Radiotherapy for Geriatric Cancer Patients: Five-year Experience at a North Indian Tertiary Care Hospital
Download
Abstract
Background: The incidence of malignancy in elderly population in India has risen due to increased life expectancy, health awareness, and access to tertiary health care. Radiotherapy is the primary treatment modality in elderly cancer patients due to morbidity of surgery. We reviewed and analyzed clinical, disease and treatment profiles of geriatric population treated with conventional radiotherapy at our institute.
Methodology: The clinical records of patients aged 70 years or more, treated from January 2015 to December 2019 were analyzed for patient characteristics (age, sex & co-morbidities), disease characteristics (site, histology & stage) and treatment characteristics (modality & intent of treatment, radiation dose).
Results: A total of 289 patients aged 70 years and above were treated during the study period. 69% were treated with curative intent, of which, 72.4% received definitive, 24.6% received adjuvant, and 3% received neoadjuvant radiotherapy. 31% were given palliative radiotherapy. The median age was 74.6 years with male: female ratio of 4.25:1. 21.4% of the study patients had co-morbidities. 14% patients were of early stage, 57% locally advanced and 29% had metastatic disease. 51% of the study population received concurrent chemotherapy along with Radiotherapy. 87.1% of those treated with curative intent & 93.3% of patients treated with palliative intent, completed the planned radiotherapy regimen. Out of total 200 patients treated at our institute with Radiotherapy, 187 were prescribed concurrent chemotherapy, while it was exhibited to only 103 patients due to various factors like old age, poor performance status and co-morbidities.
Conclusion: Our study showed a high degree of compliance amongst geriatric patients receiving radiotherapy treatment. Toxicity rates in geriatric population were not significantly higher than the overall population treated at our centre. Various factors like disease biology and stage and patient’s performance status, co-morbidities and life expectancy affect the decision making in deciding radiotherapy intent and schedules in cancer patients of geriatric age group. Combined decision making between patients, caregivers and oncologists is crucial in geriatric age group keeping in mind above mentioned factors.
Introduction
Cancer is most important public health issue with continuously rising global burden. It is the second leading cause of death globally after cardiovascular diseases [1]. It is estimated that, by the year 2030 its global burden will rise to 26.0 million with 17.0 million deaths. Cancer has a poorer prognosis in middle and low-income countries, which is even worse in elderly [2, 3]. Age is also a high risk for developing cancer [4].
Materials and Methods
This study was conducted at the Department of Radiation Oncology at a tertiary care centre in North India. This is a single institution, retrospective, observational study, analyzing the epidemiology in elderly population with respect to the clinical profile, disease, and treatment characteristics. The study population included in this study were patients of histologically confirmed malignancies in the age group ≥70 years being treated with radiotherapy. Patients were given conventional teletherapy treatment with various fractionation schedules depending on disease site and treatment intent, on a Theratron Elite-100 Tele Cobalt machine using conventional 2D planning. The radiotherapy treatment card records from departmental database of our institute were retrospectively analyzed for patients with confirmed malignancy of any origin treated between the period from January 2015 to December 2019. The patient-related variables that were studied were age, gender, presence of comorbidities, loco-regional or metastatic status of disease and the intent of radiotherapy treatment. As the patients included were across different types of solid malignancies, instead of using specific staging, we classified them into early stage or local (disease limited to primary organ of origin), locally advanced or loco-regional (disease invading regional lymph nodes or immediate surrounding structures) and disseminated or metastatic disease. The intent of radiotherapy was divided into curative when the intent was to completely eradicate the disease and palliative when the aim was to only relive the patients symptoms. Curative radiotherapy was further divided into definitive (radiotherapy as primary modality), adjuvant (radiotherapy given after curative surgery) and neoadjuvant (radiotherapy given before curative surgery). Patients were defined as having co-morbid illness if they had pre-existing diagnoses of any one or more of diabetes mellitus (DM), hypertension (HTN), coronary artery disease (CAD), chronic obstructive pulmonary disease (COPD) or Tuberculosis (TB). The data on the percentage of patients completing the planned radiotherapy, treatment breaks if any and toxicities suffered (as per CTCAE v4) were also extracted from the treatment records.
