Treatment Outcome of Early-stage Laryngeal Carcinoma Treated with Radical Radiotherapy Using Different Techniques: A Retrospective Study
Download
Abstract
Aim: The aim was to evaluate the treatment outcomes and prognostic characteristics of patients with early-stage glottic laryngeal carcinoma who underwent radical radiotherapy (RT) with different techniques.
Materials and Methods: Radiotherapy was applied using the 2D conventional technique, 3DCRT (three dimensional conformal radiotherapy and IMRT (intensity modulated radiation therapy). Clinical T stages were 12 (48%) for T1a, 5 (20%) for T1b and 8 (32%) for T2. Stage and anterior commissure involvement were analyzed as prognostic factors.
Results: There were 12 (48%) patients with T1a, 5 (20%) patients with T1b and 8 (32%) patients with T2 cancer. 5 years of overall survival and diseases free survival for T1a, T1b, T2 were found to be 91%, 80%, 62% and 91%, 80%, 62% respectively. 5 year survival for patients without and with involvement of anterior commissure was 92% and 67% respectively. Hence, showing poor survival in patients with T2 lesion or T1 lesion with involvement of anterior commissure.
Conclusion: In early-stage laryngeal carcinomas, radical RT is a function sparing and effective treatment modality with excellent survival rates, regardless of treatment techniques.
Introduction
Early laryngeal cancer, especially of the glottis, is primarily a local disease, and radiotherapy is the main treatment used to preserve the larynx. Early glottic cancer (T1-T2) is a highly treatable disease with excellent survival rates. Available treatment options include CO2 transoral laser microsurgery (CO2 TOLMS), open partial laryngectomy (OPL), or radiotherapy (RT). To date, there is no clear evidence regarding the effectiveness of surgical treatment (CO2 TOLMS and OPL) over RT, including a recent Cochrane analysis [1-6].
Radiation is the primary nonsurgical treatment for early stage glottic tumours (i.e., T1, T2/N0). Although radiotherapy techniques and doses may vary, a standard course of radiation for glottic cancer usually consists of a total of 60-70Gy administered in single daily fractions over 6-7 weeks. Advantages of radiotherapy include the avoidance of surgery and the subsequent hospitalization. A useful voice is preserved in 80-95% of patients who were treated with radiation for an early glottic tumor. Of these patients, 80-90% are reported to have good-to-excellent voice quality. Radiation failures can be salvaged successfully with surgery.
Five years of local control rates are 85–94% for T1 glottic cancers and 70–85% for T2 with radical RT in the literature [7-12]. Since a randomized trial from Japan demonstrated better local control rates with hypo-fractionated RT regimens, the use of such treatment modalities became more common [13]. However, the increase in local control rates provided by different fractionation regimens and new RT techniques has no impact on overall survival rates.
The implementation of new radiotherapy techniques such as carotid-sparing treatments has led to a decrease in non-malignant deaths and is used more often in the treatment of early-stage laryngeal carcinoma patients [14]. In this study, we evaluated the treatment outcomes and the prognostic factors of patients with early-stage glottic laryngeal carcinoma.
Materials and Methods
Patients
In this study, 25 cases with T1-T2/N0 glottic laryngeal carcinoma, who underwent radical RT between January 2017 to December 2021 were evaluated retrospectively. The median age of patients was 60 years, and a clear majority of them were men (96%). The histopathological diagnosis was squamous cell carcinoma.
Diagnosis and Staging
Patients were assessed with detailed head and neck and systemic physical examination, whole blood count, and chest X-ray. The patients were staged with direct laryngoscopy and biopsy under anaesthesia. In patients with anterior commissure involvement, the cartilage involvement was evaluated by computed tomography (CT).
Radiotherapy
Radical RT was applied to patients with stage I glottic carcinoma and stage II disease (inoperable, low performance, comorbid disease, or patient preference). Patients were treated with two-dimensional (2D) conventional technique, 3DCRT (three-dimensional conformal radiotherapy and IMRT (intensity modulated radiation therapy) techniques.
