible medical records. Of these, 247 belong to the pre-pandemic group and 74 in the pandemic (3:1). In the pre-pandemic group, 32% of biopsies were performed within the first week, while it was 56% in the pandemic group. We found a significant increase in the loss of follow-up in the pandemic group compared to the pre-pandemic group (p=0.01). The average delay for the 2nd visit was 27 days, for the 3rd visit it was 127 days in the pre-pandemic; and 89 and 152 days respectively in the pandemic group.
Conclusions: We recommend following evidence-based practices for the management of OPMD in anticipated pandemics. Strategies to diagnose patients at home must be developed and implemented. There is a higher need for the prevention of habit-related risk factors. Biopsy at the first visit or first week is recommended. Patients should be monitored using digital technologies in the absence of physical follow-up.
Introduction
Head and neck cancer has a significant contribution to the global cancer burden, where oral and pharyngeal cancers are among the 10 most common cancers in men globally, with higher incidence reported in low and middle-income countries in Asia [1]. Oral cancer is preventable cancer, mainly due to habit-related risk factors and the presence of clinically distinguishable precursor lesions [2]. In Asia, oral cancer reported a 73.3% of mortality rate, demonstrating an increasing trend with time [3]. Sri Lanka report one of the highest Age Standardized Mortality Rates (ASR) for oral cancer in the world, according to the National Cancer Control Program data published for the year 2019, lip and oral cancers reported the highest incidence rates (n=2173, crude rate=20.6 per 10 000) in Sri Lanka [4]. Since 2016, oral cancers demonstrate a decreasing trend in the country; however, remains the commonest cancer in the male population, accounting for nearly 15% of all cancer incidence [5]. The buccal mucosa is the most familiar anatomical location of oral cancers followed by the tongue [6]. The main risk factors for oral cancers and their precursors are smoking, alcohol consumption, and betel quid chewing [7,8]. Most oral cancers are preceded by precursor conditions collectively identified as “oral potentially malignant disorders” (OPMD). This risk of malignancy in an OPMD can be present in a lesion during the initial diagnosis or can develop later [9]. Therefore, it is of paramount importance that patients diagnosed with OPMD are investigated with biopsy and followed up with adequate time intervals to prevent and or early detect malignant transformation.
The pandemic caused by SARS CoV 2 infection posed significant health and economic burden to countries worldwide [10]. The virus was first isolated and identified in Wuhan, China. The first case of the virus in Sri Lanka was confirmed on 27th January 2020 [11]. Coronaviruses have caused two large-scale pandemics in the last two decades, namely Severe Acute Respiratory Syndrome coronavirus (SARS-CoV) emerged in 2002, and Middle East Respiratory Syndrome coronavirus (MERS-CoV) in 2011. When looking at the disease patterns, similar viral pandemics can be anticipated in the future as well. Therefore, it is important to retrospectively analyze the effect of the pandemic on the health care systems to be equipped with the lessons of the past.
The pandemic situation imposed significant challenges on healthcare workers. Since the virus was transmitted via respiratory droplets, dentists were identified as a high-risk group for cross infections [12]. In most healthcare settings, routine caring setup was interrupted and the attention to the management of other important disease conditions such as cancer was reduced during the pandemic [13]. The pandemic situation caused an island-wide lockdown in several instances from 20th March 2020 in Sri Lanka. Different levels of local lockdowns and travel restrictions were imposed during the pandemic [14]. Further, the general public was advised to refrain from non-essential travel during this period.
Restrictions imposed by the government and other professional bodies as well as personal concerns and fears were reasons for the absence or delay in the treatment- seeking behaviors in patients with oral cancer or OPMD [15]. In the UK, diagnosis and treatment delays in cancer patients during the lockdown were predicted to increase their death rate [16]. The changing lifestyle practices may impact the habit-related risk factors such as smoking, alcohol, and betel quid chewing, which can later manifest as changes in disease patterns.
The Dental Teaching Hospital Peradeniya is the only specialized tertiary care center in Sri Lanka dedicated to delivering treatment for patients diagnosed with OPMD. The Oral Medicine clinic of Dental Teaching Hospital Peradeniya is a unit that caters to patients with oral cancer and potentially malignant disordered patients from all over the country reported annually [17]. This study aimed to retrospectively investigate the attendance, and reasons for delays in OPMD patients presented to the oral medicine department of the Dental Teaching Hospital Peradeniya, before and during the COVID-19 pandemic.