Results
A total of 289 patients of age 70 years or more received radiotherapy at our centre during the study period. Table 1 shows the frequency distribution of various characteristics of the study population.
| Study Parameters | Range/ Parameter/Option | Number of patients | Percentage (%) |
| Age in Years | 70-79 | 249 | 86 |
| 80-89 | 37 | 13 | |
| 90-99 | 3 | 1 | |
| Gender | Male | 234 | 81 |
| Female | 55 | 19 | |
| Presence of Co morbidity | Yes | 82 | 28.40 |
| No | 207 | 71.60 | |
| Stage | Early | 41 | 14 |
| Locally Advanced | 164 | 57 | |
| Metastatic | 84 | 29 | |
| Surgery | Resectable | 65 | 22.50 |
| Unresectable | 224 | 77.50 | |
| Resectable Cases | Underwent Surgery | 54 | 83 |
| Did not undergo surgery | 11 | 17 | |
| Radiotherapy Intent | Curative | 199 | 69 |
| Palliative | 90 | 31 | |
| Modes of Curative RT | Definitive | 144 | 72.40 |
| Adjuvant | 49 | 24.60 | |
| Neoadjuvant | 6 | 3 | |
| Concurrent Chemotherapy with Radiotherapy | Yes | 147 | 51 |
| No | 142 | 49 | |
| TOTAL | 289 |
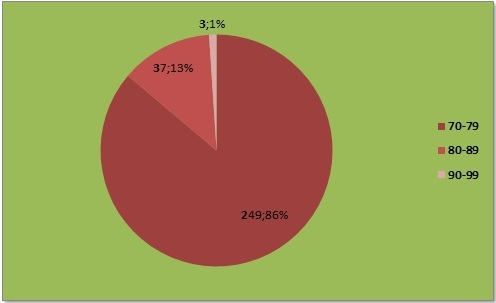
The study population was further divided into those in their 8th, 9th or 10th decade, and their respective percentages are as depicted in Figure 1.
Figure 1. Age Distribution of the Study Population.
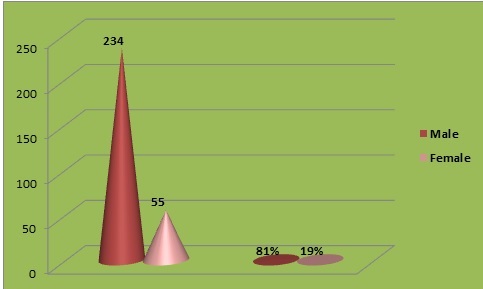
Majority of patients were male (81%) as shown in Figure 2.
Figure 2. Sex Distribution of the Study Population.
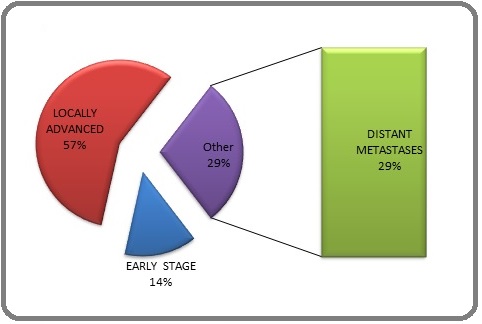
57% of the patients were locally advanced, 29% were metastatic, and 14% were early stage malignancies (Figure 3).
Figure 3. Disease Stage Distribution in the Study Population.
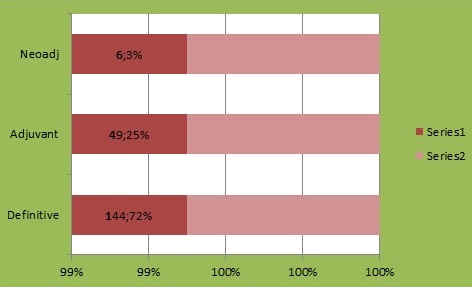
199 (69%) patients were treated with curative intent, while 90 (31%) received palliative radiotherapy for various indications. Out of those 199 patients treated with curative intent, 72% (144) received definitive radiotherapy, 25% (49) received adjuvant, while 3 % (6) patients received neoadjuvant radiotherapy (Figures 4 & 5).