Statistics
Overall survival was calculated from the first day of diagnosis to the any cause of death. The locoregional failure event/time was used to calculate disease-free survival. Disease-free survival (DFS) is defined as the time from radiotherapy start, until disease recurrence or death. Stage and anterior commissure involvement were evaluated as prognostic factors. Survival analysis was done by using SPSS software with the Kaplan–Meier method.
Follow-Up
The treatment response and side effects were assessed at least once a week during RT. Response evaluation was done by flexible and/or direct laryngoscopy and CECT at 2–4 months after treatment. Follow-up was carried out every 2-3 months for the first 2 years after RT, every 6 months between 3 and 5 years.
Early and late side effects (according to RTOG/EORTC criteria) and the response assessment were carried out together with an ENT specialist and a radiation oncology specialist. Direct laryngoscopy and biopsy was performed in case of any pathologic findings. In any case of failure, each patient was evaluated individually and salvage treatments were planned accordingly.
Results
In our study we retrospectively analysed data of 25 patients who were treated for early glottis squamous cell carcinoma (T1N0M0/T2N0M0) with definitive radiation therapy using different techniques between January 2017 to December 2021. Out of 25 patients, 24 were males and 1 was a female. Mean age of the patients was 60 years. In 24 out of 25 patients, smoking was identified as a risk factor, and hoarseness of voice was identified as the most prevalent symptom.
12 (48%) patients had T1a cancer, 5 (20%) had T1b cancer, and 8 (32%) had T2 cancer. Out of the 25 patients, 12 (48%) had anterior commissure involvement (Table 1).
| Variables | Category | n=25 | % |
| Gender | Male | 24 | 96 |
| Female | 1 | 4 | |
| Smoking | Smoker | 24 | 96 |
| Non Smoker | 1 | 4 | |
| Symptom | Hoarseness of voice | 24 | 96 |
| Upper respiratory tract infection | 1 | 4 | |
| HPE | Poorly Differentiated Squamous Cell Carcinoma | 5 | 20 |
| Moderately Differentiated Squamous Cell Carcinoma | 8 | 32 | |
| Well Differentiated Squamous Cell Carcinoma | 12 | 48 | |
| T Stage | T1a | 12 | 48 |
| T1b | 5 | 20 | |
| T2 | 8 | 32 | |
| Anterior Commissure | Yes | 12 | 48 |
| Involved | No | 13 | 52 |
All of these patients received radical radiation over a period of 6 weeks and 3 days with five fractions each week at a dose of 66 Gy in 33 fractions @ 2 Gy per fraction.
These patients had a response assessment utilising CECT and direct laryngoscopy six weeks after the radiation treatment was finished. It was discovered that 21 patients (or 84%) had a full clinico-radiological response, while 4 patients had residual disease and required a partial laryngectomy as a result. Two of the four patients who had residual disorders after finishing radiation treatment had T2 lesions, while the other two had T1 lesions that had anterior commissure involvement.
Out of 25 patients 14 (56%) were treated with the conventional technique, 6 (24%) with 3DCRT and 4 (16%) with IMRT. The overall survival rate was the same regardless of the technique used. The most frequent acute toxicities observed in the majority of individuals were Grade 1 skin toxicity and odynophagia. None of them displayed late toxicity.
The mean and median overall and disease-free survival for patients with well-differentiated glottic squamous cell carcinoma in our study were [24, 20] and [21, 19] months, respectively. This survival was statistically significant (p<0.001) (Table 2).