Materials and Methods
Methodology
This study obtained ethical approval from the Ethics Review Committee, Faculty of Dental Sciences, University of Peradeniya. This was a hospital-based cross-sectional study with descriptive analysis. Hospital-maintained medical records were obtained from the repositories of the oral medicine clinic of the University Dental Teaching Hospital, Peradeniya. These were divided into two groups, the pre-pandemic and pandemic groups. The pre-pandemic group included all patients clinically diagnosed with OPMD presenting to the clinic from January 2018 to December 2019. The pandemic group included all patients clinically diagnosed with OPMDpresenting to the clinic from January 2020 to December 2021. We included all data available in the medical records by 02.06.2022. We excluded children below the age of 12 years and incomplete records. Data were extracted and entered using a bespoke Microsoft Excel spreadsheet. Data analysis was performed using JASP (version 0.16.2) and Graph Pad Prism (version 6) software.
Results
Cohort characteristics
A total of 321 medical records were eligible for this study. From these, 247 were in the pre-pandemic group and 74 in the pandemic. The ratio between the number of patients in the pre-pandemic and pandemic groups was 3:1. The mean age of patients in the pre-pandemic group was 48.5 (range 14-83) and the pandemic group was 45.5 (range 15-75). The male-to-female ratio of the pre-pandemic group was 1:1 (117 males and 130 females); in the pandemic group, it was 2:1 (47 males and 27 females). The majority of the patients were from the Kandy district (68% in the pre-pandemic group and 73% in the pandemic group) followed byKegalla, Kurunagala, Matale, and Nuwaraeliya. Table 1 presents data on risk factors and histological diagnosis of patients in the two study groups. Using the Chi-square test, we found a significant difference between the smoking and alcohol habits of patients between the two study groups.
| Variable | Category | Number of patients | P value | |
| Pre-pandemic (%) | Pandemic (%) | |||
| Smoking | No | 224 (90.6) | 61 (82.4) | 0.048* |
| Yes | 23 (9.4) | 13 (17.6) | ||
| Alcohol | No | 225 (91.0) | 53 (71.6) | 0.001* |
| Yes | 22 (9.0) | 21 (28.4) | ||
| Betel quid | No | 159 (64.3) | 39 (52.7) | 0.07 |
| Yes | 88 (35.7) | 35 (47.3) | ||
| Histological diagnosis | KMS | 23 (9.3) | 9 (12.6) | 0.326 |
| KSED | 0 | 1 (1.4) | ||
| LP MED | 1 (0.4) | 0 | ||
| LR | 3 (1.2) | 0 (1.4) | ||
| LR MED | 0 | 1 (1.4) | ||
| OLP | 125 (50.8) | 33 (46.8) | ||
| OLP LR | 28 (11.4) | 7 (9.8) | ||
| OLP LR MED | 1 (0.4) | 0 | ||
| OLP LR SCP | 1 (0.4) | 0 | ||
| OLP MED | 5 (2) | 1 (1.4) | ||
| OSF | 41 (16.6) | 15 (21.1) | ||
| OSF LR | 1 (0.4) | 0 | ||
| OSF MED | 17 (7.1) | 3 (2.7) | ||
| VCA | 0 | 1 (1.4) | ||
| NR | 1 | 3 |
KMED, keratosis with mild epithelial dysplasia; KSED, keratosis with severe epithelial dysplasia; LP MED, lichen planus with mild epithelial dysplasia; LR, lichenoid reaction; LR MED, lichenoid reaction with mild epithelial dysplasia; OLP, oral lichen planus; OLP LR, OLP LR MED, OLP LR SCP, OLP MED, OSF, oral submucous fibrosis; OSF LR, OSF MED, oral submucous fibrosis with mild epithelial dysplasia; VCA, verrucous carcinoma, NR: not reported.