Figure 4. Intent of Radiotherapy.
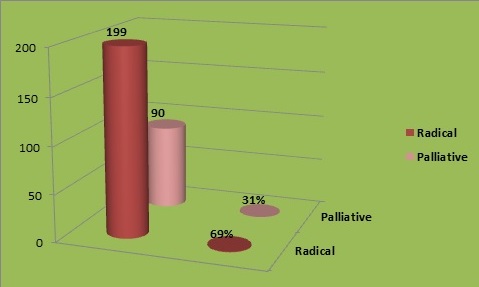
Figure 5. Types of Curative Radiotherapy.
Considering the fraction of elderly patients out of total patients treated with radiotherapy in the period January 2015 to December 2019, it was 28.5% in the year 2015, 23.5% in 2016, 24.1% in 2017, 25.5% in 2018, and 15.4% in 2019 (Figure 6).
Figure 6. Year Wise Comparison of Total Number of Patients Versus Number of Elderly Patients on Radiotherapy.

Overall, 23.2% of patients treated at our centre during the study period were of age 70 years or above. Figure 7 shows that 24% of patients were suffering from co-morbidities.
Figure 7. Presence of Comorbidity in the Study Cohort.
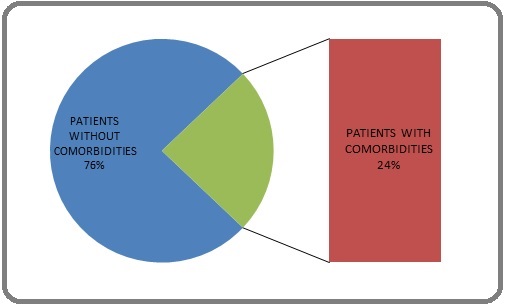
Figure 8 shows the total patients who were surgical candidates while figure 9 shows the site-wise distribution of malignancies in the study sample.
Figure 8. Surgical Resection Feasibility Status of the Patients in Study Population.

Figure 9. Site Specific Disease Distribution of the Patients in Study Population.

Out of the total 289 patients studied, 46.3% had head & neck malignancies. The commonest site was oropharynx followed by oral cavity, larynx and hypopharynx. The majority of these head and neck malignancies were squamous cell carcinomas, followed by mucoepidermoid carcinoma, melanomas & adenocarcinoma. Genitourinary cancers comprised 15.5% of the study population; commonest being adenocarcinoma prostate followed by transitional cell carcinoma urinary bladder, clear cell variant of renal carcinoma and squamous cell carcinoma of penis. The incidence of thoracic malignancies in this cohort was 10.3% among which the commonest was adenocarcinoma lung, followed by squamous cell carcinoma lung, small cell lung cancer and squamous cell carcinoma trachea. Gynecological malignancies were 7.9%, commonest being squamous cell carcinoma uterine cervix, followed by squamous cell carcinoma vulva. The percentage of gastrointestinal and hepatobiliary malignancies were 7.2%, commonest being esophageal squamous cell carcinoma, followed by adenocarcinoma stomach, adenocarcinoma rectum, squamous cell carcinoma anal canal and adenocarcinoma gall bladder. Occult primaries or CUPS (Carcinoma of Unknown Primary site) were 3.4%, commonest site of secondaries being squamous cell carcinoma in the neck, followed by adenocarcinoma in spine, poorly differentiated carcinoma in pelvis and adenocarcinoma in brain. Hematological malignancies were 2.7%; of which most common was myeloma, followed by lymphoma and leukemia. Brain tumors were 1.7% of the studied cohort, and all were Glioblastoma multiforme. Breast cancer and soft tissue sarcomas were 1.3% each. Among sarcomas, commonest was leiomyosarcoma, followed by pleomorphic sarcoma. The incidence of metachronous dual malignancy was 1% while that of synchronous dual malignancy was 0.6% in the studied population. 86.1% among those given definitive radiotherapy completed treatment. The radiotherapy treatment completion percentage was 91.8% in case of those given adjuvant radiotherapy and 83.3% in case of neoadjuvant radiotherapy. 93.3% patients were able to complete their palliative radiotherapy. as shown in Table 2.