| Parameter | Categories | Overall Survival (OS) | Disease Free Survival (DFS) | ||||
| Mean | Median | Sd | Mean | Median | Sd | ||
| HPE | P.D.Sq cell ca | 18 | 20 | 7 | 16 | 18 | 7 |
| M.D Sq.cell.ca | 22 | 22 | 10 | 20 | 19 | 10 | |
| W.D.Sq cell ca | 24 | 20 | 11 | 21 | 19 | 10 | |
| T-stage | T1a | 28 | 27 | 9 | 27 | 26 | 9 |
| T1b | 23 | 22 | 12 | 24 | 24 | 13 | |
| T2 | 20 | 20 | 8 | 18 | 18 | 7 | |
| Anterior | Yes | 19 | 20 | 8 | 17 | 18 | 7 |
| Commissure | |||||||
| Involved | No | 24 | 21 | 11 | 22 | 19 | 11 |
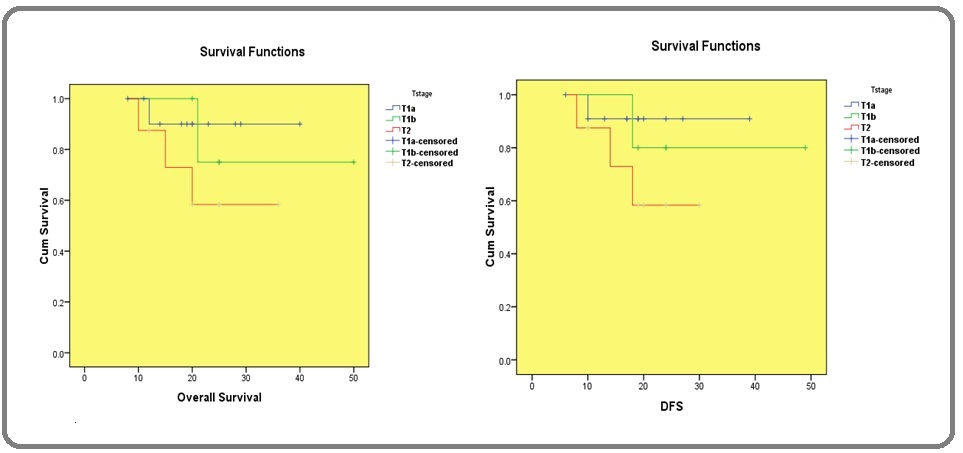
5 year overall survival (OS) and diseases free survival (DFS) for whole group was 80% and 78% (Figure 1) and for T1a, T1b , T2 were found to be 91%, 80%, 62% and 88%, 75%, 59% respectively (Figure 2).
Figure 1. Overall Survival (OS) and Disease Free Survival (DFS).
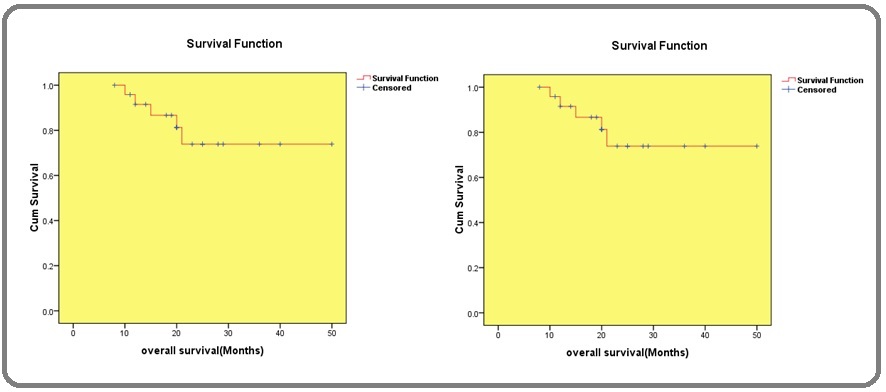
Figure 2. Overall Survival and Disease Free Survival with T Stage.
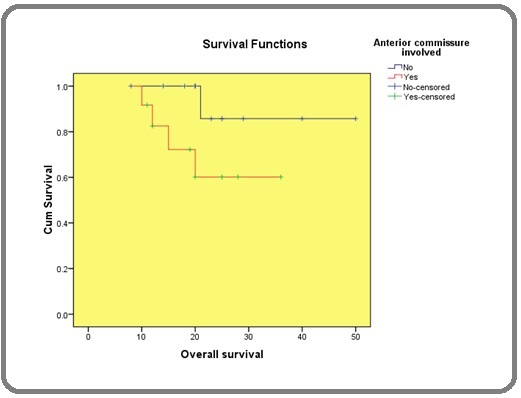
5 year survival for patients with and without involvement of anterior commissure was 67% and 92% respectively. Hence, showing poor survival in patients with involvement of anterior commissure (Figure 3).