In the pandemic group, the % of smokers was higher than in the pre-pandemic group. Similarly, % of alcohol drinkers in the pandemic group was higher (roughly 3 times) than in the pre-pandemic group. In both study groups, the highest number of OPMD patients were oral lichen planus (OLP), followed by oral submucous fibrosis (OSF).
Biopsy and associated delays
All patients clinically diagnosed with OPMD are offered an incisional biopsy for histopathological confirmation of the clinical diagnosis. We investigated the delays associated with performing biopsies in the study groups. According to data presented in Table 2, there were significant differences in the performance of biopsies in the two study groups.
| Variable | Category | Number of patients | P value | |
| Pre-pandemic (%) | Pandemic (%) | |||
| Biopsy (Bx) done on the planned date | Yes | 234 (94.5) | 63 (85.2) | 0.006* |
| No | 13 (5.2) | 11 (14.8) | ||
| Time-lapse between 1st visit and Bx | Bx on 1st visit | 22 (8.9) | 20 (27) | 0.001* |
| Within 1 week | 58 (23.4) | 22 (29.7) | ||
| Within 2 weeks | 45 (18.2) | 6 (8.1) | ||
| 2-4 weeks | 74 (29.9) | 10 (13.5) | ||
| >4 weeks | 48 (19.6) | 16 (21.7) | ||
| Reasons for Bx delay | Patient factors | 5 (38.5) | 6 (54.5) | 0.341 |
| Clinician factors | 6 (46.1) | 4 (36.3) | ||
| Hospital factors | 2 (15.4) | 0 | ||
| Patients medical reason | 0 | 1 (9.2) |
P values for the Chi-square test, p<0.05 was taken as a statistically significant difference.
Compared to the pre-pandemic group, a significantly high % of biopsies were not performed on the planned date in the pandemic group. On the contrary, only 8.9% of biopsies were performed on the 1 visit in the pre-pandemic group, this has been increased to 27% in the pandemic group. In the pre-pandemic group, only 32% of biopsies were performed within the first week of presentation, while 56% of biopsies were performed within the first week in the pandemic group. In the pandemic group, 54.6% of the delay in biopsies was due to patient-related factors, in the pre-pandemic group the highest percentage of delay was due to clinician-related factors.
Follow-up visits and associated delays
We investigated the follow-up visits and associated delays in the two study groups, these data are graphed in Figure 1.
Figure 1. Attendance of Patients for Follow-up Visits in the Two Study Groups. Values are presented as % of participants from each study group. Yes, patients attended the visit on the given date; No, patients did not attend the visit on the given date; LFU, loss to follow up indicates % patients who did not attend the visit to date.
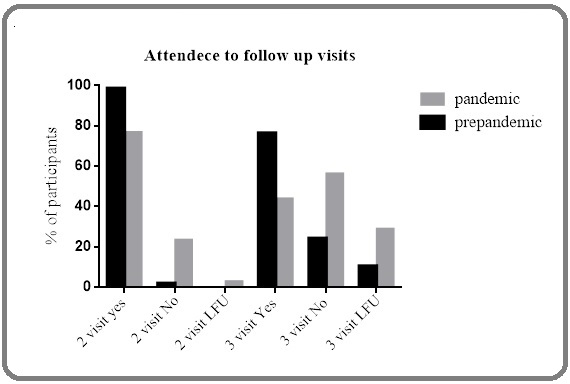
The percentage of participants who attended the first follow-up visit (2 visits) in the pre-pandemic group was 98.38%, while it was 76.71% in the pandemic group. The percentage of non-attendance for the 2 visits was 1.62% in the pre-pandemic group and 23.29% in the pandemic group. For the 2nd follow up visit (3rd visit) 76.11% attended and 23.89% were absent in the pre-pandemic group. In the pandemic, group 43.83% attended the 3rd visit while 56.17% were absent on the appointment date. There was an increase in non-attendance to follow-up visits in the pandemic group, compared to the pre-pandemic group.
All patients in the pre-pandemic group were followed up by a 2nd visit, whereas 2 patients (2.7%) in the pandemic group did not attend a 2nd visit (loss to follow- up). The Chi-square test revealed a significant p-value (0.009) when the study groups were compared. Similarly, 25 (10.12%) patients in the pre-pandemic group and 21 (28.7%) in the pandemic group did not attend a 3rd visit (loss to follow up in the 3rd visit). The Chi-square test revealed a significant p-value (<0.001) when the study groups were compared. We found a significant increase in the loss of follow-up in the pandemic group compared to the pre-pandemic group.