| Treatment Modality | Total Number | Treatment Completed or Not | |
| Definitive RT | 144 | Yes | 124 |
| No | 20 | ||
| Adjuvant RT | 49 | Yes | 45 |
| No | 4 | ||
| Neoadjuvant RT | 6 | Yes | 5 |
| No | 1 | ||
| Palliative RT | 90 | Yes | 84 |
| No | 5 |
During the study period, the overall treatment completion rates for all patients at our centre were 85% for curative and 90% for palliative radiotherapy.
In our study population, 187 out of 289 (65%) patients should ideally have been recommended concurrent chemotherapy as per current guidelines. But due to various reasons like old age, co-morbidities and poor performance status, only 103 (35.6%) were exhibited concurrent chemotherapy. Only 70 (24.4%) were finally able to complete the planned concurrent chemotherapy (Table 3).
| Concurrent Chemotherapy Indicated | Given | Not Given | Completed Concurrent Chemo |
| 187 (65%) | 103 (35.6%) | 84 (29.1%) | 70 (24.4%) |
In terms of radiation-induced acute toxicity, 61% (176) of our study patients suffered grade 1or 2 toxicity and 10% (29) suffered from grade 3 or 4 toxicity respectively. Though the type of toxicity varied according to the site of treatment, the commonest acute side effects recorded were radiation-induced skin reactions and radiation mucositis. Radiation toxicities recorded in overall population during the same period at our centre were 56.5% for grade 1 and 2 and 14% for grade 3 and 4 toxicities respectively.
Discussion
Radiotherapy is an important anti-cancer modality and the treatment of choice in many malignancies, irrespective of patient’s age. Being effective against most cancers, less invasive than surgery and without requirements of anesthesia or risk of acute bleeding or death, it is often the preferred locoregional treatment for older and frail patients, and for those with poor performance status or major co-morbidities.
Radiotherapy, however, is not without it’s side-effects or toxicities. Radiation toxicity can be either early/ acute (during or within a few weeks of radiotherapy) or late/chronic (6 months or longer after radiotherapy). It can manifest in a variety of clinical signs and symptoms depending upon the irradiated region. While acute toxicities can cause an interruption in treatment leading to poorer disease control because of tumor cell repopulation, they usually resolve spontaneously in a few days/weeks. Late effects tend to persist much longer and are a significant burden on the patient’s quality of life. Whenever concurrent chemotherapy is used along with radiotherapy, the synergistic actions of these two modalities lead to a significant increase in toxicities [5-7]. These points should be borne in mind when selecting a patient for radiotherapy and also while selecting a radiotherapy regimen for a potential patient (dose, fraction size, concurrent chemotherapy).
The toxicity profile of geriatric population is similar to that of the young [7]. In-vitro studies have shown age does not have any impact on the radiosensitivity of primary human cancers cells [8-11]. However, older adults, given their likelihood of having organs which are relatively worse in function than younger adults, are presumably more vulnerable to the toxicities of radiation therapy.
While some studies have shown that the functional impairment is more in older patients treated with radiotherapy, a few other studies have had different results [12-14]. In summary, while the rate of radiotherapy toxicities maybe similar in geriatric population compared to younger individuals, these toxicities are more likely to impair completion of planned treatment in the older population.
Fatigue is the most important toxicity in older adults, to which they are highly vulnerable [15, 16], followed by mucositis, xerostomia, dehydration, infections [7], and cognitive defects [17-20].
In malignant high-grade glioma patients aged more than 65 years, age associated with poor performance status is considered anegative prognostic factor [21], and hypofractionated regimens are recommended [22]. With the advent of newer modalities, some prospective studies have shown benefit in older patients in reducing radiation toxicities [23]. In women with breast cancer with comorbid heart condition there is higher risk of cardiotoxicity after breast radiotherapy [24].