Figure 3. Overall Survival with and without Involvement of Anterior Commissure.
Discussion
Early-stage glottic laryngeal carcinomas can be cured by radical RT or local surgical excision. The treatment decision depends on the patient’s preference as well as the technical possibilities and experience of the treatment team or the disease-specific features such as tumor location, single or bilateral vocal cord, and anterior commissure involvement.
In our study, 5 years of overall survival was 80% for the whole group and 91%, 80%, 62%for T1a, T1b and T2. Diseases free survival was 78% for the whole group and 88%, 75%, 59% for T1a, T1b and T2 respectively. These results are similar to those reported in many studies. Thariat et al. evaluated 155 patients with T1 and T2 glottic carcinomas. Overall survival was 75% for the whole group, 85% for T1a, 72% for T1b, 59% for T2. Disease-free survival was 68% for the whole group, 77% for T1a, 51% for T1b, 58% for T2 respectively [15]. Johansen et al. from Denmark has evaluated 861 glottic laryngeal carcinoma cases retrospectively and reported 5 years of disease-specific survival rates for T1a, T1b, and T2 tumors to be 95%, 93%, and 83%, respectively [12]. Chera et al. evaluated retrospectively 585 patients with T1N0, T2N0 glottic larynx carcinoma treated by RT at Florida University. In this study, 5 years of local control rates were reported as 94% for T1a; 93% for T1b; 80% for T2a, and 70% for T2 [10].
In our study, stage and anterior commissure involvement are evaluated as prognostic factors in univariate analyses. Stage (p < 0.001) and anterior commissure involvement (p < 0.001) were found to be significant in overall survival and disease-free survival. Patients with T2NOMO and involvement of anterior commissure were having poor survival and these results were consistent with many other studies which determined that stage and anterior commissure involvement are the prognostic factors in early stage glottic carcinoma [16-21]. In our study, using conventional or conformal radiation techniques had no effect on overall survival and toxicity profile was also same proving none beneficial over the other.
In conclusion, radical radiotherapy remains an efficient option in the treatment of early glottic carcinomas providing a high local control rate with excellent functional results in laryngectomy-free patients, regardless of treatment techniques. This strategy should be discussed according to the tumour stage, feasibility of conservative surgery and patient’s preferences.
Conflict of interest
Nil
Funding
Nil
References
- Treatment of early-stage glottic cancer: meta-analysis comparison of laser excision versus radiotherapy Higgins KM , Shah MD , Ogaick MJ , Enepekides D. Journal of Otolaryngology - Head & Neck Surgery = Le Journal D'oto-Rhino-Laryngologie Et De Chirurgie Cervico-Faciale.2009;38(6).
- Laser surgery versus radiotherapy for T1-T2N0 glottic cancer: a meta-analysis Feng Y, Wang B, Wen S. ORL; journal for oto-rhino-laryngology and its related specialties.2011;73(6). CrossRef
- Transoral Laser Microsurgery in Early Glottic Lesions Sjögren EV . Current Otorhinolaryngology Reports.2017;5(1). CrossRef
- Radiotherapy versus open surgery versus endolaryngeal surgery (with or without laser) for early laryngeal squamous cell cancer Warner L, Chudasama J, Kelly CG , Loughran S, McKenzie K, Wight R, Dey P. The Cochrane Database of Systematic Reviews.2014;2014(12). CrossRef
- Oncologic and functional outcomes of patients treated with transoral CO2 laser microsurgery or radiotherapy for T2 glottic carcinoma: a systematic review of the literature Hendriksma M, Heijnen BJ , Sjögren EV . Current Opinion in Otolaryngology & Head and Neck Surgery.2018;26(2). CrossRef
- Transoral laser microsurgery versus radiotherapy for T2 glottic squamous cell carcinoma: a systematic review of local control outcomes Warner L., Lee K, Homer JJ . Clinical otolaryngology: official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery.2017;42(3). CrossRef