In the pre-pandemic group, 7 patients and 14 patients of the pandemic group presented to the clinic for the 2 visits with delays. For the 3rd visit, 34 patients in the pre-pandemic group and 19 in the pandemic group presented with delays. The number of days of delay is presented in Figure 2.
Figure 2. Number of Delayed Days for 2nd and 3rd Visit Follow-up in Study Groups. Data are presented as scatter plots with all data points and horizontal bars for men and a 95% confidence interval.
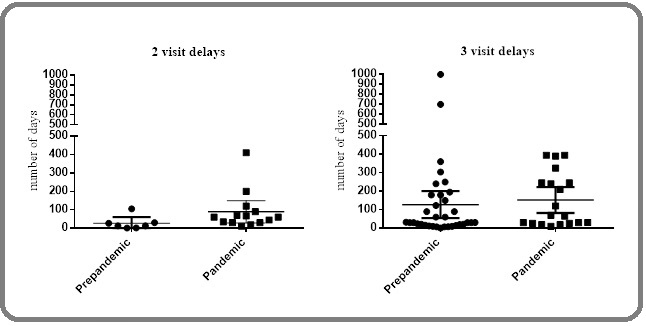
In the pre-pandemic group, the average delay for the 2nd visit was 27 days, for the 3rd visit it was 127 days. In the pandemic group, the average delay for the 2nd visit was 89 days, for the 3rd visit it was 152 days.
Discussion
The covid-19 pandemic is among the substantial challenges faced by mankind in the 21st century. It has caused a significant impact on health care systems, the economy, habits, lifestyle, and human biology around the globe. When analyzing the patterns of pandemics, similar viral pandemics can be anticipated in the future as well. Hence, it is important to retrospectively study the various effects of the pandemic for future policy and practice.
Oral cancer is a significant public health problem in Sri Lanka; it is the commonest cancer in males in this country [18]. Oral cancer is preceded by precursor conditions collectively identified as OPMD. As Sri Lanka is a low and middle-income country, thereby has limited human resources as well as health care facilities. Dental Teaching Hospital Peradeniya is a tertiary care center specialized to deliver treatment for OPMD. In this study, we attempted to compare the presentation and management of OPMD patients before and during the pandemic.
We observed a substantial reduction in the number of OPMD patients during the pandemic. In our study, the number of OPMD patients presented during the pandemic was one-third compared to the pre-pandemic group. In a study done in India, comparisons between the pre-lockdown and post-lockdown data yielded significant changes in the proportions of oral sub-mucous fibrosis, oral leukoplakia, oral lichen planus, and oral cancer presentation [19]. In their study, a reduction was observed in oral submucous fibrosis, and the proportion of oral cancer cases increased. On the contrary, in our study, the proportion of types of OPMDs was similar in the two study groups. Several reports suggested that the COVID-19 pandemic can have a significant impact on the early detection of oral cancer and OPMDs [20, 21]. Our results support this conclusion as the reduction in the number of OPMD cases in the clinic reflected the indirect effects of the pandemic than the actual reduction in the number of patients. As the patients diagnosed at the OPMD stage have reduced, they can present with oral cancers in the post-pandemic era.
An interesting finding of our study was the higher % of smokers and alcohol drinkers in the pandemic group than in the pre-pandemic group. More free time with reduced activity, more time spent at home, and high levels of stress due to social and economic constraints can lead to significant changes in risk habits such as smoking and alcohol. A systematic review on the effect of the pandemic on smoking reported that smokers tend to purchase large quantities of smoking during the pandemic and therefore, this can lead to increased frequency [22]. Much evidence supports the notion that significant lifestyle changes including dietary habits, alcohol consumption, and mental health were caused by the pandemic [23], the associations between these changes and disease patterns must be further explored.