Geriatric patients also have higher prevalence of co-morbid conditions like renal, hepatic and cardiac dysfunctions, cognitive and neurological decline, which is likely to affect their ability to complete the radiation treatment [25]. The manoeuvres used in advanced radiation treatment techniques like breath-holding or abdominal compression are difficult to accomplish in older adults with frailty/ severe physical impairment [26]. Hypofractionated radiotherapy is a conservative alternative fractionation option [27-30], & is useful for palliation. It can also be used in adjuvant and definitive settings in patients with poor performance status and limited life expectancy to avoid the morbidity of acute toxicites and prolonged hospital visits.
Acute toxicities are less common in palliation of bone metastases in regimen of 8 Gy in single fraction versus 30 Gy in 10 fractions [31]. Use of concurrent chemotherapy with radiotherapy has shown to enhance toxicities and decrease survival and patients of the age of 70 and above [32]. In other studies, older adults were able to tolerate concurrent chemotherapy similarly, as compared to the younger population [33, 34]. However, these trials only included medically fit older individuals with few or no comorbidities [35]. The concurrent use of temozolomide (TMZ) and radiotherapy in glioblastoma found that older patients receiving hypofractionation and TMZ generally tolerated the combined regimen well [36]. Older adults with poorer functional status may better tolerate sequential, rather than concurrent, chemoradiation [37]. One study found that patients with nasopharyngeal carcinoma receiving sequential chemoradiation had overall less severe acute toxicities (leukopenia, anemia, mucositis, and weight loss) than those who underwent concurrent chemoradiotherapy; however, there was no significant difference in survival between the two modalities [38]. The use of more precise radiation technologies, hypofractionation, and sequential chemoradiation may benefit older individuals with poor functional status.
In our study, the rate of acute toxicities suffered by the geriatric population were similar to those reported for the overall patient population across all age groups. Similarly, the rate of geriatric patients who were able to complete planned palliative or curative radiotherapy was similar to the treatment completion rates of the general population. However, significantly fewer geriatric patients could complete planned concurrent chemotherapy than the general population.
In conclusion, with increasing life expectancies in developing countries, geriatric oncology is an emerging and important field. Active participation of patients and their families decision-making with treating oncologists for selection of appropriate treatment modality and intent is critical to obtain maximal benefit for elderly patients at minimal acceptable adverse effects. Disease biology and stage, patient’s performance status, co-morbidities and life expectancy are important considerations during such treatment decisions.
Cancer and aging are dynamic multi-dimensional processes that pose challenges to older patients and require multi-disciplinary research teams. Our study has shown that geriatric patients did not suffer a higher rate of radiation toxicities and were able to complete planned radiotherapy at a rate comparable to the general population. Use of modern treatment techniques, shorter hypofractionated schedules when appropriate and adequate supportive care measures are important in the radiotherapy of geriatric patients.
References
- State of Cancer Research Around the Globe Copur MS . Oncology (Williston Park, N.Y.).2019;33(5).
- Evidence-informed frameworks for cost-effective cancer care and prevention in low, middle, and high-income countries Chalkidou K, Marquez P, Dhillon PK , Teerawattananon Y, Anothaisintawee T, Gadelha CAG , Sullivan R. The Lancet. Oncology.2014;15(3). CrossRef
- Population-based cancer screening programmes in low-income and middle-income countries: regional consultation of the International Cancer Screening Network in India Sivaram S, Majumdar G, Perin D, Nessa A, Broeders M, Lynge E, Saraiya M, et al . The Lancet. Oncology.2018;19(2). CrossRef
- The age distribution of cancer and a multi-stage theory of carcinogenesis Armitage P, Doll R. British Journal of Cancer.1954;8(1). CrossRef
- Repopulation of cancer cells during therapy: an important cause of treatment failure Kim JJ , Tannock IF . Nature Reviews. Cancer.2005;5(7). CrossRef
- Radiobiology for the Radiologist, Lippincott Williams & Wilkins HALL EJ , Giaccia AJ . Philadelphia, PA, USA, 7th edition, 2012..