- Voice quality after treatment of early vocal cord cancer: a randomized trial comparing laser surgery with radiation therapy Aaltonen LM , Rautiainen N, Sellman J, Saarilahti K, Mäkitie A, Rihkanen H, Laranne J, et al . International Journal of Radiation Oncology, Biology, Physics.2014;90(2). CrossRef
- Radiotherapy for laryngeal cancer-technical aspects and alternate fractionation Yamazaki H, Suzuki G, Nakamura S, Yoshida K, Konishi K, Teshima T, Ogawa K. Journal of Radiation Research.2017;58(4). CrossRef
- T1-T2N0 squamous cell carcinoma of the glottic larynx treated with radiation therapy Mendenhall WM , Amdur RJ , Morris CG , Hinerman RW . Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2001;19(20). CrossRef
- T1N0 to T2N0 squamous cell carcinoma of the glottic larynx treated with definitive radiotherapy Chera BS , Amdur RJ , Morris CG , Kirwan JM , Mendenhall WM . International Journal of Radiation Oncology, Biology, Physics.2010;78(2). CrossRef
- Radical radiotherapy for early glottic cancer: Results in a series of 1087 patients from two Italian radiation oncology centers. I. The case of T1N0 disease Cellai E, Frata P, Magrini SM , Paiar F, Barca R, Fondelli S, Polli C, et al . International Journal of Radiation Oncology, Biology, Physics.2005;63(5). CrossRef
- Glottic carcinoma--patterns of failure and salvage treatment after curative radiotherapy in 861 consecutive patients Johansen LV , Grau C, Overgaard J. Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2002;63(3). CrossRef
- Radiotherapy for early glottic carcinoma (T1N0M0): results of prospective randomized study of radiation fraction size and overall treatment time Yamazaki H, Nishiyama K, Tanaka E, Koizumi M, Chatani M. International Journal of Radiation Oncology, Biology, Physics.2006;64(1). CrossRef
- Intensity-modulated radiotherapy for early glottic cancer: transition to a new standard of care? Samuels MA , Freedman LM , Elsayyad N. Future Oncology (London, England).2016;12(22). CrossRef
- Conservative treatment of early glottic carcinomas with exclusive radiotherapy Thariat J, Bruchon Y, Bonnetain F, Barillot I, Truc G, Peignaux K, Horiot JC, Maingon P. Cancer Radiotherapie: Journal De La Societe Francaise De Radiotherapie Oncologique.2004;8(5). CrossRef
- Patterns of Care for Patients With Early-Stage Glottic Cancer Undergoing Definitive Radiation Therapy: A National Cancer Database Analysis Stokes WA , Abbott D, Phan A, Raben D, Lanning RM , Karam SD . International Journal of Radiation Oncology, Biology, Physics.2017;98(5). CrossRef
- Radiation therapy in early glottic carcinoma: uni- and multivariate analysis of prognostic factors affecting local control Sakata K, Aoki Y, Karasawa K, Hasezawa K, Muta N, Nakagawa K, Terahara A, Onogi Y, Sasaki Y, Akanuma A. International Journal of Radiation Oncology, Biology, Physics.1994;30(5). CrossRef
- Prognostic factors in early glottic carcinoma implications for treatment Nur DA , Oguz C, Kemal ET , Ferhat E, Sülen S, Emel A, Münir K, Ann CSR , Mehmet S. Tumori.2005;91(2). CrossRef
- Prognostic factors for local control in patients receiving radiation therapy for early glottic cancer: anterior commissure involvement and effect of chemoradiotherapy Kitani Y, Kubota A, Furukawa M, Sato K. European archives of oto-rhino-laryngology: official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS): affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery.2016;273(4). CrossRef
- Do overall treatment time, field size, and treatment energy influence local control of T1-T2 squamous cell carcinomas of the glottic larynx? Fein DA , Lee WR , Hanlon AL , Ridge JA , Curran WJ , Coia LR . International Journal of Radiation Oncology, Biology, Physics.1996;34(4). CrossRef
- Radiation therapy in T1-T2 glottic carcinoma: influence of various treatment parameters on local control/complications Dinshaw KA , Sharma V, Agarwal JP , Ghosh S, Havaldar R. International Journal of Radiation Oncology, Biology, Physics.2000;48(3). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2023
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times