We intended to investigate the effects of the pandemic on aspects of health care delivery. The biopsy is an essential investigation in the management of OPMD. A positive impact of the pandemic was that more biopsies were performed during the first week of the presentation including a higher number on the first visit itself. This can be due that planned appointments for biopsy may be interrupted due to travel restrictions during the pandemic. This can be adopted as a future policy to increase the effective and timely delivery of care to OPMD patients.
We observed a significant increase in the loss to follow-up and an increase in the number of delays in the pandemic group, compared to the pre-pandemic group. This finding highlights the need for employing teledentistry and digital technology for patient follow-up. If the patient is unable to physically attend the follow-up visits, they should be given a chance of a video conference or in their absence, a telephone conversation with the clinician. Despite the limitations of examination and accurate visual inspection, these strategies may be effective in delivering health promotion, motivation, and habit intervention. A similar finding was reported where digital technologies, such as video conferencing with Zoom, Google Meeting, or WhatsApp, were useful tools for patient triage, managing emergencies, reassurance, and follow of OPMD patients [24].
One of the limitations of this study is the absence of contact details such as email or contact telephone numbers in the medical records. Due to this limitation, we could not extract reasons for the delay in the attendance to follow-up visits from patients. A similar study conducted in another Tertiary care center in Sri Lanka (National Cancer Hospital, Maharagama) reported that the education level of the patients and traveling costs were associated with delays in seeking treatment [25]. We recommend improving the medical record keeping including contact details (telephone or email) of the patients or their family members for future reference in the absence of physical follow-up.
In conclusions, Covid-19 had a significant impact on the fields such as health care, economy, and lifestyle.These changes may manifest as disease patterns in the post-pandemic era. Our study revealed important changes in the presentation and management of OPMD patients in the pandemic group compared to the pre-pandemic situation in the Teaching Hospital Peradeniya, in Sri Lanka. To improve the health care delivery to patients with OPMD, we propose the following evidence-based recommendations for practice and policy in anticipated viral pandemics. During a pandemic the presentation of OPMD patients to clinics may be reduced; therefore, strategies to diagnose patients at home (screening at home) must be developed, applicable to low resource settings. During a pandemic, there is a tendency to increase habit-related risk factors such as smoking, alcohol, and betel quid chewing. Effective prevention programs must be iterated during this time. Biopsy at the first visit or within the same week is recommended for patients presenting to the clinic during a pandemic. Further, patients should be followed up using video conference, and or telephone conversations in the absence of physical presence during follow-up visits.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for- profit sectors.
Acknowledgments
Statement of Transparency and Principals:
· Author declares no conflict of interest
· Study was approved by Research Ethic Committee of author affiliated Institute.
· Study’s data is available upon a reasonable request.
· All authors have contributed to implementation of this research.
References
- Epidemiology and Demographics of the Head and Neck Cancer Population Cohen N, Fedewa S, Chen AY . Oral and Maxillofacial Surgery Clinics of North America.2018;30(4). CrossRef
- Oral Cancer and Precancer: A Narrative Review on the Relevance of Early Diagnosis Abati S, Bramati C, Bondi S, Lissoni A, Trimarchi M. International Journal of Environmental Research and Public Health.2020;17(24). CrossRef
- Epidemiologic aspects of oral cancer Sarode G, Maniyar N, Sarode SC , Jafer M, Patil S, Awan KH . Disease-a-month: DM.2020;66(12). CrossRef
- Cancer Incidence Data Book-2019.pdf Registry NC. 2019.