- Radiation therapy in the elderly: more side effects and complications? Gomez-Millan J. Critical Reviews in Oncology/Hematology.2009;71(1). CrossRef
- Chromosomal radiosensitivity in breast cancer patients: influence of age of onset of the disease Baeyens A, Van Den Broecke R, Makar A, Thierens H, De Ridder L, Vral A. Oncology Reports.2005;13(2).
- Effect of age on the radiation-induced repopulation in mouse lip mucosa Landuyt W, Schueren E. Strahlentherapie Und Onkologie: Organ Der Deutschen Rontgengesellschaft ... [et Al].1991;167(1).
- Radiation survival of vascular smooth muscle cells as a function of age Rosen EM , Goldberg ID , Myrick KV , Levenson SE . International Journal of Radiation Biology and Related Studies in Physics, Chemistry, and Medicine.1985;48(1). CrossRef
- In vitro radiosensitivity of primary human fibroblasts. Lack of correlation with acute radiation toxicity in patients with head and neck cancer Rudat V, Dietz A, Conradt C, Weber KJ , Flentje M. Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.1997;43(2). CrossRef
- Radiotherapy-related fatigue Jereczek-Fossa BA , Marsiglia HR , Orecchia R. Critical Reviews in Oncology/Hematology.2002;41(3). CrossRef
- Cancer-related and treatment-related fatigue Wang XS , Woodruff JF . Gynecologic Oncology.2015;136(3). CrossRef
- Subacute brain atrophy after radiation therapy for malignant brain tumor Asai A, Matsutani M, Kohno T, Nakamura O, Tanaka H, Fujimaki T, Funada N, Matsuda T, Nagata K, Takakura K. Cancer.1989;63(10). CrossRef
- Neurobehavioral sequelae of cranial irradiation in adults: a review of radiation-induced encephalopathy Crossen JR , Garwood D, Glatstein E, Neuwelt EA . Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.1994;12(3). CrossRef
- Neuropsychologic impairment in adults with brain tumors Maire JP , Coudin B, Guérin J, Caudry M. American Journal of Clinical Oncology.1987;10(2). CrossRef
- Longitudinal CT study of parenchymal brain changes in glioma survivors Stylopoulos LA , George AE , Leon MJ , Miller JD , Foo SH , Hiesiger E, Wise A. AJNR. American journal of neuroradiology.1988;9(3).
- Outpatient thyroidectomy is safe in the elderly and super-elderly Grubey JS , Raji Y, Duke WS , Terris DJ . The Laryngoscope.2018;128(1). CrossRef
- Use of systemic therapy with definitive radiotherapy for elderly patients with head and neck cancer: A National Cancer Data Base analysis Ward MC , Reddy CA , Adelstein DJ , Koyfman SA . Cancer.2016;122(22). CrossRef
- No age limit for radical radiotherapy in head and neck tumours Pignon T, Horiot JC , Van den Bogaert W, Van Glabbeke M, Scalliet P. European Journal of Cancer (Oxford, England: 1990).1996;32A(12). CrossRef
- The effect of advanced age on the efficacy of radiation therapy for early breast cancer, local prostate cancer and grade III-IV gliomas Peschel RE , Wilson L, Haffty B, Papadopoulos D, Rosenzweig K, Feltes M. International Journal of Radiation Oncology, Biology, Physics.1993;26(3). CrossRef
- Abbreviated course of radiation therapy in older patients with glioblastoma multiforme: a prospective randomized clinical trial Roa W, Brasher PMA , Bauman G, Anthes M, Bruera E, Chan A, Fisher B, et al . Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2004;22(9). CrossRef
- Glioma in the elderly Laigle-Donadey F, Delattre JY . Current Opinion in Oncology.2006;18(6). CrossRef
- Risk of ischemic heart disease in women after radiotherapy for breast cancer Darby SC , Ewertz M, McGale P, Bennet AM , Blom-Goldman U, Brønnum D, Correa C, et al . The New England Journal of Medicine.2013;368(11). CrossRef
- Hazzard’s Geriatric Medicine and Gerontology, McGraw-Hill Medical, New York, NY, USA, 6th edition, 2009 Hazzard WR , Halter JB . .