- Cancer services in Sri Lanka: current status and future directions Jayarajah U, Abeygunasekera AM . Journal of the Egyptian National Cancer Institute.2021;33(1). CrossRef
- Descriptive study of 896 Oral squamous cell carcinomas from the only University based Oral Pathology Diagnostic Service in Sri Lanka Jayasooriya PR , Pitakotuwage TN , Mendis BRRN , Lombardi T. BMC Oral Health.2016;16(1). CrossRef
- Oral potentially malignant disorders: risk of progression to malignancy Speight PM , Khurram SA , Kujan O. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology.2018;125(6). CrossRef
- Prevalence and Risk Factors for Oral Potentially Malignant Disorders in Indian Population Singh AK , Chauhan R, Anand K, Singh M, Das SR , Sinha AK . Journal of Pharmacy & Bioallied Sciences.2021;13(Suppl 1). CrossRef
- Oral potentially malignant disorders Amagasa T. Oral Cancer.;:83-98. CrossRef
- ‘Corona Virus: A Review of COVID-19’ Kumar D. Eurasian Journal of Medicine and Oncology, (April).2020. CrossRef
- Effectiveness of the Strategies Implemented in Sri Lanka for Controlling the COVID-19 Outbreak Erandi KKWH , Mahasinghe AC , Perera SSN , Jayasinghe S. Journal of Applied Mathematics.2020;2020. CrossRef
- COVID-19 transmission risk and protective protocols in dentistry: A systematic review Banakar M, Lankarani K, Jafarpour D, Moayedi S, Banakar M, Mohammadsadeghi A. BMC Oral Health.2020;20. CrossRef
- Cancer diagnostic delay in the COVID-19 era: what happens next? Hamilton W. The Lancet. Oncology.2020;21(8). CrossRef
- Social distancing and its impact on flattening the COVID-19 curve in Sri Lanka Hewage S, Wickramasinghe N, Jayakody S, Samaranayake D, Prathapan S, Arambepola C. Journal of the College of Community Physicians of Sri Lanka.2020;26. CrossRef
- Cancer symptom experience and help-seeking behaviour during the COVID-19 pandemic in the UK: a cross-sectional population survey Quinn-Scoggins HD , Cannings-John R, Moriarty Y, Whitelock V, Whitaker KL , Grozeva D, Hughes J, et al . BMJ open.2021;11(9). CrossRef
- Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study Sud A, Torr B, Jones ME , Broggio J, Scott S, Loveday C, Garrett A, et al . The Lancet. Oncology.2020;21(8). CrossRef
- GIS to Explore the Geographical Mysteries of Oral Cancer: Geospatial Distribution of Patients Diagnosed with Oral Potentially Malignant Disorders at the University Dental Hospital Peradeniya Athukorala I, Medawela RMSHB , Gunawardana M, Jayasinghe RD . Asian Pacific Journal of Cancer Care.2022;7(1). CrossRef
- Barriers to early detection and management of oral cancer in the Asia Pacific region Ng SW , Syamim Syed Mohd Sobri SN , Zain RB , Kallarakkal TG , Amtha R, Wiranata Wong FA , Rimal J, et al . Journal of Health Services Research & Policy.2022;27(2). CrossRef
- Impact of COVID-19 Lockdown on Oral Oncology-related Outpatient Volume at Indian Dental Institutions Panta P, Reddy P, Misra SR , Segonds-Pichon A, Patil S. The Journal of Contemporary Dental Practice.2021;22(5).
- Oral potentially malignant disorders: A consensus report from an international seminar on nomenclature and classification, convened by the WHO Collaborating Centre for Oral Cancer Warnakulasuriya S, Kujan O, Aguirre-Urizar JM , Bagan JV , González-Moles MA , Kerr AR , Lodi G, et al . Oral Diseases.2021;27(8). CrossRef
- Could we benefit from oral self-examination during the COVID-19 pandemic? Motta ACF , Rodrigues KRDH . Oral Oncology.2020;107. CrossRef
- Systematic review of changed smoking behaviour, smoking cessation and psychological states of smokers according to cigarette type during the COVID-19 pandemic Chun H, Cheon E, Hwang J. BMJ open.2022;12(6). CrossRef
- Lockdown Due to COVID-19 and Its Consequences on Diet, Physical Activity, Lifestyle, and Other Aspects of Daily Life Worldwide: A Narrative Review Rubio-Tomás T, Skouroliakou M, Ntountaniotis D. International Journal of Environmental Research and Public Health.2022;19(11). CrossRef
- Management of oral medicine emergencies during COVID-19: A study to develop practise guidelines Lv N, Sun M, Polonowita A, Mei L, Guan G. Journal of Dental Sciences.2021;16(1). CrossRef
- Patient-Linked Factors Associated with Delayed Reporting of Oral and Pharyngeal Carcinoma among Patients Attending National Cancer Institute, Maharagama, Sri Lanka Alahapperuma LS , Fernando EA . Asian Pacific journal of cancer prevention: APJCP.2017;18(2). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2023
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times