- Review of current best practice and priorities for research in radiation oncology for elderly patients with cancer: the International Society of Geriatric Oncology (SIOG) task force Kunkler IH , Audisio R, Belkacemi Y, Betz M, Gore E, Hoffe S, Kirova Y, et al . Annals of Oncology: Official Journal of the European Society for Medical Oncology.2014;25(11). CrossRef
- Prevalence of fatigue among cancer patients receiving various anticancer therapies and its impact on quality of life: a cross-sectional study Karthikeyan G, Jumnani D, Prabhu R, Manoor UK , Supe SS . Indian Journal of Palliative Care.2012;18(3). CrossRef
- Hypofractionated radiation therapy for treatment of bladder carcinoma in patients aged 90 years and more: A new paradigm to be explored? Méry B, Falk AT , Assouline A, Trone JC , Guy JB , Rivoirard R, Auberdiac P, et al . International Urology and Nephrology.2015;47(7). CrossRef
- Split-Course Accelerated Hypofractionated Radiotherapy (SCAHRT): A Safe and Effective Option for Head and Neck Cancer in the Elderly or Infirm Bledsoe TJ , Noble AR , Reddy CA , Burkey BB , Greskovich JF , Nwizu T, Adelstein DJ , Saxton JP , Koyfman SA . Anticancer Research.2016;36(3).
- Short-course radiotherapy in elderly women with breast cancer: Comparison by age, comorbidity index and toxicity Giugliano FM , Falivene S, Esposito E, Di Franco R, D'Aiuto M, Lanza F, Borzillo V, et al . International Journal of Surgery (London, England).2016;33 Suppl 1. CrossRef
- Update on the systematic review of palliative radiotherapy trials for bone metastases Chow E, Zeng L, Salvo N, Dennis K, Tsao M, Lutz S. Clinical Oncology (Royal College of Radiologists (Great Britain)).2012;24(2). CrossRef
- Increased acute mortality with chemoradiotherapy for locally advanced head and neck cancer in patients ≥70years Strom TJ , Naghavi AO , Trotti AM , Russell J, Kish JA , McCaffrey J, Otto KJ , Harrison LB , Caudell JJ . Journal of Geriatric Oncology.2017;8(1). CrossRef
- Radiotherapy with or without temozolomide in elderly patients aged ≥ 70 years with glioblastoma Metcalfe E, Karaoglanoglu O, Akyazici E. Contemporary Oncology (Poznan, Poland).2016;20(3). CrossRef
- Preoperative Chemoradiotherapy for Rectal Cancer in Patients Aged 75 Years and Older: Acute Toxicity, Compliance with Treatment, and Early Results Guimas V, Boustani J, Schipman B, Lescut N, Puyraveau M, Bosset JF , Servagi-Vernat S. Drugs & Aging.2016;33(6). CrossRef
- Concurrent systemic therapy with radiotherapy for the treatment of poor-risk patients with unresectable stage III non-small-cell lung cancer: a review of the literature Cardenal F, Nadal E, Jové M, Faivre-Finn C. Annals of Oncology: Official Journal of the European Society for Medical Oncology.2015;26(2). CrossRef
- Feasibility evaluation of hypofractionated radiotherapy with concurrent temozolomide in elderly patients with glioblastoma Uto M, Mizowaki T, Ogura K, Arakawa Y, Mineharu Y, Miyamoto S, Hiraoka M. International Journal of Clinical Oncology.2016;21(6). CrossRef
- Radical Radiotherapy for Locally Advanced Non-small Cell Lung Cancer: When Should Concurrent Chemoradiotherapy Not Be Used? De Ruysscher D, Loon J. Clinical Oncology (Royal College of Radiologists (Great Britain)).2016;28(11). CrossRef
- Induction Chemotherapy Followed by Radiotherapy versus Concurrent Chemoradiotherapy in elderly patients with nasopharyngeal carcinoma: finding from a propensity-matched analysis Zeng Q, Wang J, Lv X, Li J, Yin LJ , Xiang YQ , Guo X. BMC cancer.2016;16(1). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2023
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times